BY: JESSICA BRUNELLE, M.P.A., AND RETHA PORTER
Catholic health has a long tradition of embracing and reaching out to the most vulnerable and marginalized in society out of the conviction that "the least of these" is made in the image of God. This premise follows Christ's example as he stepped across cultural boundaries and misconceptions to heal and restore those suffering to a place of wholeness and a return to society. A striking example is the Gospel of Mark's account of Jesus healing a man possessed by a legion of unclean spirits. The man lived naked among the tombs, rejected and feared by society. Jesus, not only healed this man, but restored him to vitality and to community.
This reverence for humanity, particularly within vulnerable populations, remains vital to mission-based organizations as pressures mount for health care entities to care for an increasingly unhealthy and aging population with limited resources. Often, hospitals and clinics look to cut back on non-revenue-producing programs such as behavioral health, which can be costly to a health system. It is, therefore, increasingly important, in the midst of health care reform and ever-tightening budgets, to seek innovative ways to sustain the programs and services for the vulnerable patient populations we in Catholic health care are called to serve.
PeaceHealth St. John Medical Center, a licensed 346-bed acute care Catholic hospital in Longview, Wash., faced such a challenge after losing a large county mental health contract in the midst of health care reform and an ever-changing health care environment.
Longview is one of the poorest per-capita areas in Washington State, with high unemployment, an aging population and the accompanying social and health issues. The combination of health care reform and the loss of the county mental health contract put particular pressure on the hospital's behavioral health department; however, it also allowed the reallocation of some staff resources to help meet a longstanding need in PeaceHealth's primary care area. Primary care had long struggled to meet the needs of the community's vulnerable patients, often because of historically limited access to behavioral health and patient reluctance to seek services in a behavioral health setting. Frequently these patients would choose instead to seek services from the hospital's emergency department or from their primary care physician.
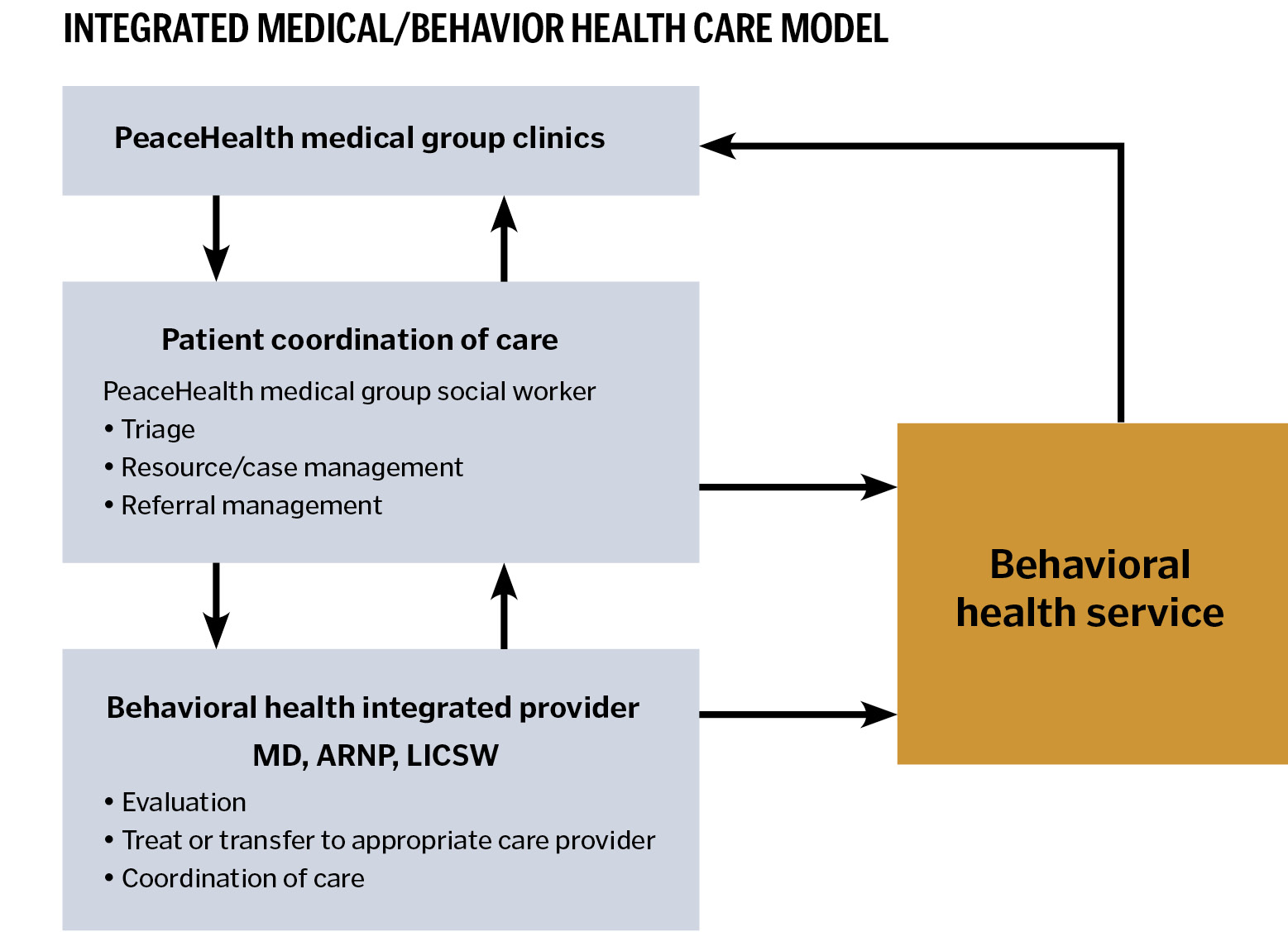
