BY: FR. CHARLES BOUCHARD, OP, STD
 If you watched the AMC series "Mad Men," you saw the dramatic shift that took place in American business culture — specifically advertising — in the 1960s. In a just a few years, corporate life passed from starched collars, suits, lots of cigarettes and liquor to something quite different. Health care experienced a similar cultural shift as medical paternalism gave way to collaboration, teamwork and patient autonomy. Motherhouse properties were alienated to corporations, a family business model became professionalized,1 and waves of mergers and acquisitions almost eliminated the stand-alone hospital. Medical specialization, government funding and technology brought even more drastic changes.
If you watched the AMC series "Mad Men," you saw the dramatic shift that took place in American business culture — specifically advertising — in the 1960s. In a just a few years, corporate life passed from starched collars, suits, lots of cigarettes and liquor to something quite different. Health care experienced a similar cultural shift as medical paternalism gave way to collaboration, teamwork and patient autonomy. Motherhouse properties were alienated to corporations, a family business model became professionalized,1 and waves of mergers and acquisitions almost eliminated the stand-alone hospital. Medical specialization, government funding and technology brought even more drastic changes.
The changes were not just technological or cultural. There were huge changes within the church as well. When Pope John XXIII was elected in 1958, most people thought he was an affable Italian uncle who would be a caretaker. No one imagined that he would convene the Second Vatican Council, which would be the largest, the longest, the most prolific and probably the most influential in church history.
VATICAN IIThere were certainly substantive theological changes that resulted from Vatican II, but church historian John O'Malley, SJ, maintained that the biggest innovation of the council was how it said what it said, its style: "Style — no other aspect of Vatican II sets it off so impressively from all previous councils and thereby suggests its break with 'business as usual.'''2 Documents from previous councils had been short, polemical and confrontational. They often involved condemnation of erroneous or heretical positions. By contrast, the documents of Vatican II had a narrative style, an invitational and collaborative tone and a dialogical language. To a large extent, the church redefined itself by speaking as a mother, a friend and a shepherd rather than as an authoritarian voice from on high.
What did Catholic health care leaders think at the time? How did they think Vatican II would change their world? To find out, I reviewed dozens of articles in Hospital Progress written between 1966 and 1972 (the journal's name changed to Health Progress in 1984). None of the writers understood fully how dramatic the changes would be, but I found several recurrent themes, as well as some truly visionary ideas that contained the seeds of Catholic health care as we know it today.
Here is how writers thought we were emerging from isolation, incorporating laity, rethinking the role and identity of religious, providing theological depth to our mission, forming leaders, and laying the groundwork for the discipline of health care ethics.
EMERGING FROM ISOLATIONUntil the 1960s, Catholic health care consisted mainly of stand-alone hospitals, so part of the change was reducing the isolation among the hospitals themselves. "The days of isolation are past," wrote Mother Mary Regina Cunningham, RSM, mother general of the Sisters of Mercy, in 1965. "Gone too are the independent health care organizations."3
In an address to the Catholic Hospital Association Convention in 1966, Archbishop William Cousins of Milwaukee addressed this idea in ecclesial terms that reflected a move from the immigrant parochial church that was familiar at the time. He suggested the broader mission of a universal church that would shape Catholic health care's understanding of itself:
You are not working just for your own hospital. You are working for Christ primarily with your dedication and loyalty to the hospital. You represent more than you realize: Catholic thought, Catholic training, Catholic ethics and Catholic idealism … This is not something local. Christ did not save souls just in this town or in that community. He died for all men. Your service is for all.4
