BY: SR. MARY LOU AVERBECK, RSM
In the fall of 1994, Mercy Regional Health System Greater Cincinnati (MRHSGC) encouraged the leaders of its pastoral care departments to redesign their services. MRHSGC, a component of Catholic Healthcare Partners (then called Mercy Health System), comprised primarily four hospitals, a long-term care facility, and a home care service, all spread over a large geographical area. (MRHSGC also had a hospice, but it soon merged with another organization.)
At that time, each facility made its own arrangements for providing pastoral care to patients and staff. Mercy Anderson Hospital had long had a fully staffed pastoral care department. Clermont Mercy Hospital had a certified pastoral care professional on staff, an agreement according to which local priests visited to perform sacramental ministry, and a well-developed volunteer clergy organization. Mercy St. Theresa Center, the long-term care facility, had a resident priest who provided for the sacramental needs of Catholic residents. Mercy Hospital Hamilton and Mercy Hospital Fairfield each had full pastoral care staffs but shared a pastoral care director.
Catholic Healthcare Partners's director of mission effectiveness, with "grass roots" support from various pastoral care professionals, formed a task force composed of such professionals and asked it to reconfigure pastoral care as a network rather than separate departments. Having such a network, the reformers hoped, would enable MRHSGC to extend pastoral care beyond the walls of its facilities.
Pastoral Care's New Model
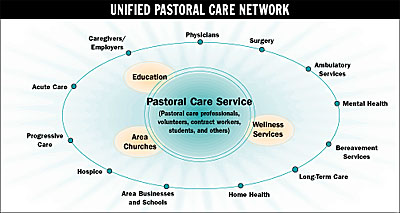
The task force, working with input from all pastoral care staff members, designed a model (see
Figure
) for the new, unified department. This model was essentially put into operation in 1995 (some parts are still being completed). The new pastoral care network is anchored by two "hubs." One, in the northern part of the greater Cincinnati area, serves Mercy Hospital Hamilton and Mercy Hospital Fairfield; the other, in the east, serves Mercy Hospital Anderson and Clermont Mercy Hospital.
Each hub has a pastoral care team with a team leader. Full-time pastoral care professionals staff the long-term care facility and the home care service. A director oversees the network as a whole.
Under the new model, pastoral care staff are employees of MRHSGC, rather than of the separate facilities, as they had been previously. The network itself is funded by assessments levied on the facilities.
The New Network in Action
MRHSGC's pastoral care network currently has 15 full-time employees, who get together every other month to discuss goals, policies, procedures, and "best practices." Hub staffs meet monthly.
The creation of the network has made possible several innovations.
Home Care Chaplaincy Program
Financial constraints had previously prevented MRHSGC from offering pastoral care to its home care patients. The new funding system has enabled the home care service to hire a pastoral care professional.
Volunteer Pastoral Companion Program
This program recruits and trains volunteers from the area to reinforce the efforts of the home care pastoral care professional. Professionals from the hubs mentor the volunteers, ensuring that each home care patient receives pastoral care.
Bereavement Program
As with other pastoral care services, each MRHSGC facility used to have its own bereavement program. Some facilities offered grief support groups for surviving family members; others held memorial observances; one facility had a complete bereavement education and resource packet.
Now the network has instituted a comprehensive program for all settings. Family members are given a sympathy card immediately after a patient's death. After a month, they are sent information about MRHSGC's four grief support groups. Within six months, they are invited to memorial services. If family members have indicated a need for special support, the staff makes follow-up phone calls to them at one and three months following the patient's death.
The network is currently developing bereavement care for staff members and their families.
Benefits of the New Model
The creation of the pastoral care network has resulted in a wide range of benefits. These include:
- Improved communication. Pastoral care workers, no longer restricted to a single facility, can now work easily together to develop new programs. They are also in a better position to exchange ideas with medical caregivers, business personnel, area clergy, and other members of the community.
- Centralized resources. Pastoral care clients now have improved access to support groups, rehabilitation services, and educational programs.
- Increased flexibility. Pastoral care workers, having collaborated to create basic presentations, can adapt them to fit the different educational needs of member facilities.
- More freedom to experiment. Pilot projects can be tested in one or two facilities before being extended to the network as a whole.
In 1993, more than a year before pastoral care was redesigned, MRHSGC began reconfiguring itself as network, a process that was not completed until four years later. During this larger effort, the pastoral care network was used as a prototype for the networking of larger departments. MRHSGC's leaders described the new pastoral care as an example of "creative restructuring."
For more information call Sr. Mary Lou Averbeck, RSM, 513-624-4526.
Sr. Averbeck is director, Pastoral Care Services, Mercy Regional Health System Greater Cincinnati.
