Executives and policy advocates at CHA and its member health systems are on the alert for the ripple effects of the end of the COVID-19 national and public health emergencies that created temporary flexibility in how care is delivered.

Michael Richards, vice president of government programs and public policy at SSM Health, cited relaxed pandemic regulations related to telehealth, including the allowance for mental health services to be provided to Medicare enrollees by phone.

Richards leads the Interstate Healthcare Collaborative, which operates out of SSM Health. The collaborative advocates for and provides education on interstate license compacts and telehealth policy on behalf of health systems and medical associations.
"During the public health emergency we showed that caring for patients at home through telehealth or digital health has been successful and widely accepted by the general public," he said.
Regulators are in the process of deciding whether or how to make permanent some rule changes. Health care leaders said they hope the innovations spurred, the lessons learned and the examples set by Catholic health systems during the COVID pandemic will be taken into consideration by policymakers as they make those decisions.

"We really have to remember what that first year was like and what we did as a society to come together and the important leadership role that Catholic health care played," said Kathy Curran, senior director of public policy at CHA.
She pointed to the rapid development and deployment of COVID vaccines and to the work of the Catholic Cares Coalition. The coalition, which CHA and several of its member systems helped establish, has promoted equitable access to those vaccines at home and across the globe.
Phase out begins
The Biden Administration has said it will let the COVID public health emergency declaration lapse May 11. A separate national emergency that was declared because of the pandemic ended April 10.
The declarations, in place since early 2020, eased many federal health care rules and provided flexibility to triage health care services to combat the deadly novel virus. The changes increased access to virtual care at home for patients with chronic conditions at a time when hospitals and outpatient facilities were locked down early in the pandemic. Even years into the pandemic, many vulnerable patients feared inpatient appointments heightened their contagion risk.
Telehealth boom
Regulation waivers from the Centers for Medicare & Medicaid Services gave Medicare enrollees wide access to virtual care outside of overwhelmed hospitals and providers permission to bill just
as they would for in-person visits.
State Medicaid programs and private insurers quickly followed suit. Outpatient care providers stood up or expanded telehealth services with remarkable speed.

Dr. Hoda Asmar, executive vice president and system chief medical officer for Providence St. Joseph Health, said the impact of the temporary waiver was immediate.
The system was already a national leader in telehealth with 70,000 virtual visits across its seven-state service area in 2019. In May 2020, shortly after CMS eased restrictions, Providence's virtual visits just for the month jumped to 200,417.
Asmar called it particularly helpful that the telehealth waivers by both public and private insurers have covered mental and behavioral health care visits at a time when the pandemic and its impacts have driven up the need for those services.
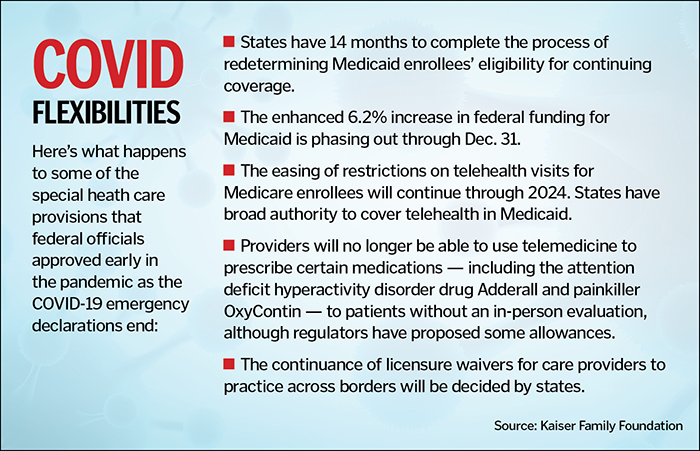
CMS has extended the telehealth flexibilities for Medicare through 2024. CMS also extended through next year the Acute Hospital Care at Home initiative, which has allowed hospitals to expand inpatient-level care into patients' homes.
Curran said the extensions give the agency and other policymakers time to study whether the flexibilities improved care delivery and health outcomes for patients and whether they were cost effective. She said the findings will help guide CHA's advocacy efforts around making the special provisions permanent.
Medicaid reenrollments
Another key aspect of the COVID emergencies was to temporarily lock in Medicaid recipients' eligibility and coverage. The Kaiser Family Foundation reports that the number of enrollees in Medicaid and the Children's Health Insurance Program jumped to 95 million by the end of March, a 32% increase from February 2020. The spike was primarily due to the
emergency continuous enrollment provision but some of it was because of coverage expansions under the Affordable Care Act.
Legislation passed in December decoupled the Medicaid coverage provision from the public health emergency and allowed it to lapse on April 1. Starting then, states could begin determining whether enrollees still qualify for coverage and the federal government began scaling back a 6.2% funding enhancement. The Kaiser Family Foundation estimates that 5 million to 14 million people could lose coverage during the unwinding of the Medicaid continuous enrollment provision.

