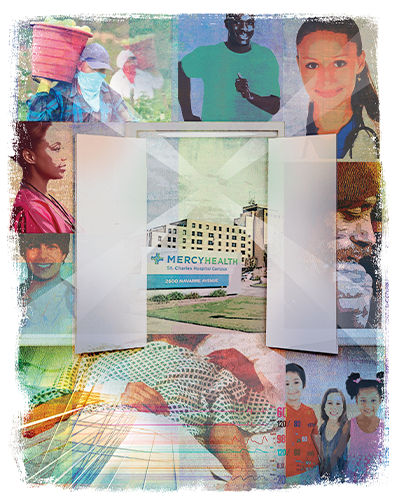
Mission Ambassador at Mercy Health — St. Charles Hospital
A man was brought into the emergency room at Mercy Health — St. Charles Hospital in Oregon, Ohio, suffering from hyperglycemia. He had rapid breathing, confusion, excess sugar in his urine and heart palpitations, and was admitted to the ICU. A migrant worker who came to Ohio to help harvest crops, he had run out of insulin and had no financial means to obtain the medication.
The patient later improved and was transferred to a medical unit until he recovered. He returned to his temporary living situation with medicine from the hospital's Mercy Health-funded medication outreach program — which provides an initial dose of medication for qualified people who cannot afford it when they are discharged from the hospital — and was supplied with enough to last until he could acquire his own. A hospital community outreach worker conducted a follow-up visit to determine if he had any further health care needs.
What does it mean to "open doors" to improve access, particularly for those most in need?
It requires health systems to be attentive to the complex needs of our patients beyond the time they are in the hospital. This migrant worker's difficult situation served as a case study for Mercy Health executives, hospital administration, mission leaders, outreach workers and emergency personnel about three decades ago to determine creative ways to prevent a similar situation in the future. Out of these discussions, the Mercy Health mobile health van program was launched.
The mobile health van program included the purchase of a 40-foot van that became a clinic on wheels, primarily serving Northwest Ohio. Some participants train to drive the van, and community health nurses and patient care technicians deliver the services needed.
Launching a mobile health van program required raising funds to pay for program costs. Members of Mercy Health Foundation — Greater Toledo took up the challenge and raised funds to purchase the van. Community members understood the need and wanted to be involved in making a difference. Thirty years later, the program continues to help meet the needs of the underserved by going out to where they are located.
Recently, a young woman waited for an opportunity to be seen by one of the mobile van program's volunteer doctors. As she walked out of the exam room with reassurance and resolution of her issues, she had a wide grin on her face and said, "God bless you" to the mobile van staff.
EXPANDING THE VISION OF CARE
Opening doors to health care access for those who are poor and underserved requires developing a vision of what the care can look like. Health care is no longer focused solely on the patient, but also
attends to the overall health of the community.1 Often, it is difficult to know how to begin. The county community health needs assessment (CHNA) is a good place to start.
For the purpose of the CHNA, Mercy Health — Toledo used Lucas County as the main service area. The most recent Lucas County CHNA was conducted in 2019/2020 by Healthy Lucas County, a coalition of hospitals and community agencies that work together to improve county residents' health through a strategic planning process. The poverty rate in Lucas County is nearly 20%, with 13% of adults on Medicaid or other assistance.2 Per the CHNA, 17% of adults described their health as fair or poor, increasing to 34% for those with annual household incomes less than $25,000.3
The mobile health van program expanded its outreach based on the Lucas County CHNA. It increased its collaboration with other community agencies, including schools, senior centers, 1Matter's Tent City project,4 African American Male Wellness Walk and community health events. Health screenings are conducted and abnormal ranges identified. Participants receive results they can share with their physicians, or, for those who don't have one, help is provided to assist them with finding a primary care provider.
A PATH TO COMPASSIONATE CARE
While we need data to identify the greatest health needs, how we respond is based on the ministry's mission to provide compassionate care. In my experience, I believe the following elements help to make
opening doors for the poor successful.
A Passion to Serve
First, a person needs to have a passion for serving the poor, a passion that follows in the footsteps of Jesus. Jesus went to the poor and marginalized to offer them healing and comfort. He told the story of the
Good Samaritan when he was asked, "Who is my neighbor?" The answer to that question guides us on how we should respond to the needs of the poor.
