BY: JIM WITHERS, MD
In 1992, I decided to begin making house calls.
I should say I decided to return to making house calls, for I used to make them with my father in rural Pennsylvania when I was a child. I remember riding along with him in his little VW into the hills of south-central Pennsylvania. For me, it was a wonderful adventure but also time to spend with my very busy father, a dedicated country doctor. Those visits shaped my sense of medical care. His patients clearly loved my dad, and some of that love spilled over to me in the form of cookies, milk and the nickname "Little Doc."
My mother, a registered nurse, reinforced my sense of purpose when I learned to drive. It was while doing Meals on Wheels with her that I mastered parallel parking. Later, as a family, we did medical work in Nicaragua, Guatemala and St. Lucia. Service that went to those in need was a natural part of our lives. The sense of purpose that filled me during those international trips sealed my desire to become a physician.
On the first day of medical school, I felt I had entered into a sacred profession. I still feel that way. When I finished medical school, I knew I wanted to continue to care for those in need, but I was uncertain what the path would be. Wisely, I chose a residency at the Mercy Hospital of Pittsburgh, a system built on the solid mission foundation of the Sisters of Mercy. "Plant your seeds in the right soil" is advice I give my students, but even in the best health systems, the structure and culture can fall short of our ideals.
For several years I tried to develop hospital protocols for detecting and dealing with domestic violence, but had only mixed success. The thing that astounded me was that despite the prevalence of domestic violence victims among our patients, we remained largely unaware of their suffering. Not only did this ignorance prevent proper treatment and follow-up, it reinforced to the victims the notion that their actual circumstances were irrelevant to the medical community.
I learned to anticipate a diagnosis of domestic violence if a female patient's numerous expensive tests were negative and staff was growing hostile towards her as a problem they couldn't seem to solve. So often in the rush to perform tests and studies, we forgot to really listen to the person in front of us. It was shocking to me that just giving attention to each patient's story could make me a much better diagnostician. The more I looked, the more I saw groups of patients whom we were serving frequently, but not serving very well. They tended to be the ones we didn't like very much.
Self-examination does not come easily to any of us, especially professionals like doctors and nurses. We are convinced of our own good intentions, and this can prevent us from seeing how things look from the patient's point of view. If things go poorly, and we know we have adhered to our standards of treatment, the tendency is to blame the patient for the lack of effectiveness. Not coincidentally, these most often seem to be poor patients, those struggling with complex mental health issues, lack of transportation, housing, recovery services and insurance.
In a professional epiphany, I realized how many patients passed through our care whose health was affected by social circumstances to which we were blind. To not address the centrality of their real life issues was tantamount to a thought disorder on our part. By allowing the reality gap to widen between our most vulnerable patients and our system, we were not only wasting money, but also failing to achieve the best results. The sickest patient, perhaps, was the medical system I loved.
OUT ON THE STREETS
On reflection, I felt it was time to get out of the hospital and see things from another perspective. House calls might just be what the doctor ordered. But if we were really to have the transformation we needed, it would have to be a fairly radical experience.
One of the patients I had seen in the hospital was a homeless man who left against medical advice and went out into a snowstorm. I learned later that he froze to death. That man haunted me. Somehow, his death wounded me. I believe that true healing requires connection with those we serve, but on the night he left the hospital, I was unable to make a connection with him. He left me with a deep sense that my own healing was out there, somewhere, under the bridges of my city. I began to look for a way to make house calls to the homeless.
As God would have it, the only sabbatical of my career was offered to me at just that time. For a month, I learned everything I could about the homeless and the network of providers who cared for them. Over and over, I would ask about the people who didn't come to the shelters or clinics. Nobody, it seemed, was actually going out to see how they were doing.
Finally, however, I was introduced to a formerly homeless man named Mike, who had been visiting the street homeless for six years on his own. I asked if I could join him. Initially he was skeptical about bringing along a "suit," but he agreed to take me if I "didn't dress like a doctor" and "didn't act like a jerk." Being a typical academic, I checked out a book on how to dress like a homeless person. Apparently passing Mike's dress code, I began to make visits with him at night, into the alleys, along the riverbanks and in the abandoned buildings of Pittsburgh. I would let my malpractice carrier know about this later.
