By JULIE MINDA
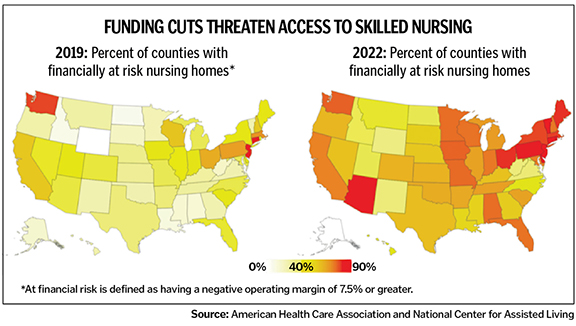
A longtime plea to state and federal government from the nation's eldercare sector is resounding again as inflation claws at a low-margin industry weakened by COVID-19: Medicaid reimbursements are so low they threaten the viability of many facilities caring for frail and impoverished patients.

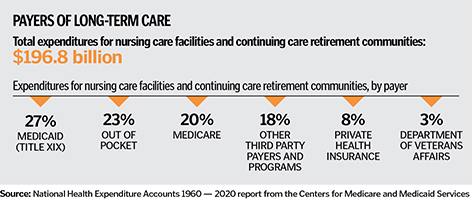
Medicare pays more than Medicaid for skilled nursing care, covering up to 100 days of care for patients after hospital stays of three or more days. Medicare, along with private pay patients, have subsidized Medicaid shortfalls in many nursing home facilities. But not all eldercare facilities can afford the décor and upgrades to attract private pay patients and Medicare reimbursements are under pressure too.
In June, 22 U.S. senators wrote to the administrator of the Centers for Medicare and Medicaid Services, decrying changes to Medicare's skilled nursing facility prospective payment system that "would result in a $320 million overall decrease in payments to long-term care facilities." CHA is a member of the nonprofit aging services advocate LeadingAge, which also opposes the payment system change. In February, CHA joined other organizations in a letter urging a continuation of a moratorium on Medicare program cuts.
In their letter, the 22 senators called out the "disastrous effect" that potential cuts in reimbursement could have on rural nursing homes that "continue to face severe workforce shortages as they deal with the aftermath of the COVID-19 pandemic."
The senators reminded CMS that 429 rural skilled nursing facilities closed between 2019 and March 2022. "When a small community loses a health care provider, there is no guarantee it will ever come back," they wrote.
Ministry eldercare executives are among those also calling for higher Medicaid reimbursement rates to shore up an essential industry.
Allison Q. Salopeck is president and chief executive of Jennings, a Garfield Heights, Ohio-based continuum of care system with four Northeast Ohio locations. Its private pay, assisted living and independent living units generate revenues that help offset the unreimbursed expenses of the organization's Medicaid skilled nuring beds — flexibility not afforded standalone nursing homes. Still, Salopeck says she worries "because of increased wages, overtime costs, agency costs, food costs, gas prices" and a host of other rising expenses.
Salopeck says inflation is affecting nearly every category of expenses in eldercare facilities and Medicaid reimbursement that has never covered the cost of care is slipping further behind. "It is an everlasting problem," she concedes.
Seesaw finances
During the worst of the pandemic, nursing homes were among the many beneficiaries of the Coronavirus Aid, Relief, and Economic Security Act enacted in March 2020. Payments to nursing homes also were included in the
March 2021 American Rescue Plan. Salopeck and other ministry eldercare executives say those funds largely have been exhausted, and now costs, particularly labor costs, are rising precipitously, without a commensurate increase in income from payers.
Salopeck says the federal aid enabled nursing homes to stay afloat, but it was a bandage, not a cure. "The government money masked problems related to increasing expenses."
Achilles' heel
Staffing issues, long an industry Achilles' heel, grew worse because of how COVID-19 impacted patient census and revenues. During the first year of the pandemic, staffing levels at nursing homes dropped due to retirements
and resignations. Patients needing rehabilitation therapy after a hospital stay steered clear of nursing homes when they could out of fear of contracting COVID. Because of staffing constraints, some facilities turned away patients, and lost revenue.

The ability to hire improved somewhat in early 2021 after the rollout of COVID vaccines, says Jerry Carley, president and chief executive of Benedictine. But the relief was short-lived. Staff numbers declined sharply in mid-2021 amid the nation's "Great Resignation."
Carley says the exodus of nursing home staff in 2021 caused a "cratering" in long-term care census and finances because many continuum of care campuses had to decrease or halt admissions — this primarily happened in skilled nursing but also to a much lesser degree in assisted and independent living. Nursing homes couldn't staff their beds.
The drop in revenue coincided with a "huge cash outflow" to pay for overtime, hiring and retention incentives and the higher salaries and fees commanded by staffing agencies to fill gaps, Carley says. Minnesota-based Benedictine operates 30-plus continuum of care communities in five states.
This year, staffing levels have been rebounding slightly, he says. He speculates this could be because of decreasing availability of government aid for the unemployed and because people's bank accounts started to be depleted.
Even so, Carley says that minimum staffing regulations for skilled nursing facilities and related fines proposed by the Biden administration feel disconnected from reality, given the ongoing staffing problems. Salopeck says that at times the regulatory environment has felt overly punitive for providers.
The Biden administration says it is working to protect patients from profiteering by private equity companies that have built a significant stake in the long-term care industry.
Uneven impact
Eldercare executives at Benedictine, Jennings, SSM Health and Trinity Health say their facilities have been able to manage through Medicare and Medicaid shortfalls, inflation and spiking labor costs at nursing homes
because they have independent living and assisted living business lines.

