MARIA GATTO, MHsB, ACHPN, APHN-BC
System Palliative Care Consultant, PeaceHealth
Patients' needs are growing exponentially, as people are living longer with serious and complex illnesses. Despite the advances of modern medicine and technology, health care systems can be siloed and fragmented, with medical models that don't always put patients and their quality of life at the center of their care. Current care models often don't align with what matters most to patients, nor do they prioritize their values, goals and preferences so that they and their health care team can choose the care uniquely appropriate to them and their situation.
In addition, there were people already facing serious illness prior to the pandemic who then contracted COVID-19, and many will require a greater level of care than what medical professionals have previously provided or have been taught in medical schools. Health care resources have been stretched thin. There is now a national health care staffing shortage that is straining medical professionals' physical, mental, emotional and spiritual health as well as stressing our health care systems and society in ways not previously experienced. The increased use of palliative care provides a new and better model to effectively address these health care needs. Not only does palliative care attend to these issues, but it provides for better care navigation in the COVID environment. Hallmarks of palliative care include the use of skilled emotional support while also reducing moral distress and confusion by clarifying and aligning care with the goals of patients and their families.
Palliative care is specialized medical care for those living with a serious illness that is focused on providing relief from the symptoms and stresses of the condition. The goal is to improve quality of life for both the patient and the family through a specially trained, interdisciplinary team of doctors, nurses and other professionals who collaborate with the individual's other physicians to provide an extra layer of support. It is based on the needs of the patient, not on the patient's prognosis. Appropriate at any age and at any stage during a serious illness, palliative care can be provided along with curative treatment.1 Serious illness is defined as a "health condition that carries a high risk of mortality and either negatively impacts a person's daily function or quality of life or excessively strains their caregiver."2
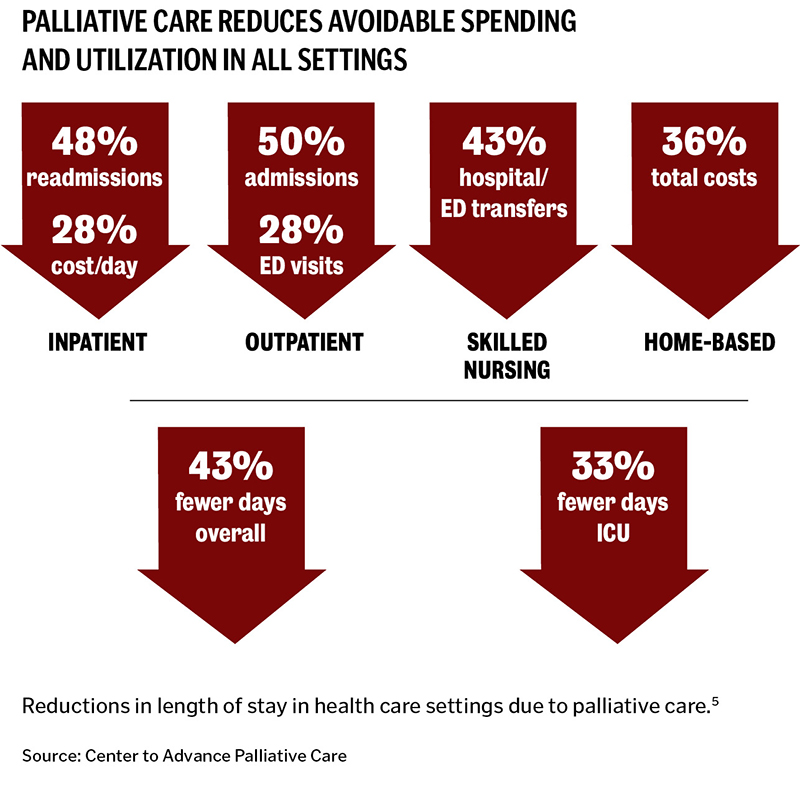
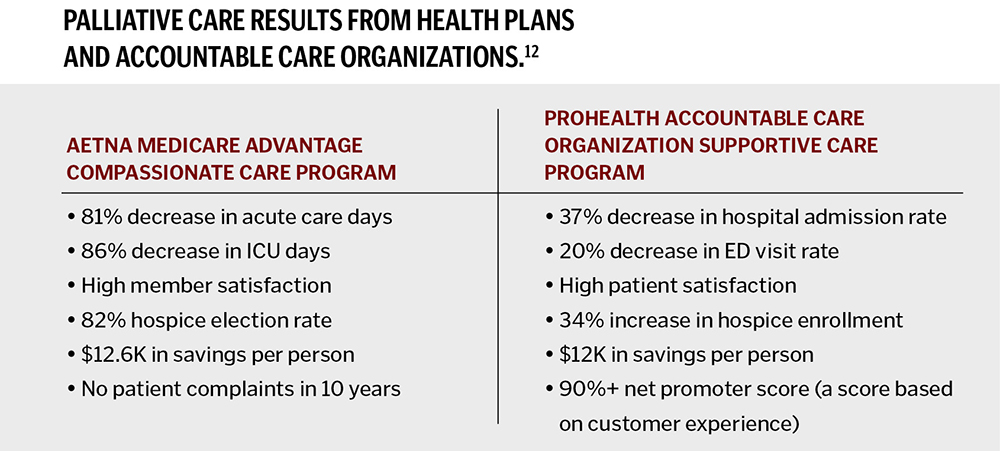
Palliative care focuses on patient-centered outcomes, including quality of life, symptom burden, emotional well-being and caregiver need. Its emphasis on communication and continuity of care fits the episodic and long-term nature of serious, multifaceted illness. Since it helps ensure that resources are matched to patient and family needs and priorities, it results in substantially lower unnecessary hospital spending, providing patients and clinicians across an entire health care system with an effective solution to a growing challenge.3, 4
