By LISA EISENHAUER
Despite offering sign-on bonuses, referral bonuses and starting pay of at least $15 per hour, Avera Health is getting an underwhelming response to postings for job openings at its nursing homes, assisted living communities and rehabilitation centers across the Upper Midwest.
The message on a signboard at Hale O Meleana, an assisted living community in Honolulu that opened earlier this year, reflects labor shortages being felt in the service industry across the U.S. The St. Francis Healthcare System of Hawaii has struggled to find enough employees to fully populate the 111-bed facility.
At the D'Youville Life & Wellness Community in Lowell, Massachusetts, managers are using more temporary contract workers for aide and nursing positions, and for the first time, for housekeeping openings, until they can find permanent staffers for its skilled care and assisted living facilities that serve a primarily senior population.
In Honolulu, the St. Francis Healthcare System of Hawaii can't fully populate the 111-bed assisted living center called Hale O Meleana that it added early this year. "The need is there. The demand is there," said Jerry Correa, the system's chief executive. "The biggest issue is staffing."
The Catholic health care organizations aren't alone in their workforce challenges. A researcher with LeadingAge, the association of nonprofit providers of aging services, is hearing similar reports of employee shortages elsewhere.

Bryant
"A lot of members, like other people in aging services, are having difficulty recruiting and retaining frontline staff," said Natasha Bryant, managing director/senior research associate at the LeadingAge LTSS Center @UMass Boston that studies issues related to long-term services and supports.
Critical challenges
Last fall, an agency within the Department of Health and Human Services posted a report called "COVID-19 Intensifies Nursing Home Workforce Challenges." The report noted that operators of skilled nursing facilities have in recent years "faced critical challenges" in recruiting and retaining their workforce of 1.2 million health care personnel and support workers. The report said the pandemic has made that challenge worse.

A poster at D'Youville Life & Wellness Community in Lowell, Massachusetts, features photos of staff members and residents giving a thumbs up as part of a campaign called We've Got This! The goal was to boost spirits as the COVID-19 pandemic created new challenges for the facility and its staff.
"While many people join the field with a desire to provide compassionate, hands-on care for residents, physical and emotional demands and low wages drive high rates of turnover among direct care workers," the report says. "The onset of the COVID-19 pandemic has intensified workforce shortages to crisis conditions, putting the safety and well-being of both vulnerable residents and nursing home staff at risk."
The crisis is reflected in data from the U.S. Bureau of Labor Statistics, which have shown that health care overall is losing workers. In June, the number of people employed in the sector dropped by 7,000 from the previous month, the bureau reported. The same agency projects that the health care sector will add about 2.4 million new jobs, growing 15 percent, from 2019 to 2029.
Fewer candidates, higher wages
Executives and human resources officers confirm that the labor challenges from 2020 have carried over. They said those challenges have been intensified as the worker shortage drives up wages across the economy.

O'Brien
At D'Youville, Kathy O'Brien, director of human resources, said the rate of staff turnover this year is slightly up over last year. In April 2020 it was 2.15%, while this April it was 3.98%. Last May it was 4.55%, while this May it was 4.58%. What's different is the reasons people are leaving and the dearth of replacement candidates.
O'Brien said workers who left last spring and summer cited concerns about on-the-job exposure to the COVID-19 virus and nonwork demands, such a lack of child care services when schools closed. This year, with vaccines available and concern about the virus easing somewhat, more workers are simply accepting higher-paying positions elsewhere.

Prendergast
Naomi Prendergast, D'Youville's president and chief executive, said the competition for entry-level staff is intense. She has seen Dunkin' Donuts post signs that offer new hires $16 an hour. Leading–Age says federal statistics put the median hourly wage nationwide for nursing assistants at $13.90.
While executives report that low-skill jobs generally are the most challenging to fill, wage escalation is being seen higher up the pay scale, too. Prendergast said a social worker who left D'Youville to work for another health care provider this summer mentioned that her salary was going to jump by $20,000.
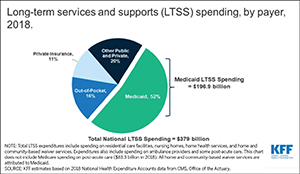
"The wages have just gone way up and it's really difficult for us to compete because our reimbursement is stagnant in that like most nursing homes we rely heavily on Medicaid and Medicare and other insurances. We simply can't just raise our rates to offset the cost of wages," Prendergast said.
Vacancies linger
Correa said that St. Francis Healthcare employs about 40 nursing aides. As of mid-July, about 15 of those positions were vacant. While the aides are typically in limited supply, the current shortage is the worst in his 10 years at the helm of the system.

Correa
On the Facebook page for Hale O Meleana, many of the posts are advertising open positions. The facility has openings for nurses, nursing aides and food service workers.
The managers of St. Anthony Nursing Home, a facility in Carroll, Iowa, that is affiliated with a hospital but not part of a larger system, offered a number of reasons they suspect nurses and nursing aides have become harder to find since the start of the pandemic.
The reasons include continued concern about medical field jobs because of COVID, greater health needs among patients than in years past because many are waiting until later in life to enter facilities, and the physical and mental toll of the work.
St. Anthony is using radio advertisements and online sites including LinkedIn and Indeed to recruit job candidates. It is offering bonuses to new hires and referral bonuses to staff who help fill openings.
Trying out new strategies
Anthony Erickson is vice president for senior services for the Sacred Heart region of Avera that includes Yankton, South Dakota. He said the nationwide labor shortage means "you've got to figure out and do whatever you can to retain any new person that comes to your door."