Carley explains that independent living and assisted living are in demand and operators have the ability to raise rates to adjust to rising costs. Campuses that have all three levels of care can subsidize the struggling parts of their operations through the revenue-producing parts. Long-term care campuses that are in systems with acute care can take similar steps.
Nursing home facilities without such flexibility are more exposed to damaging financial strain. Salopeck says a standalone, nonprofit nursing home near a Jennings campus recently went out of business. More than 90% of its residents had been insured by Medicaid.
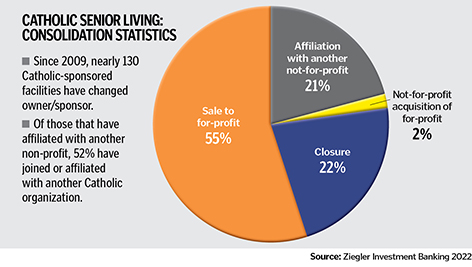
Julie Trocchio, CHA senior director of community benefit and continuing care, says while most ministry members with skilled nursing facilities also have market rate assisted living and independent living apartments and home nursing care, there are some standalone ministry facilities that are vulnerable to closing. Many Catholic nursing homes have already closed or have been acquired by for-profit investors.
Coalitions of care
Long-term care facilities are using various strategies to improve their operational capabilities and financial position over the short and long term.

Denise "D.G." Gloede is SSM Health's president of post-acute care. SSM Health has five continuum of care campuses in Wisconsin and just acquired one on the campus of SSM Health DePaul Hospital — St. Louis. Gloede says SSM Health is taking advantage of the benefits of economies of scale, standardization and quality benchmarking.

Jan Hamilton-Crawford is president and chief executive of the Trinity Health Senior Communities, which owns 32 continuum of care communities and manages an additional 15. She says Trinity Health Senior Communities is moving toward a more integrated approach to managing its eldercare campuses and consolidating management positions. Additionally, for several years Trinity Health has been adding assisted living and independent living units on some campuses and, in some cases, scaling back skilled nursing beds.
Carley says the pandemic has brought to the fore how vital it is for acute care and long-term care providers to work together. By better coordinating patients' and residents' movement through a community's health care facilities, Benedictine and its partners are aiming for better outcomes and better efficiency.
Carley says he is encouraging hospitals to join Benedictine in advocacy efforts at the federal, state and local levels. He says their support of long-term care providers' stability can hold sway with government officials who control payments.
Part of the advocacy focus for all these ministry executives is getting government reimbursement formulas to reflect the increased cost of providing care. When it comes to Medicaid — the largest payer for nursing home care — states play a deciding role in reimbursement rates. Carley notes that some states have tried to improve rates and some have not.
The providers are also calling for regulatory relief and financial support for increasing staffing.
Hamilton-Crawford says success in these efforts is crucial. "Long-term care needs to be in communities."
Panelists say action is needed now to ward off eldercare crisis (November 15, 2021)
Care communities face stiff competition to meet their workforce needs (August 15, 2021)
Long-term care providers slowly recovering from pandemic's financial hits (August 15, 2021)
CHA calls for greater reimbursement and for collaboration on staffing
Earlier this year, the Biden administration announced a collection of changes it is implementing through the Department of Health and Human Services aimed at improving the quality of care in nursing homes. Soon after, CHA sent a letter to President Joe Biden urging the administration to work closely with stakeholders in the nursing home sector in rolling out the changes.
The association said it welcomed the administration's efforts to improve the quality of nursing home care. CHA also offered suggestions around providing sustainable financing for nursing homes, strengthening the workforce and enhancing oversight through innovative partnerships.
A Feb. 28 Biden administration fact sheet says that HHS is developing and implementing the administration's reforms in an effort to "improve the safety and quality of nursing home care, hold nursing homes accountable for the care they provide, and make the quality of care and facility ownership more transparent so that potential residents and their loved ones can make informed decisions about care."
The reforms include new minimum staffing standards, requirements for staff training, monitoring of poorly performing nursing homes, reduction of reimbursements if quality is not improved and increased transparency about nursing home conditions. The fact sheet explains that the Centers for Medicare and Medicaid Services is putting in place multiple initiatives in each of these focus areas.
In the fact sheet, the White House explained a reason for the reforms is quality concerns in the long-term care sector. The administration noted that research has found that resident outcomes are significantly worse at private equity-owned nursing homes.
Biden touched upon the nursing home reforms in his March 1 State of the Union address.
In its March 23 letter, CHA applauded the administration's deep commitment to its stated intent to "improve the quality of our nursing homes so that seniors, people with disabilities, and others living in nursing homes get the reliable, high-quality care they deserve." CHA said the ministry stands ready to work with the administration "to address longstanding and systemic issues that have resulted from underinvesting in nursing home care."
In that letter, CHA said that through CMS, the federal government should increase reimbursement rates. The association also said states should be required to have Medicaid rates that fully reimburse for care.
CHA described the pressing staffing challenges long-term care facilities are facing and urged the administration "to involve provider, consumer and academic experts to work on this urgent problem."
CHA also called for continued collaboration between nursing homes and CMS, including when it comes to CMS demonstration projects on quality measurement and improvement.
-- JULIE MINDA
