BY: FRED ROTTNEK, MD, MAHCM
Because he focused on the social determinants of health of his time, there is no doubt that he would challenge us to explore the deeper stories surrounding gun violence, sexual violence, abuse and neglect — social determinants of health for us.
There also is no doubt he would be disappointed that we haven't pursued a generosity of spirit and developed a moral theology of caring for those affected by violence and chronic stress as zealously as we have pursued medical research and technology.
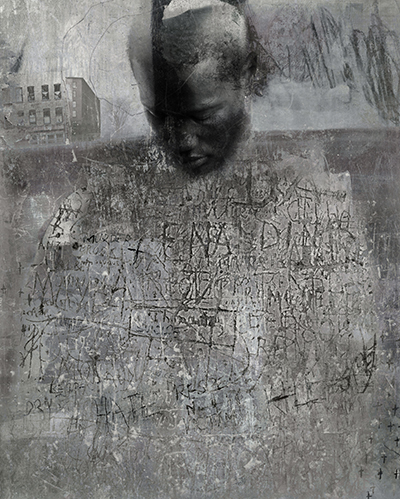
ST. LOUIS AS A SYMBOL
The eyes and ears of the world were on Ferguson, Missouri, in August 2014, when an unarmed black youth, Michael Brown, was shot and killed by a white police officer. Since then, regional tensions, stress and violence have ebbed and flowed, an example of what happens in communities affected by decades of chronic toxic stress and trauma.
Missouri's St. Louis area has long struggled with segregation, health inequities, infrastructure challenges, uneven tax bases and unpredictable public health funding. In years past, despite the advantage of having several large health care systems in the area, there was little cooperation among the hospital systems and the developing Federal Qualified Health Centers caring for the underserved residents of these communities.
According to the FBI's latest Semi-Annual Uniform Crime Report, violent crime in St. Louis makes it one of the nation's most dangerous cities with a population over 100,000. After the 2014 shooting in Ferguson, a north St. Louis County suburb, international attention focused on the aftermath: demonstrations, arson, "militarized" police response to community unrest and the rise of the Black Lives Matter movement that spread to other U.S. communities that also experienced police confrontations with African-American residents.
Underlying most of the post-Ferguson conversations and plans to address regional segregation, there is acknowledgment that the systems influencing people's lived experiences play a role in determining health outcomes and creating inequities. Using the lens of the social determinants of health is not new — what's new is bringing social determinants front and center among diverse public and private discussions. For the first time, people in the region are working together to not only reduce violence and disparities and uncover unhealthy practices and disease, but to look upstream to find out why they exist.
ACE STUDY
California's Kaiser Permanente health system and the Centers for Disease Control and Prevention collaborated on research that ultimately led to the trailblazing Adverse Childhood Experiences (ACE) Study that demonstrated a staggering correlation between adverse events in childhood and poor health outcomes as an adult. The study, conducted in 1995, shows that persistent, toxic stress creates poor health outcomes. The study also highlights the prevalence and impact of trauma and toxic stress in society.
The correlation between traumatic and stressful childhood events and negative adult health outcomes results not only from behavioral factors, but also from biological changes to the body, because the body's natural response to stress, the hypothalamic-pituitary-adrenal axis (HPA), is programmed to react with the same level of intensity to varying threat levels. Individuals who experience persistent and toxic stress, especially at a young age, over-utilize their HPA, which is highly destructive to physical, psychological and neurological development.1 The correlations among violent childhood experiences and vulnerability to similar experiences during adulthood are particularly striking. A CDC-supported study linked the ACE variable directly to sexual abuse during adulthood; in fact, there was an increase in sexual violence risk with each additional ACE recorded for an individual.2
Today, the ACE study shapes thinking about how to improve the health of a community by looking past symptoms to find the root causes of issues such as violence. Across the country, communities are engaged in efforts to become "trauma informed," that is, to look for and identify the interpersonal and social violence and chronic social stressors that have touched people in childhood or as young adults and have had a lasting effect.