Erickson
Erickson said that even though there had been no cases of COVID among those being cared for at nursing centers in his region of Avera for more than six months, the pandemic has had lingering effects on hiring. While the pandemic was raging, hiring needs and processes were reassessed and recruiting was interrupted.
"We're actually just starting to go back to interviews on-site, bringing staff on board, and starting to get back to that new normal as far as how you process employees," Erickson said.
In November, Avera raised its lowest hourly wage for any worker to $15 to stay competitive with other employers. In response to the current crunch, the system is looking at other ways to ways to recruit and retain staff.
For one, Avera is exploring retention bonuses to keep its current employees from accepting outside offers. The system also is readying a pilot program called Direct Hire at its largest hospital, Avera McKennan Hospital & University Health Center in Sioux Falls, South Dakota. Under the program, a dedicated Direct Hire talent acquisition team will manage the entire hiring process for high-volume service positions including food services and housekeeping, from sourcing candidates to making the hire and assisting in onboarding.

Miller
Jane Miller, the lead human resources officer for two Avera regions, said the goal of Direct Hire is to reduce the number of management hours devoted to interviews and to give hiring managers more time to work with their staffs.
"We're aware that another system is doing it and they've had great successes with it," Miller said. "The leaders really appreciate the time that they can round now with their employees."
Avera operates its own temp agency, Avera Education & Staffing Solutions, through which it deploys temporary workers across its own system and contracts for them with other employers. Even so, the system taps outside agencies to fill some openings. Through one of those agencies, Avera hires nurses from the Philippines for temporary assignments. Some of those nurses have stayed on permanently.
'Infused enthusiasm'
D'Youville is looking at creative new strategies to recruit workers. The senior leaders have started a strategic initiative to work with department leaders to ensure that job applicants receive a quick response. It also is reviewing its interviewing process to make sure managers know how to recruit prospective hires.

Hailey Gukeisen, a certified nursing assistant at Avera Brady Health and Rehabilitation in Mitchell, South Dakota, visits with resident Genevieve Gray. Gukeisen has been a CNA at the facility for about one year.
"It's really the role of anybody doing an interview to infuse enthusiasm in job candidates about why D'Youville really is the place they want to work," Prendergast said.
"We actively talk about how our mission of compassionate care is not just about how we treat those we care for but about how we treat each other," Prendergast said. "We actively work on the culture here."
O'Brien said the system also has sent direct mail appeals to former employees to see if they are interested in returning and to applicants who turned down job offers to see if they are in the candidate pool again.
Flexibility and gratitude
Representatives of several systems said they are or are planning to collaborate with local colleges and universities to better align their need for workers with education programs. Correa said St. Francis Healthcare hopes a collaboration it has in the works will create career pathways for entry-level workers that enable and encourage them to get the education and credentials required for higher-paying positions in nursing and social work.
While that partnership with local colleges is taking shape, Correa said that his system is being especially attentive to the personal needs of its 250-member workforce. The system is offering flexible schedules and holding events to thank workers for their service.
Correa said he and other managers at St. Francis are aware that competitive wages are just one of the factors that attract workers and build loyalty. "It's being able to spend time with family," he said. "It's their work-life balance. It could be things like recognition."
As to how to fill the system's many openings, Correa said he welcomes new ideas. "I'm all ears if there's different ways of recruiting," he said. "I'd love to find out and see how other people are being successful at it."
LeadingAge report suggests how to stabilize direct care workforce
 A report called "Feeling Valued Because They Are Valued" that was released in July by LeadingAge says that to ensure that the nation's direct care workforce can meet the growing needs of an aging population those workers need competency-based training, living wages and benefits, and career-development opportunities.
A report called "Feeling Valued Because They Are Valued" that was released in July by LeadingAge says that to ensure that the nation's direct care workforce can meet the growing needs of an aging population those workers need competency-based training, living wages and benefits, and career-development opportunities.
The report is subtitled "A Vision for Professionalizing the Caregiving Workforce in the Field of Long-Term Services and Supports." It was written by Natasha Bryant, managing director/senior research associate at the LeadingAge LTSS Center @UMass Boston, and her colleague Robyn I. Stone.
Bryant said the challenges of hiring and retaining direct care staffers — nursing assistants, personal care aides and home health aides — preceded the COVID-19 pandemic but were exacerbated by it.
"The frontline staff certainly do not receive high wages. They don't always get the supervision and the training that they need to do complex jobs," Bryant said. "They don't have career advancement opportunities, so it can be difficult to get people to come into these jobs, let alone stay in these jobs."
The report says the median hourly wage for direct care workers — home care aides, home health aides, nursing assistants, and certified nursing assistants — is $12.80, up only 19 cents over the last decade; median annual earnings for the workers is $20,300, in part because many are employed part time; and 15% of the workers do not have health insurance while 36% receive health insurance through Medicaid, Medicare, or other public coverage.
To stabilize the workforce, the report offers several suggestions:
- Expand the pipeline of potential caregivers by recruiting nontraditional workers, such as high school students or those who have been displaced from other fields, and foreign-born workers.
- Enhance education and training so professional caregivers will feel well prepared to carry out increasingly complex care tasks, and so nursing homes, assisted living communities, home care organizations, consumers, and their families will have confidence in those caregivers.
- Facilitate career advancement so caregivers can advance in careers in long-term services and support that offer them a variety of opportunities.
- Increase compensation so direct care professionals can earn a wage that covers basic living expenses such as housing and food.
- Train "universal workers" on a core set of competencies set at the federal level. These workers would then have the flexibility to work across settings and even across state boundaries.
- Reform the financing system, which now is largely reliant on Medicaid, by using insurance-based dollars to provide additional and more consistent funding.
"I think we as a sector need to create jobs that people want and that at the end of the day is what we have to do," Bryant said.
— LISA EISENHAUER