In 1967, Lawrence Hoban of St. Mary's Help Hospital in San Francisco reflected on organizational changes that would flow from this new identity. Using a term that is often used to describe the dynamic of the council itself, he said "the authority of … the Catholic hospital will need complete aggiornamento," that is, bringing up to date. His article included schematic diagrams of the relationships Catholic health care had in the past, those that existed in 1966, and those that would surely develop in the future. His diagrams reflected the transition from an in-house operation with the motherhouse at the top to one with lines of accountability to other systems, to the bishops and to the government. He proposed creation of a "National Catholic Institute of Health" under the direction of the Conference of Major Superiors to create a stronger Catholic presence, less competition and more efficiency. 5
ROLES EVOLVEThe council's use of the phrase "people of God" to describe the church was one of its most distinctive and important contributions. It helped us see that the church was more than the hierarchy, and it raised questions about the future role of the laity. Like many others, Hoban saw an increased role of the laity, but his hopes were modest. Indeed, he only went so far as to say that "participation by laypeople on boards of directors seems inevitable."6 Others worried about what would happen to women and men religious as more laypeople became involved. In her 1966 address to the CHA Convention, Mother Vincentia Steffens, OSF, of the Maryville, Missouri, Franciscans, cautiously described the future this way:
It is expedient to introduce dedicated and devoted laymen into the hospital family in order to guarantee efficient and effective management and administration. Laymen have much to offer in administration positions in our hospitals today. … I am in no way advocating that sisters' hospitals be taken over by laymen, nor do I mean that gradually all the key positions in the hospital be filled by laymen. And on the other hand, I do not mean to imply to the layman that he or she is just a poor substitute for the sister. … It is because of their professional competency and their zeal for corporal and spiritual works of mercy that sisters should feel free to welcome laymen to help them meet their responsibilities in the care of the sick.7
She also addressed a worry that the religious would be diminished by the presence of these competent laypeople. Note her use of "people of God" and the early acknowledgement of a broader range of charisms than it was common to think of at the time.
We will not lose the identity, the status or prestige, which is uniquely ours by means of our religious profession. We must make an earnest effort to accept our lay brothers and sisters and show them how they can help us in our work, which is not limited to religious alone, but a work in which all the people of God must engage according [to] their state of life, their calling and their talents."8 [Italics added.]
Daughter of Charity Bernadette Armiger, who chaired the Department of Nursing at St. John's University in New York, saw the theological implications of this new view of church: "What is the place of the layman in the Catholic hospital? Should he assume a leadership role if qualified by his education, experience and talents? Why do we exclude him from full participation?"
She astutely said that the "outmoded attitude that laypeople work for the religious group which conducts the hospital must be replaced with the conviction and appreciation of the layman as co-worker in the magnificent apostolate to the sick. We will want these laypeople to be co-responsible for the philosophy and policy of the hospital," for they are "not merely members of the Church," they "are the Church."9 Her words may not sound very revolutionary to us, but in 1966 they were a bold statement that reflected a clear grasp of the fundamental changes brought about by the council. She was perhaps the first to suggest lay responsibility for anything resembling sponsorship, a term which did not even exist at the time.
This acknowledgement of lay competence and the increased demands for professionalism brought about by the move into the bigger world of health care raised questions about the competence of the sisters. Sr. Armiger was candid about this when she said "Every sister does not have the leadership potential which management positions entail. Religious obedience supplies motivation, not competence. We are symbols, it is true, by our veils and holy habits but we eschew the use of them to cloak incompetence and mediocrity."10 So the council's view of the church as the people of God was a double-edged sword. It empowered the laity and prompted a self-assessment by religious.
FROM APOSTOLATE TO MINISTRYPrior to the council, health care had been seen mainly as a corporal work of mercy, a charitable human response to suffering of the poor. After 1965, renewed theology and changing economic circumstances prompted questions about whether there was something more. Several writers noted that with the changes in funding, there might not be any poor to care for in the future.