St. Louis is the latest region to build upon the ACE study to reimagine a healthy community for everyone. The work was taken up by the St. Louis Regional Health Commission, a consortium of government representatives, providers of care and members of the community "charged with developing and implementing a long-range plan to improve health care access and delivery to the uninsured and underinsured," according to the organization's website. The work began several months before Michael Brown's death, and it has become a grassroots community movement called Alive and Well STL. (See sidebar)
Since its inception in 2001, the St. Louis Regional Health Commission has increased outpatient safety-net health care services, integrated the region's health care system for greater efficiency and piloted the Gateway to Better Health Demonstration sponsored by the federal Centers for Medicare and Medicaid Services. In doing so, the Commission has preserved more than $400 million in health care funding and increased the health of the region.3
The Regional Health Commission is particularly interested in how to apply ACE research findings to reduce health disparities in the St. Louis metropolitan area, leading to better health outcomes for all citizens — regardless of age, race, sex or insurance status. To that end, the commission is working to encourage service providers, both in health care and other sectors, to create understanding and acceptance in the general community of the fact that good health is a result of both physical and emotional well-being. Those are initial steps in helping the region to become a trauma-informed community.
The St. Louis Regional Health Commission also is working with the Missouri Department of Mental Health and the Saint Louis Mental Health Board, Mental Health America of Eastern Missouri and the Behavioral Health Network to elevate the Missouri Model, a framework for the implementation of trauma-informed practices, to a high profile across the region and nationally.
Conclusion
We are hopeful that working to move from trauma awareness to becoming a trauma-informed community will prevent violence, trauma and chronic illness before it occurs, by giving people the skills, tools and resources they need to overcome the stress in their circumstances and lead healthier lives. Also, by highlighting the region's best practices for trauma-informed services, the commission hopes to ensure that mental wellness is a funding priority for the State of Missouri, foundations and other funders.
Catholic health care systems in the St. Louis region, including Mercy and SSM, are active leaders in the Regional Health Commission and not only have embraced the Alive and Well STL message, they have found creative ways of implementing the message into the culture of their institutions. From patient care to staff support to physician residency training opportunities, Alive and Well STL has become an avenue to improve the health and well-being of organizations, service delivery and the region.
Truly understanding the impact of violence and toxic stress changes one's view of individuals' and communities' health and well-being. When we have patients in our systems, offices and emergency departments who show terrible manifestations of choices they have made, we must pause to ask what has happened to these patients that brought them to such behaviors. Looking for such causes is good practice, but it is also effective practice: We know the behavior cycles continue unless we can work with individuals to address the root cause. Until we address root causes, we can never become alive and well.
FRED ROTTNEK is associate professor, director of community medicine, Department of Family and Community Medicine, Saint Louis University School of Medicine, St. Louis.
NOTES- MacArthur Research Network on Socioeconomic Status and Health, "Allostatic Load and Allostasis, Allostatic Load Notebook www.macses.ucsf.edu/research/
allostatic/allostatic.php. - Katie A. Ports, Derek C. Ford and Melissa T. Merrick, "Adverse Childhood Experiences and Sexual Victimization in Adulthood," Child Abuse and Neglect Journal 51 (January 2016), www.ncbi.nlm.nih.gov/pubmed/26386753.
- St. Louis Regional Health Commission, "History," www.stlrhc.org/about/history/.
ALIVE AND WELL STL: A REGIONAL RESPONSE TO TRAUMA AND TOXIC STRESS
Alive and Well STL is a collaborative grassroots movement to reimagine and reconnect communities in the St. Louis region. By bringing together theory, practice, empathy and compassion, the group plans to courageously address community histories and move forward into a healthier future.
The roots of Alive and Well STL stretch back to December 2012. That was when the St. Louis Regional Health Commission released its Decade Review of Health Status report, and the surrounding region was ready to pay attention in new ways. The report was a simultaneous snapshot of current health status as well as history of change over the preceding 10 years, as the area population shifted.
Although the report found overall improvement in health status throughout the area, race- and gender-based disparities persisted, as did some medical risk factors. Roughly 1 in 3 residents was obese, and slightly more had high blood pressure and high cholesterol. Approximately 27 percent of St. Louis City residents smoked, as did approximately 15 percent of St. Louis County residents.