Second, a passion for the poor follows in the footsteps of the founders of our religious congregations who started our healing ministry. Catherine McAuley, the founder of the Sisters of Mercy, walked the streets of Ireland caring for the poor and sick during the cholera epidemic in the early 1830s. The sisters treated the poor respectfully by keeping them warm, fed, clean and comforted. Their presence not only alleviated this situation, but, at a time when nursing was not a recognized profession, it so improved the quality of care of the patients that the death rate was one of the lowest on record.5 Additionally, Pope Francis encourages his bishops to be shepherds who smell like their sheep. By "tending sheep," this means one welcomes, walks and stays with those in their care.6
Serving the poor continues as a priority in our actions today. An internal medicine physician told me a story of a difficult case he had. The patient was an insulin-dependent diabetic and had trouble staying on his regimen. He often came into the office with an infection at the site of the injections. A social worker suggested it might be helpful if the physician visited the patient at home to see what could be the barrier to compliance. The physician agreed and discovered upon a visit that the patient did not have hot water in his apartment. The physician now understood the reason for the patient's infections. He realized it was not a compliance matter, but a socioeconomic issue. He switched his medication to an oral one instead, resulting in improved patient outcomes. The patient was connected with other community resources by the social worker. Today, socioeconomic conditions are part of the assessment of each patient during their medical appointment, and the information is integrated into their health chart.
Show Leadership's Commitment
Third, leadership needs to be involved in developing the priorities for serving the poor — it is not only the responsibility of the frontline workers. A positive shift in organizational commitment
occurs when strategies and goals are aligned. For example, a young mom arrives late for her doctor's appointment after riding the bus on a rainy day. Can frontline workers fit her into the schedule, or do they have to send her home per policy? Examining
policies and procedures is an important element of care for the poor to see how protocols impact vulnerable persons.
Leadership needs to be committed to making a difference in the community. Basic justice demands the "establishment of minimum levels of participation in the life of the human community."7 Aligning internal targets with the results of the CHNA provides better outcomes for the community. Engaging the board of trustees in an immersion experience is one way to increase the knowledge of board members to the struggles of the poor. It is also a way for the board to understand the significant contribution of the health system to make a positive difference.
Support Community Professionals and Training
Fourth, acknowledge the special skills needed to work with the poor to improve their health. Addressing poverty is everybody's business in a community. By addressing poverty, better health
outcomes can result. Training hospital employees increases the ability of staff to connect with the poor. One approach, Bridges Out of Poverty, is a training program that shifts the way we understand and approach poverty. It shifts seeing individuals
as strong, not wrong, and brings people of all different classes to the same table to increase sustainability.8
One group of professionals who can be highly valuable in improving care access for underserved individuals are community health workers. As trained professionals who provide resources and information to individuals who are in poverty, community health workers often come from the same neighborhoods and understand the challenges many people face. The Toledo campus of Mercy College of Ohio offers a training program to become a community health worker, which includes interactive experiences in a variety of community settings, and, upon program completion, a certificate from the Ohio Board of Nursing.
I have witnessed the commitment and dedication of community health workers to help people of all ages, and how their incorporation into ongoing community outreach efforts — like serving as navigators for persons entering the federal health care exchange insurance program — can help individuals overcome complex barriers to meet their health care needs.
Community Collaboration
Fifth, collaboration is essential to long-term success. An example of collaboration in action is CareNet, founded in 2002, which provides access to coordinated health care services for low-income Lucas County
residents. In 2002, then Toledo Mayor Jack Ford challenged the health care systems to work together to provide better access to care. Today, through CareNet, all the local health care systems, local government, health department and other agencies
work together to provide care. Licensed and certified navigators provide help to enroll individuals in Medicaid and the federal health insurance marketplace. To date, CareNet has helped approximately 29,000 low-income residents of Lucas County to
get access to coordinated health care services.9
Through collaborative efforts like CareNet, I am reminded how Jesus was able to break down barriers and get his apostles and disciples to work together to help others in need.