Paulo Pontemayor, senior director of government relations at CHA, said Congress did put some guardrails in place to prevent the unwinding from having an abrupt impact. For one thing, states have 14 months to complete the redetermination process.
Pontemayor said Congress also authorized CMS to work with states to ensure that there is extensive outreach to patients and efforts to move those who are no longer eligible for Medicaid to other options, such as subsidized policies purchased on the health care marketplace. CHA created a toolkit of resources called Protect What's Precious for its member health systems related to Medicaid reenrollments.

Brenda Chilman, chief revenue officer for SSM Health, said her system is working with its Medicaid eligibility vendor on an outreach campaign to people who have to reenroll to provide support and resources to secure Medicaid coverage or to direct them to other sources for coverage.
Among the complicating factors, Chilman said, is that the redetermination process varies in each of the four states where SSM Health operates. "The risk is that those patients who are eligible for Medicaid won't successfully complete the reenrollment," she said. "Our approach here is to provide active outreach to help them navigate this reenrollment process."
Asmar said Providence has trained its frontline staff on how to guide patients who rely on Medicaid to reapply or access other options such as the health insurance exchange. The system also is offering people who are potentially losing their coverage access to financial counselors who can navigate them through options based on their needs.
In part because of the Medicaid continuous coverage provision, the nation saw its uninsured population drop to around 8% last year, a historic low. In addition, the number of uninsured children decreased during the pandemic, reversing a decline in coverage.
Asmar is concerned that those advancements will be lost during the Medicaid redetermination. She noted that estimates say at least 6 million children will lose coverage. "This is a setback in our journey on improving health equity and access to care for all," she said.
A provision that is lapsing completely to the disappointment of Asmar and others regards Medicare coverage for people in need of skilled nursing care. That waiver has allowed patients to file Medicare claims for nursing home care without first spending three days classified as a hospital inpatient. Asmar said the waiver helped reduce backlogs and create capacity in acute care settings.
Lessons learned
Lucas Swanepoel, CHA senior director of government relations, praised the overall effort by policymakers and providers to ensure patients' access to care during the health emergencies.
He said that effort — including rule waivers and substantial federal financial assistance to hospitals — was critical to keeping health systems afloat at a time when many nonemergency services had to be suspended and
supply and labor costs soared.

He noted that the policy waivers and financial aid were a piece of a massive pandemic economic policy response that included loans to businesses, direct payments to families and enhanced unemployment benefits as well as small, but significant, increases in food assistance to families — all of which worked to lessen the impact of the pandemic on the nation.
"I think moving forward, this will continue to be a lesson on how we create policies that support a stronger social safety net while also supporting health care providers," he said.
Asmar pointed to three big takeaways from the nation's response to COVID. The first is that the U.S. needs to be in a better state of readiness before the next pandemic. She urged a hard look at supply chain, stockpiles and public health infrastructure.
The second lesson is to continue the progress on policies and action to address health equity, as was evidenced by the drop in uninsured Americans while the Medicaid moratorium on ending coverage was in effect.
Lastly — and Asmar said this keeps her awake at night — is that health systems must become better at caring for their caregivers. Providence, she said, is focused on safeguarding and promoting the well-being of its caregivers.
CHA created many resources related to caregiver well-being that are available for members' use at chausa.org/well-being.