A SECRET WORLD
A new world opened up to me. On the riverbanks, in the alleys and abandoned buildings were hundreds of people with virtually no health care. There were young pregnant women, veterans with post-traumatic stress disorder, people with untreated diabetes, hypertension and other illnesses. One of my first patients was an 85-year-old man whose leg ulcers were teeming with maggots. It was overwhelming. Almost none of these people had insurance, and most refused to go to the hospital. Not knowing what else to do, I began to treat people on the streets.
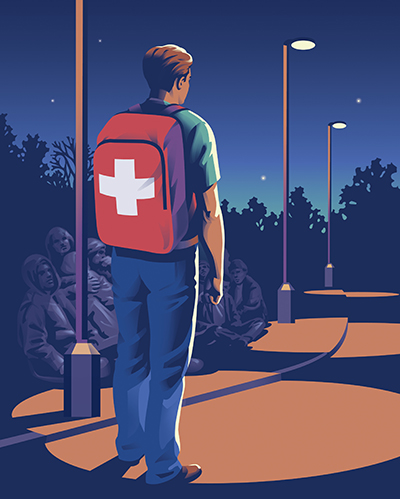
It didn't take long till I developed a practice. As I began to provide medical care from my backpack, some of the homeless people embraced me, calling me "Doc Jim." From one bridge to the next, I got referrals from the street folks to see their friends who were in need. Before long, I had what would have been a thriving and profitable practice, were these patients who could pay.
In fact, they did pay me with their profound gratitude. I remember one man sobbing by the river bank, saying, "I can't believe someone still cares that we're alive!"
At night as it was raining, I would think of the people I knew were suffering out there. Each was becoming known to me as a precious, unique human being. And I was becoming an integral part of their world. When possible, I worked to get patients to come into our clinic. When not possible, I just tried to keep them alive. It wasn't always easy.
One night, a couple of the homeless guys came to find me. Old John, one of the older homeless men, wasn't feeling well, they said. In a nearby doorway, Old John was curled up and holding his belly. After a quick exam, it was apparent that he was critically ill, so I called the emergency room. Before long, the paramedics arrived. Before even examining him, they shook their heads and said, "Don't worry about him, he's just an old bum. We know him well."
As they turned to leave, I made it clear I was a physician and that Old John should go to the ER where they were waiting for him. Reluctantly, the paramedics took him away. Later I learned he required immediate surgery or he would have died that night.
SHEDDING THE DISGUISE
It eventually occurred to me that my homeless disguise might be a little too convincing. When I tried to enter certain stores to buy a cup of coffee, I was turned away. Mike, searching for one of the homeless guys, decided to investigate the subway tracks. Refusing to join him on the tracks, I stood defiantly, hands on my hips, until he came back. About two blocks away from the subway station, a couple of police cars suddenly pulled up, and a policeman jumped out, pointing at me.
"We got you on the video camera urinating in the subway! There's no use arguing about it!" he shouted. After a few awkward moments, I was able to explain my role as a physician and persuade him I was innocent of the charge. To his credit, the policeman chuckled and asked for my card so he could call if he saw any homeless people with medical needs.
When one of the homeless guys asked me why I dressed so poorly, I realized it was time to just be myself.
Gradually, more and more of the street homeless began coming to our clinic. Building on trust developed on the streets, they were willing to take the next step to establish primary care.
It was a blessing to watch the nurses and clinic staff gradually welcome the street homeless into the clinic for the care they deserved. I know it revived our sense of mission as an organization.
We dealt with some colorful characters, but there were poignant moments as well. A frightened young pregnant woman came to see us one night. She had tried every shelter in town, and there was no room for her anywhere. In a few weeks, she would deliver her first baby. Unable to think of anything else, we took her to a hotel. After checking her into a warm, safe room, I took my stethoscope and listened to her abdomen. After searching, I was able to hear a rapid, strong little heartbeat.