"There are those, of course, who maintain that since Catholic hospitals came into existence to care for the sick poor, and since this need has changed somewhat, we are no longer needed and should withdraw from the contemporary hospital scene," said Sr. Margaret Vincent Blandford, SCN, hospital consultant for the Sisters of Charity of Nazareth, in 1966. She quickly added that even though an outside agency may pay the bills, it will never be able to "satisfy the needs of his soul." But, she said, "If our hospitals are really continuing the work of Christ, we shall be able to satisfy that need."11
Jesuit Fr. Trafford Maher was director of the Human Relations Center for Training and Research at Saint Louis University and wrote extensively on organizational development in health care. He expressed the ecclesial dimension of health care clearly: "What is the unique character of the Catholic hospital? It is a health agency that gives an enduring, official and formally professed witness to the reality of God, the presence and redemptive work of Christ, and the dignity and worth of man."12
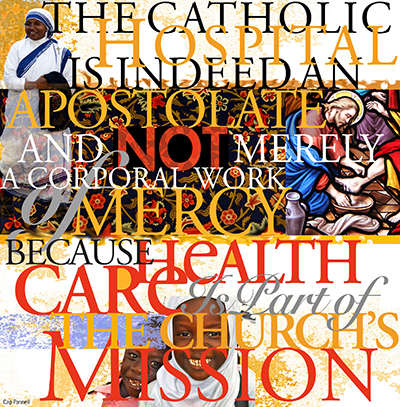
Walter Burghardt, SJ, who in 1971 was a professor at Woodstock College in New York City, went further. "Your apostolate is ecclesial," he wrote, "because what you touch is man, man-in-process-of-redemption [that is, not just man-as-a-suffering-human] … the Catholic Hospital Association is indeed an ecclesial apostolate [and not merely a corporal work of mercy]. Why? Because health care is part of the Church's mission; sickness calls for the Church's service."13
In 1967, a CHA task force on the future of Catholic health care facilities cited a challenge regarding "the mission of the Church" in health care which remains with us today. "This challenge presents several identity problems for the hospital — with the Church, the religious community and the people of God … this challenge requires more effective communication with … the hierarchy," and "a clearer understanding of the interrelationship between institutional service and personal witness."14
These ideas were the beginning of a new theology of health care (a term that did not even exist at the time) that was not rooted primarily in the corporal works of mercy (taking care of bodily needs) but in the work of the apostles, preaching the Gospel through care of the sick.
Not a single writer used the word "ministry" to describe health care, but the shift from a "corporal work" to an "apostolate" was an important step in that direction. Even though apostolate was understood to be the work of the laity in the world (and not the sacramental and ministerial work of the ordained), this emphasis on apostolate was the foundation of our contemporary understanding of health care as a ministry.
ADMINISTRATION AS APOSTOLATESeeing health care as an apostolate raised questions about administration, which apparently had been seen more as a business function than as real ecclesial work. Fr. Paul Reinert, the revered Jesuit president of Saint Louis University asked bluntly, "Is the role of an administrator of apostolic value? Is the personal, face-to-face relationship between religious and patient or between religious and poor people in the 'inner city' more important and of greater value than the position of chief executive of a hospital?"15 "Is it impossible for a religious man or woman to find vocational satisfaction in a management position?" Is it just a "cold, sterile position?"16
Fr. Edward J. Stokes, SJ, professor of Canon Law at St. Mary of the Lake Seminary in Mundelein, Illinois, raised a similar concern as he discussed the lack of integration between religious life and hospital administration. He cited James Hayes, dean of the School of Business Administration at Duquesne University in Pittsburgh, who tentatively and awkwardly proposed that administration might in some strange way be a vocation or a mission: "I believe that the spiritual health, the effectiveness and the example of any community can be improved if an understanding of the management task and effective administration can be expressed as an unusual aspect of a vocation. Is it not possible that this skill could be recognized as a peculiar kind of mission within the community?"17
THE NEED FOR FORMATIONToday we take the ministerial dimension of administration and leadership for granted. Early questions about the apostolic quality of administration, and of health care itself, laid the foundation for what we would later call "formation," which would be distinct from ongoing professional education.
Part of the self-assessment that religious entered into as a result of Vatican II pointed to the need for better religious formation for sisters. It also called into question the dichotomy that existed between the "work" of health care and the spirituality of the religious. Fr. Stokes asked, "Should the administrator think of the work in the hospital apostolate as first, a series of spiritual exercises, and after that, work on the floor, in the office, going about various medical meetings and then back to prayer to rekindle the spirit? ... Should there not be a greater integration between the two, especially if sisters began to see prayer as so discrete that it was an interruption in their work?"18
If the church is the "people of God" and if this bestowed a basic equality on all, whether religious or lay, then should greater holiness and better formation be a concern for all? Again, no writer used the word "formation" with regard to laypeople, but they were certainly beginning to think along those lines as it became clear that many more qualified laypeople would be required to lead Catholic health care into the future.