At PeaceHealth, palliative care programs began in 2018 through its foundations and philanthropic funding. As programs grew in demand, the PeaceHealth executive leadership team recognized the critical role that palliative care plays in its Catholic mission and in alignment of health system strategies, including effective care management of complex, chronically ill patients and shared financial risk for high-risk patient populations. The health system is currently investing in more access to palliative care programs across the continuum of care. It is working to enhance effectiveness, efficiency and standardization related to program models, staffing, health system education and skills training, specific electronic medical record documentation, predictive analytics, data collection and measurement and reporting that meets quality, operational, management and accreditation guidelines.
PeaceHealth hired this article's author for expertise in helping health systems across the country to implement palliative care programs while optimizing it as a service line with the rigor necessary to meet system goals. Darrin Montalvo, executive vice president, chief financial and growth officer for PeaceHealth, has been fully supportive of the work throughout the system, which is based on 1) putting the needs and values of PeaceHealth patients and community at the center of care at the right place and right time; 2) fostering care driven by quality expertise; and 3) achieving accountable financial sustainability. We keep the individual and what they value the most at the center of this work: life on their terms the way it was intended.
Palliative care's philosophy rebalances medical care by moving from its traditional focus on disease treatment to the inclusion of whole-person and family care informed by palliative care principles. A key component to making palliative care changes at PeaceHealth is beginning with this philosophy and moving to evidence-based practice standardization. Standardized evidence-based practice is a cornerstone of patient safety and a fundamental principle of excellent health care quality. Unfortunately, it is often not translated into accountable health care processes and system design in an organization's structure and culture because change in this industry is rapid, constant and often unpredictable. This results in poor relationship-building and communication, factors necessary for meaningful change. Processes and approaches usually differ significantly among health care providers, practices and organizations. According to the Institute for Healthcare Improvement, standardization is fundamental.6 However, it is challenging in health care because of the complex relationships between a wide range of organizations, professionals, patients and caregivers.
The proposed action of PeaceHealth's system-wide palliative care initiative is a three-year, four-phased approach to performance excellence: pre-design, design, implementation and sustain. The overall goals are for the PeaceHealth palliative care programs to establish themselves as a sustainable model of service lines across the system, integrated as a fundamental component in the continuum of care. The overall objectives are to: standardize, align and integrate with local variation considerations, the palliative care clinical model(s) and operational processes; sustain standardized budgeting and resource allocation; and secure profitable value-based contracting agreements.