Smiling, I handed the earpieces to the young woman so she could hear it herself. Her eyes grew wide with delight as she heard the sound of her baby's heart for the first time. Then Mike listened, and then she asked to hear it again. It was a magical night, and, thankfully, it was the first step to a safe delivery of a healthy young boy.
Soon, other volunteers and students joined the work, and Operation Safety Net officially was born. My parent organization, the Pittsburgh Mercy Health System, was supportive from the very beginning. Speaking with the CEO, a Sister of Mercy, I soon learned why they felt Operation Safety Net was so special. In 1843, the seven sisters who founded the hospital had come over from Ireland to walk the streets and care for the poor. Known as the "Walking Sisters," six of them gave their lives in an epidemic. Learning of their legacy, I felt God's blessing in our work.
I finally told my malpractice carrier where I was practicing and dedicated myself wholly to the street work. Our program expanded, and we were able to establish an office with social workers, a full-time nurse and dedicated staff. In the years that followed, we have been able to provide medical care and counseling, but also we have been able to move more than 1,400 chronically homeless people into their own apartments. Now part of an integrated care model, we are accomplishing more than I could have imagined when we first began.
TRIP TO INDIA
In 1993, I made a trip to India to meet a doctor in Kolkata, Jack Preger, MD, who had been working on the streets there since 1979. Before seeing him, I visited the Missionaries of Charity motherhouse in Kolkata and was lucky to have a chance to talk with Mother Teresa about my work and to hear her thoughts. What a blessing! She had great sympathy for our Pittsburgh homeless, especially in winter.
After a very moving visit to her order's House of the Dying, I made my way to see Dr. Preger at Calcutta Rescue, a registered non-governmental organization that helps the poor in Kolkata and parts of West Bengal. For me, it was an epiphany. I had never met another physician who had pioneered the kind of work I was doing. Watching him work and comparing notes, I was convinced we had a common field of medicine.
From that day onward, I dedicated myself to promoting what I now call "street medicine." It has been a privilege to help 36 other street medicine programs to be created in cities around the world, and there are 16 more in the process of forming. In 2005, we hosted the first International Street Medicine Symposium in Pittsburgh. It is the only gathering of its kind, bringing together those who work medically on the streets and helping them to improve their work and build what is now a global movement.
In 2008, a new nonprofit, the Street Medicine Institute, was launched in the Greater Pittsburgh area to be the home of this new field of health care. The 10th International Street Medicine Symposium, held in 2014 in Dublin, had a record number of participants from six continents.
No matter how many cities I visit, and how many homeless people I meet throughout the world, I have a special love for the street homeless of Pittsburgh. As I'd hoped in the beginning, the street homeless have been my greatest teachers. By allowing me to be part of their lives, mine has been enriched beyond measure. I've been taught how hard it is to be rejected by society, but also how strong many of the street homeless are in the face of adversity. I have been inspired to see so many of them reclaim their lives. They have taught me to laugh in times of trouble, and their love has given me hope that we can heal as a society. Through the students whose hearts they touch, our street homeless have helped create a better future for our health care system.
In the final analysis, it's the bonds of connection that are the most powerful force we have. Despite the best technology in the world, real healing ultimately depends on a commitment to each other.
This week, one of our homeless men was tragically burned. As he lay in his bed, I asked him if he had any family that had visited him. A tear rolled down the scarred surface of his cheek. After some time looking at me fiercely, he choked out, "You people are my family!" What came from the heart spoke to the heart. Whatever lay ahead, we would face it together.
JIM WITHERS is the founder and medical director of Operation Safety Net, part of the Pittsburgh Mercy Health System and Trinity Health, serving in the tradition of the Sisters of Mercy. He holds the position of clinical assistant professor of medicine at the University of Pittsburgh and is also the founder and medical director of the Street Medicine Institute.