Providers from behavioral health and primary care clinics came together with PeaceHealth leadership in 2012 to seek a solution. The result: an innovative pilot program to serve the behavioral health needs of patients within the PeaceHealth Medical Group's primary care clinics. PeaceHealth Medical Group — a group of 117 primary and specialty care providers — already provided more than 14,000 behavioral health visits each year with 8,000 of these visits occurring in their family practice, internal medicine and OB/GYN clinics. Under the integrated care model, patients would be offered behavioral health services at their primary care clinic. The integrated care model triages behavioral health treatment needs for a patient during his or her primary care visit. Timely behavioral health triage assesses the patient's need for treatment and engages him or her in the medically necessary level of behavioral health care needed.
Transitioning the hospital's behavioral health providers — physicians, advanced registered nurse practitioners and licensed social workers — into a centralized primary care location at a regularly scheduled time each week creates a more streamlined venue for patient access to behavioral health services. Within the primary care setting, the behavioral health providers handle triage, evaluation, consultation and brief follow-up services as well as resources/case management and referral management. The shared space and close proximity of medical staff provides training opportunities for both primary and behavioral health providers. Medical providers have access to behavioral health professional input almost on the spot, resulting in improved quality of care while at the same time normalizing access to that care.
Normalizing the need for behavioral health care is important. In general, our culture inaccurately perceives individuals who suffer from behavioral health disorders as weak and unstable. At times, these labels and perceptions can result in feelings of shame for the patient and may lead to social isolation of a person in need of behavioral health treatment. Quality of care inherently improves when individuals feel free to receive treatment for medical needs rather than "special" behavioral health treatment in a "special" setting.
"Our patients have been very grateful for the opportunity to receive mental health services in the familiar setting of their medical home," said Tim Randall, MD, a family medicine provider.
Jodi Donaldson, a licensed social worker with PeaceHealth since 1999, sees a positive benefit for both patient and caregiver in the integrated care approach. Providers like having the behavioral health resource within the primary care setting for their patients who may need behavioral health care. The patient can be referred to a social worker right in the clinic where they can collaboratively determine the appropriate follow-up care plan.