The grimmest change involved violence. Homicides increased in the region by 18 percent between 2000 and 2009. Zip codes with the highest rates of victims tended to be clustered in the City and in the North County.1
To help disseminate the results, the commission partnered with Rare Gem Productions in St. Louis to create a weekly 15-minute radio program called "Alive and Well STL." It featured community members and local health experts discussing community-driven health topics, particularly from the experience of community, relationships and faith. The program quickly grew an audience and regional recognition. The highest-rated shows focused on health disparities, the impact of substance abuse and the stigma of behavioral illness.
After two seasons of broadcasts, the St. Louis Regional Health Commission brought together its two advisory boards to brainstorm a new version of Alive and Well, one that creates a community-wide effort to reduce the impact of toxic stress and trauma on health and well-being. Joe Yancey, chair of the commission's community advisory board, suggested trying a model he had studied — trauma-informed community building, a grassroots program of community education, dialogue and programming about the long-term and cumulative effects of trauma and toxic stress on individuals, families and communities.
During his long career in community mental health services, Yancey, executive director of the St. Louis nonprofit Places for People, has learned this: When people and communities are exposed to violence, there are enduring, cumulative negative effects on health, choices and behaviors.
Alive and Well STL is an effort to encourage everyone — from individual citizens to entire school systems and many other organizations and institutions — to create opportunities for healing, so everyone in the community can live a healthy life. To move St. Louis toward being trauma-informed, the Regional Health Commission is working with health care service providers and others to help the general community understand — and accept — that good health results from both physical and emotional well-being. The commission is nearing the end of its first year of intensive media promotion of the Alive and Well STL initiative with newspaper and broadcast partners, as well as using websites, Facebook and Twitter in order to continue reaching people in the community who traditionally are not included in public health media campaigns.
Nationally, the Substance Abuse and Mental Health Services Administration has declared creating trauma-informed communities to be "the next major era in public health." Furthermore, the Missouri Model of implementing trauma-informed practices is nationally recognized, and Alive and Well STL exemplifies its implementation.
NEXT STEPS
The Missouri Department of Mental Health is facilitating development of Alive and Well STL Learning Collaboratives. Member organizations will receive about 18 months of expert consultation on how to implement trauma-informed practices. Consultation will be based on the Missouri Model for the stages of trauma integration within an organization. By the end of the collaborative session, each participating organization will have an ongoing work plan to guide them over the next year.
Among the key components of each learning collaborative are:
- Introductory training/meetings for staff and leadership, as needed
- Advanced trauma training for the trauma committees within each organization
- Monthly webinars/training for trauma committees to provide technical assistance in specific areas of organizational change (based on SAMHSA's 10 "domains" for implementing a trauma-informed approach): governance and leadership; policy; physical environment; engagement and involvement; cross-sector collaboration; screening, assessment and treatment services; training and workforce development; progress monitoring and quality assurance; financing; and evaluation
- Monthly coaching calls and limited on-site support for each organization, to provide guidance on implementation
The St. Louis Regional Health Commission also has convened a team charged with developing an evaluation strategy for the Alive and Well STL initiative. Building from data gathered through qualitative and quantitative analyses during trauma-awareness training sessions, the evaluation team has created a logic model, identified a core patient population in order to evaluate the population impact from the initiative, and generated a request for proposal for an external evaluation team to deliver the following:
- Comprehensive evaluation plan, formulated with input from community stakeholders
- Benchmark updates on protocols, results and anticipated conclusions
- Final product displaying progress on identified metrics
- Final product geared to share process learning with community partners and other trauma-based initiatives
- Recommendations for dissemination strategy
NOTE
- St. Louis Regional Health Commission, "Executive Summary," Decade Review of Health Status (2012). http://qocri3zgw3918amdk1xadmx1.wpengine.netdna-cdn.com/wp-content/uploads/2013/07/Decade-Review-Executive-Summary.pdf.