Fr. Stokes noted that religious profession alone was not enough for the needs of tomorrow's Catholic hospital. "It is not a question of installing some saintly soul in the office of administrator, on whatever level it might be, but of sanctifying the present well-qualified incumbent in the office," he said.19 Foreshadowing the contemporary discussion about "intentional discipleship" in the church, Fr. Maher noted that knowing about theology wasn't enough. Rather, he said,
Each individual must internalize the central Christian truth that we are possessors of the Spirit, then messengers and 'Christophers' [i.e., bearers] of the Spirit. Mere theological knowledge is no substitute for an individual if he is to be a true person. He must have internalized an awareness of, a feeling for, and a habitual readiness to act on the truth of our deeply personal relationship with God.20
Fr. Maher asked how long it would take to provide this kind of formation. He was referring to religious, but it is clear from what he says elsewhere that he was beginning to think of laypeople too.
"Properly trained," he said, "the formed religious person's first, fundamental and enduring impulse will be to respond, to fulfill and to transcend his individual personality by entering in relational, committed union with God himself, the world, and men."
Contemporary definitions of formation used by various health systems contain some of the same elements.21
MORAL AUTHORITY LOCUS SHIFTSPerhaps the most important change of all was the shift away from a vertical and hierarchical understanding of moral authority. Prior to Vatican II, the laity were largely in a passive relationship to moral truth and the teaching office of the church: the church taught, Catholics obeyed. Vatican II, both in tone and in explicit statement, changed that by emphasizing freedom of conscience, moral discernment, dialogue and responsibility.
In this view, church authority assists conscience but does not replace it. We discover moral truth through reflection and prayer. Fr. Maher picked up on this theme as he commented about the requirements for what we would today call formation:
To train the adequate person for the modern apostolate and its demands … we need a new orientation concerning the individual and his freedom, for it is only the free individual who can be a full person, a truly adequate person, a unique image of God. A person is free only when he takes the personal initiative … Any other state leads to mere conformity which is a kind of death state. … At first this may appear paradoxical for a religious who is to spend his life dependent upon authority. Paradox though it may be, it is in no sense a contradiction.22
This shift from an external to an internal source of moral authority had important implications. First, by emphasizing moral freedom and responsibility, it created the conditions for patient autonomy and a state of informed consent. It invited patients to consider and reflect upon moral principles and how they could be concretely realized in their lives rather than having decisions made for them by others. It also laid the groundwork for the discipline of health care ethics, which uses both clinical evidence and patient experience to inform decision-making.
This brief exploration provides an interesting picture of Catholic health care thinking its way through an unprecedented period of change. It shows adaptability and innovation that should encourage us as we face the challenges of the future.
FR. CHARLES BOUCHARD, OP, is senior director, theology and ethics, the Catholic Health Association, St. Louis.
NOTES
- Edward J. Stokes, "Integration of Religious Life and Hospital Administration," Hospital Progress 44, no. 6 (June 1963): 91-158. Also see Lawrence Hoban "Can … Should … Will Catholic Hospitals Be Partners in the Emerging Health Network? Part 1. Problems Facing Catholic Hospitals," Hospital Progress 48, no. 7 (July 1967): 71. Hoban quotes Fr. Andrew Greeley describing the shift from the familial structure of religious life that stressed integration to a more businesslike model that stressed achievement.
- John O'Malley, "The Style of Vatican II," America (Feb. 24, 2003): 12. O'Malley identifies the council's horizontal orientation, its focus on serving rather than controlling, use of words like "development" and "progress," use of an inclusionary rather than an exclusionary vocabulary and shift from passive acceptance to participation and engagement as stylistic hallmarks of the documents of Vatican II.
- Mary Regina Cunningham, "Impact of Change on the Religious Hospital Apostolate," Hospital Progress 46, no. 6 (June 1965): 112.
- "A Head Start toward Unity," Hospital Progress, 47, no. 10 (October 1966): 109.
- Hoban, "Part 1. Problems Facing Catholic Hospitals," 64-71, 98. Also see Hoban, "Can … Should … Will Catholic Hospitals Be Partners in the Emerging Health Network? Part 2. Reorganization of Catholic Health Services," Hospital Progress, 48, no. 8 (August 1967): 103-107, 140.