The integrated care approach is especially beneficial for palliative, oncology and geriatric patients who are dealing with chronic disease issues or who may be experiencing anxiety or depression as a result of the aging process and life transitions.
"The elderly, in particular, are more comfortable being treated in a primary care setting due to the social stigmas and perceptions associated with behavioral health treatment," said Donaldson. Drawing on her experience as a licensed social worker with a behavioral health background, Donaldson uses her skills to help patients feel more comfortable, asking "Are you feeling a little blue lately?" rather than "Are you depressed?" Family members are also very grateful for the respectful and "normalized" treatment their aging loved ones receive in the primary care setting, she said.
"It's just a different environment, a more low-key approach and helps keep a patient's stress level down," said Donaldson.
Having someone with behavioral health training and skills working within the primary clinic setting also models behavior for others on staff. Donaldson remembers a primary care patient who had forgotten to take medication and balked at some routine procedures, such as recording blood pressure and weight, before seeing a provider in the clinic. The medical assistant working with the patient became so frustrated that she sought out Donaldson's assistance. Donaldson was able to gain the patient's cooperation and turn the situation into a positive experience for everyone — and the medical assistant thanked her later.
Donaldson remains hopeful that primary care staff will continue to respond favorably to integrated services, and she looks forward to a future of treating the "whole" patient in the primary care setting. On her wish list, she said, is for the program to include an element of spiritual care.
"It's all a process," said Donna Kolowsky, another PeaceHealth St. John social worker with behavioral health training. When primary care is overutilized for behavioral health needs, she said, providers can feel bogged down and patient needs are not met, causing frustration on both sides.
"The behavioral health social workers are able to keep patient stress down and keep things from escalating for the patient and caregiver. It's a win-win for both," Kolowsky said.
Family medicine provider, Christopher Collins, MD, said he finds the program very helpful. "Often, I'm able to get my patients that need immediate [behavioral health] care in within a day or so, which helps relieve my stress level, especially when they are on multiple psychiatric medications that I feel uncomfortable prescribing," he said.
Another benefit of the integrated care model is the appropriate triage of patients for behavioral health treatment, thus reducing inappropriate admissions to another hospital floor and involving other caregivers unnecessarily.
Laura Wagner, ARNP, a behavioral health provider in the primary care setting, said, "In my experience with PeaceHealth's pilot program, integrating mental health services in a primary care setting reinforced the wisdom of such a strategy. For too long, mental health services were a sequestered sector of our health care delivery system. That separation from mainstream medical care carried an implicit stigma with it."
"Naturally, an approach that keeps mental health patients in a separate and distinct location reinforces negative stereotypes, which for many patients is not only insulting, but might also discourage them from seeking care," she said, adding, "When mental health and primary care are integrated into a unitary program of services, mental health patients are merely part of the traffic flow and are not highlighted or singled out in any way. I believe that this anonymity creates a much more comfortable environment for those seeking care."
"Perhaps the most important function of this integration concept is a decisive improvement of access to services for patients," she said. "The facilitation of getting a mental health referral from one's primary provider to see a colleague in that very same venue is a much simpler, less daunting and certainly less stigmatic experience for those in need of mental health treatment."
PeaceHealth's integration of behavioral health services and primary care is an excellent example of transforming the challenges of health care reform into an opportunity. The temptation to succumb to financial pressures in today's health care environment is great. With this innovative solution, PeaceHealth has chosen to remain true to Catholic health social values and PeaceHealth's mission: "We carry on the healing mission of Jesus Christ by promoting personal and community health, relieving pain and suffering and treating each person in a loving and caring way."
Through normalizing the care for behavioral health patients, they are not only restored in body, mind and spirit, but they are restored to community in a way that patterns and honors the healing ministry of Christ.
JESSICA BRUNELLE is clinical supervisor, behavioral health, at PeaceHealth St. John Medical Center, Longview, Wash.
RETHA PORTER is communications and public relations specialist at PeaceHealth St. John Medical Center, Longview, Wash.