Experience Joy in Helping Others
Sixth, enjoy the ministry and serve with joy. The ministry is challenging and rewarding. Rewards come in the way of connecting with people and seeing their health improve. Catherine McAuley said our
lives need to be centered on God, and that we need to take one small step today and strive to do better tomorrow. She also cared for her sisters and provided them moments of respite, including finding a relaxing place by the sea for them to renew
their spirit.10 Paying attention to the needs of our team members gives them an opportunity to experience what provides wellness for them so they can translate similar experiences to those in need.
The Getting Healthy Zone project in Toledo is an example of taking one small daily step and doing better tomorrow. Beginning in August 2018, concerned about the high infant mortality rate in the community, Mercy Health engaged residents to come together to share their insights and experiences. Through these conversations, a plan was developed to support residents to address the social determinants of health and structural racism.
Today, through Getting Healthy Zone, neighborhood goals link residents with resources to increase infant vitality, connect residents with living wage jobs, assist them with credit repair and home ownership, help entrepreneurs with needed support, and provide community members with a space for outdoor recreation through the creation of a usable park.
Today, the Getting Healthy Zone project is seeing results. In 2018, 12% of the infants who died prior to the age of 1 were in three Lucas County zip codes. By 2022, that number decreased to 5%.11 Getting Healthy Zone's motto is "Everyone can be a superhero to help prevent poor birth outcomes." There are currently 25 agencies working together to make this progress become sustainable.
RESPONDING TO OUR CALL TO SERVE
Each of us is called to reach out to those in need. When one is sick, one is in need. A focus on the health of the poor is a special calling, one that I might suggest could lead those called to serve
in a new role as mission ambassadors. I began the role of mission ambassador volunteer when I retired from my role as vice president of mission for the Mercy Health — Toledo region in 2022. My role as mission ambassador is to be the face of
the ministry to the community. In the future, I envision more people will desire to be a mission ambassador. Qualifications for this role include someone who knows community health or patient care, has worked for the health system for many years,
is willing to serve as a volunteer and can meet with diverse groups of people. The role expands the strategic direction of the hospital and draws from the mission to aid those in need.
Responding with compassion brings comfort and healing to the person in poverty as well as to the one being the helper. When we look at the needs of a person from their perspective, we walk in the shoes of God, who loves each person — it gives us an opportunity to love as Jesus did. The image of Jesus as the Good Shepherd from his parable of the lost sheep can be an inspiration. As a Good Shepherd, Jesus left the 99 sheep and went after the one lost sheep until he found it. (Luke 15:4-7) We can trust that God will be with us along the way and carry us forward in our ministry of health care.
SR. DOROTHY THUM, RSM, is mission ambassador volunteer at Mercy Health — St. Charles Hospital in Oregon, Ohio. She retired in 2022 after serving 40 years at Mercy Health — Toledo, including her last role as vice president of mission for the Toledo market.
NOTES
- Cardinal Joseph Bernardin, A Sign of Hope: A Pastoral Letter on Healthcare (St. Louis: Catholic Health Association, 1995), 8.
- "2019/2020 Lucas County Community Health Assessment," Healthy Lucas County, December 8, 2020, https://www.healthylucascounty.org/wp-content/uploads/sites/2/2020/11/2019-2020-Lucas-County-Community-Health-Assessment.pdf.
- "2019/2020 Lucas County Community Health Assessment," Healthy Lucas County.
- 1Matters, https://www.1matters.org.
- M. Joanna Regan, RSM, and Isabelle Keiss, RSM, Tender Courage: A Reflection on the Life and Spirit of Catherine McAuley, First Sister of Mercy (Chicago:
Franciscan Herald Press, 1988), 85. - Pope Francis, The Church of Mercy: A Vision for the Church (Chicago: Loyola Press, 2014), 85.
- Economic Justice for All: Pastoral Letter on Catholic Social Teaching and the U.S. Economy (National Conference of Catholic Bishops, 1997), 44.
- "Bridges Out of Poverty," aha! Process, Inc., https://www.ahaprocess.com/our-services/#tab-a51176197740d672e83.
- Care Net Toledo/Lucas County, https://www.toledocarenet.org.
- Mary C. Sullivan, ed., The Correspondence of Catherine McAuley, 1818-1841 (Washington, DC: The Catholic University of America Press, 2004), 136.
- "Getting Healthy Zone Report to the Community," Mercy Health, 2022, https://www.mercy.com/-/media/mercy/about-us/community-benefit/ghz-report-to-community-2022.ashx.