Our strategic blueprint is based on the national, regulatory and quality evidence-based standards, guidelines and national resources for medical palliative care to meet the requirements for the following:
- The Joint Commission's advanced palliative care program certification guidelines.7
- National Consensus Project for Quality Palliative Care's Clinical Practice Guidelines for Quality Palliative Care, 4th edition.8
- Twelve operational domains of palliative care outlined in Framework for Preferred Practices for Palliative and Hospice Care Quality: A Consensus Report.9
- The Palliative Care Quality Collaborative registry.10
- • The Center to Advance Palliative Care.11
In the first six months, the project began with a comprehensive gap analysis that identifies variations from the national clinical quality and regulatory standards required of palliative care programs. The foundational pillars of the health system's palliative care programs will go through a standardization process of analysis, design, implementation and sustainability, including: educational competency, program models, operational and clinical practice domains, electronic medical record documentation, centralized data collection, billing, productivity, quality metrics dashboard reporting and financial return on investment projections.
While standardization is important, it is also not a one-size-fits-all approach, and resistance to change can be a common barrier. To inform our work, we are completing specific interviews and engagement surveys. Participants include corporate leaders, physicians, nurses, social workers and chaplains, in addition to PeaceHealth patients through public surveys. These support greater awareness and a tailored approach to maintain the integrity across all provider settings and the communities they serve. A formal process for gathering stakeholder input about their priorities and design advice will help ensure successful startup and sustainability, while meeting health care system priorities and providing a unique approach regarding the service to their communities. One particular inquiry that cuts across all care settings is, "What keeps you up at night?" We hear personal stories from the heart which can help shape change in addition to the data gathered.
THE HEART OF PALLIATIVE CARE: WHAT MATTERS TO PATIENTS MOST
All clinicians have the responsibility to improve outcomes and provide person-centered care for those with serious illness, but many have not received extensive palliative care training.13 To provide patient-centered care, clinicians must understand their patients' hopes, fears, goals and preferences.14 When treating patients whose needs are most complex, many clinicians are uncertain about when to request a palliative care consult, while others lack access to board certified palliative care specialist teams. Furthermore, more than 70% of physicians report having no formal training in how to have compassionate and effective advance care planning conversations.15
PeaceHealth has identified education, training and practice change tied to specific outcomes as foundational to this effort and will know it's working through measures such as improving readmission rate and decreasing emergency room visits and mortality rate. To support education and training for its team members, PeaceHealth has invested in membership to the Center to Advance Palliative Care to offer employees access to online educational modules,16 toolkits, resources and materials, in addition to forming collaborative partnerships with national organizations and leaders in the field such as Ariadne Labs17 and Respecting Choices.18
PALLIATIVE CARE WITHIN THE PANDEMIC
The sudden and unprecedented increase in seriously ill patients with COVID-19, further compounded with the lack of core palliative care training and expertise among frontline providers and the palliative care workforce shortage, produced an immediate challenge.19 PeaceHealth's investment in expansion of its palliative care program demonstrates that this support is now the standard expected by patients with serious illness and those caring for them. Palliative care has been expanding within emergency rooms and ICUs and through investment in additional telehealth, making it accessible for more people everywhere to engage in this service no matter where they live. However, COVID-19 has been a source of exhaustion, moral distress and grief; therefore, we also are addressing team health to promote resilience and prevent burnout.
Furthermore, as we anticipate our programs and staffing to increase, we continue to add and identify national resources and proactive steps palliative care teams can take to promote caregiver wellness.20 We support each other with coping strategies such as nurturing physical, mental, emotional and spiritual needs; encourage taking time away to recover; and to focus on personal time. Support is available from employee assistance programs, counselors and spiritual providers. Daily huddles also provide an outlet to share joy and grief while acknowledging contributions, accomplishments and shout-outs that reinforce team values and healing from laughter. As a team, we acknowledge feelings of loss and suffering related to specific cases, and we conduct team debriefs. Overall, we strive to always foster a high-trust culture and to be respectful. The practice of empathy and showing our human side is essential. In our culture, it is OK to admit that everyone is struggling during a time of high demand and seemingly constant change, and we encourage communication.