- Hoban, "Part 1. Problems Facing Catholic Hospitals," 71.
- M. Vincentia Steffens, "Expectation and Role of Religious," Hospital Progress 47, no. 9 (September 1966): 145. Robert Hoyt, then editor of The National Catholic Reporter, wrote a companion piece in the same issue: "The Expectation and Role of the Layman," 138-43. Also see John Flanagan, "What Is the Catholic Hospital Apostolate?" Hospital Progress, 47, no. 3 (March 1966): 49-51. Flanagan, then executive director of CHA, asked whether there was a need for Catholic hospitals today, whether religious should be engaged in hospital work, especially finance and administration, and whether there would be any poor to care for after Medicare, insurance and Blue Cross. In a later article, he described what it means to be "apostolic," and suggested that we develop new committees to assure the "catholicity of the hospital" ["Reaffirmation of the Hospital Management Apostolate," Hospital Progress, 48, no. 5 (May 1967): 101-105).]
- Steffens, "Expectation and Role of Religious," 146.
- Bernadette Armiger, "Mutual Expectations of Laymen and Religious," Hospital Progress 47, no. 4 (April 1966): 76-77.
- Armiger, 76.
- Margaret Vincent Blandford, "The Religious Congregation and the Hospital," Hospital Progress 47, no. 4 (April 1966): 87. Others, including Edward Spillane, PhD, former chairman of the board of Incarnate Word Hospital in St. Louis, maintained that once federal money came in, the church should get out of health care: "A planned exit to disengage and use the resources for other worthwhile and defendable ministries for the poor is called for." (unpublished manuscript, circa 1992).
- Trafford Maher, "The Viability of the Catholic Hospital," Hospital Progress no. 7 (July 1969): 56. John Comey gives Catholic health care a firmer theological base when he asks whether the Catholic hospital sees itself as "a microcosmic Body of Christ in which there are many members in the same body." ("The Documents of Vatican II and the Catholic Hospital" Hospital Progress 52, no. 6 (June 1971): 50.
- Walter J. Burghardt, "Towards a Theology of the Health Apostolate," Hospital Progress 52, no. 9 (September 1971) 66-71 at 69 and 71.
- "Progress Report of CHA Task Force," Hospital Progress 48, no. 8 (August 1967): 36.
- Paul C. Reinert, "The Role of Religious in Management," speech adapted for Hospital Progress 48, no. 9 (September 1967): 59-61, 96-100, at 59.
- Reinert, 60, 61.
- Stokes, "Integration of Religious Life and Hospital Administration," 95. Stokes also cites French Dominican Albert Plé, who considered apostolic action a "school of perfection." We have come a long way from thinking of the ministry of health care administration as an "unusual" or "peculiar" manifestation of the Spirit.
- Stokes, "Integration of Religious Life and Hospital Administration," 95. He quotes the early Jesuit Jerome Nadal, who said there must be "some sort of causality between prayer and the apostolate, one helping the other."
- Stokes, 93.
- Trafford Maher, "How Long Does It Take to Form a Person for the Modern Apostolate?" Hospital Progress 47, no. 3 (March 1966): 57. For a fuller discussion of the importance of "intentional discipleship," see Sherry Wedell, Forming Intentional Disciples: The Path to Knowing and Following Jesus (Fort Wayne: Our Sunday Visitor, 2012).
- Maher, "How Long Does It Take," 53. Note, for example, the similarity to the definition of formation used by Ascension Health: "Formation is a life-long transformative process that opens us to God's action and connects us more deeply with self, God, others, and the world. Through self-reflection and other practices grounded in theology and spirituality, formation enables us to consider our calling, find deeper meaning in our work, realize our gifts, develop our competencies, and grow as a community in service of human dignity and the common good."
- Maher, "How Long Does it Take?" 55-56. Maher frequently addressed the importance of mature freedom and a personal relationship with Christ. These were definitely post-conciliar ideas. The understanding of human freedom he presents is a prerequisite for today's formation programs.