PeaceHealth's palliative care initiative is more than just standardizing best practices: it is a unifying force for a close look at enhancing care. Palliative care is core to PeaceHealth's commitment statement "providing quality and compassionate care, every time, every touch. We care for the whole person, acting with kindness, respect and providing services that are high-quality, safe and patient centered."
MARIA GATTO is system palliative care consultant, PeaceHealth, Vancouver, Washington. She works with health care systems in standard–izing and implementing palliative care programs while meeting regulatory requirements.
BRYAN STEWART is a contributor to this article. He is system vice president, home and community, PeaceHealth, Vancouver, Washington, whose department supports home health, hospice, palliative care and home infusion.
NOTES
- "What Is Palliative Care?," Get Palliative Care, https://getpalliativecare.org/whatis/.
- Amy S. Kelley and Evan Bollens-Lund, "Identifying the Population with Serious Illness: The 'Denominator' Challenge," Journal of Palliative Medicine 21, no. S2 (March 2018): S7-S16, https://doi.org/10.1089/jpm.2017.0548.
- Peter May et al., "Economics of Palliative Care for Hospitalized Adults With Serious Illness: A Meta-analysis," JAMA Internal Medicine 178, no. 6 (June 2018): 820-29, https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2678833.
- R. Sean Morrison, "Palliative Care Consultation Teams Cut Hospital Costs for Medicaid Beneficiaries," Health Affairs 30, no. 3 (March 2011): 454-63, https://www.healthaffairs.org/doi/10.1377/hlthaff.2010.0929.
- "The Positive Financial Impact of Hospital Palliative Care," Center to Advance Palliative Care, https://www.capc.org/positive-financial-impact-hospital-palliative-care/.
- Robert Lloyd, "Standardize Before You Improve," Institute for Healthcare Improvement, July 3, 2018, http://www.ihi.org/communities/blogs/standardize-before-you-improve.
- "Palliative Care Certification," The Joint Commission, http://www.jointcommission.org/certification/palliative_care.aspx.
- "Palliative Care Guidelines," National Coalition for Hospice and Palliative Care, https://www.nationalcoalitionhpc.org/ncp/.
- David E. Weissman and Diane E. Meier, "Operational Features for Hospital Palliative Care Programs: Consensus Recommendations," Journal of Palliative Medicine 11, no. 9 (November 2008): 1189-94, https://doi.org/10.1089/jpm.2008.0149.
- "National Palliative Care Registry," Center to Advance Palliative Care, https://www.capc.org/national-palliative-care-registry/.
- "Welcome to the Center to Advance Palliative Care," Center to Advance Palliative Care, https://www.capc.org/.
- Rebecca Aslakson et al., "Evidence-based Palliative Care in the Intensive Care Unit: A Systematic Review of Interventions," Journal of Palliative Medicine 17, no. 2 (February 2014): 219-35, https://doi.org/10.1089/jpm.2013.0409.
- "The Case for Improving Communication and Symptom Management Skills," Center to Advance Palliative Care, https://www.capc.org/tools-for-making-the-case/.
- Terry Fulmer et al., "Physicians' Views on Advance Care Planning and End-of-Life Care Conversations," Journal of the American Geriatrics Society 66, no. 6 (July 2018): 1201-5, https://doi.org/10.1111/jgs.15374.
- "The Case for Improving Communication," Center to Advance Palliative Care.
- "CAPC Curriculum–Continuing Education Credits Overview," Center to Advance Palliative Care, https://www.capc.org/documents/546/.
- "Serious Illness Conversation Guide," Ariadne Labs, https://www.ariadnelabs.org/resources/downloads/serious-illness-conversation-guide/.
- "Respecting Choices," Respecting Choices: Person-Centered Care, https://respectingchoices.org/about-us/.
- Laura P. Gelfman, "Palliative Care as Essential to a Hospital System's Pandemic Preparedness Planning: How To Get Ready for the Next Wave," Journal of Palliative Medicine 24, no. 5 (May 2021): 656-58, https://doi.org/10.1089/jpm.2020.0670.
- "Team Health and Resiliency During the COVID-19 Pandemic," Center to Advance Palliative Care, https://www.capc.org/covid-19/team-health-and-resiliency-during-covid-19-pandemic/.