BY: MC SULLIVAN, RN, MTS, JD
EXAMINING DIVERSE PERSPECTIVES OF CATHOLICS ON ADVANCE CARE PLANNING, PALLIATIVE CARE, AND END-OF-LIFE CARE IN THE UNITED STATES
Untangling the Gordian Knot of Language and Attitude about Palliative Care and Advance Care Planning: Pathways to Convergence
 The centuries-old tradition of the Catholic healing ministry, carrying on the example of Christ found over and over again in the New Testament, has provided the language and myriad best practices for taking care of seriously ill people to the world of public policy on matters of health and health care delivery. Catholic health care's quality and reputation for dedicated commitment has attracted the attention and participation of many beyond the Catholic community. In their number are patients, practitioners, administrators, supporters, admirers and colleagues from the bedside to the board room to the communities served. They include colleagues in the policy world.
The centuries-old tradition of the Catholic healing ministry, carrying on the example of Christ found over and over again in the New Testament, has provided the language and myriad best practices for taking care of seriously ill people to the world of public policy on matters of health and health care delivery. Catholic health care's quality and reputation for dedicated commitment has attracted the attention and participation of many beyond the Catholic community. In their number are patients, practitioners, administrators, supporters, admirers and colleagues from the bedside to the board room to the communities served. They include colleagues in the policy world.
One such group is Pew Research Center, a subsidiary of The Pew Charitable Trusts, which has both observed and worked with individual practitioners and organizations from Catholic health care over the years. Pew Research staff frequently have engaged in conversations with groups like the Supportive Care Coalition, a national network of Catholic health care systems whose focus is the promotion and implementation of palliative care; the Catholic Health Association; and other Catholic health care organizations. Thus, the ongoing dialogue — sometimes formalized, more often serendipitous as we encountered each other at conferences and meetings — was in many ways unremarkable and somewhat routine.
The topics of these discussions very often were matters dealing with palliative care, advance care planning and end-of-life issues. Many of us run in the same palliative care circles and participated in these conversations. We were greatly interested in the number of times we experienced a "What did you say?" moment, or a "Really, you think that's what it means?" or "Why would you think or feel or speak that way about such-and-such topic?" exchange.
These reactive questions arose (or we found the answers becoming more and more interesting) because everyone asserted their positions or decisions to be based on — or in accordance with — church teaching.
How, many of us wondered, could colleagues draw on the same primary sources, the same corpus of canonical literature, but arrive at such different perspectives, judgments or decisions? It was an intriguing situation from an intellectual point of view, but from a practical point of view it could lead, perhaps, to some difficult and divergent moments in clinical or pastoral situations. The notion of digging into how people might arrive at substantively different decisions while asserting compliance with Catholic teaching was one that merited further examination and serious attention.
In August 2015, The Pew Charitable Trusts gathered a group of six Catholic ethicists who worked in and with the Catholic health ministry from a variety of perspectives. All of them served as resources to help organizations in the ministry remain faithful to and compliant with Catholic teaching. Serving as a kind of steering committee, this initial group sketched out a framework for a project that would look at three main topics in Catholic health care:
- The public nature or role of Catholic health care, which is a ministry done very publicly and receives a great deal of attention in the public eye;
- The nature of the relationship between and among the church and those it serves through their providers and organizations;
- The specific issues and decisions made by patients and families and providers in the setting of living with serious illness and, ultimately, dying from it.
Noticeably, these questions follow the same schematic framework and deal with most of the topics treated in Parts II, III and V of the United States Conference of Catholic Bishops' Ethical and Religious Directives for Catholic Health Care Services. This framework was intentionally constructed, and the ERDs served as the most primary of the project's primary sources. The other primary sources were papal statements (since the mid-90s when palliative care was established as a medical subspecialty, all three pontiffs to hold the office have promoted it and exhorted its implementation in the care of the seriously ill and the frail elderly); papal encyclicals; pastoral letters; and Catholic social teaching.
Three work groups, each moderated by two co-chairs, met six times. At the conclusion of the work group meetings, the co-chairs presented their findings to a gathering of all three groups plus the steering committee for a plenary session or summit during which observations, questions, issues and concerns were raised for discussion by all of the project participants. Areas of divergence and areas of convergence were specifically pointed out.
The report that follows captures the observations, thoughts and ideas expressed during the summit meeting. The project and its participants do not speak for any agenda or with any notion of being authoritative, proscriptive or prescriptive.
MC SULLIVAN is chief health care ethicist for the Archdiocese of Boston and director of its Initiative for Palliative Care and Advanced Care Planning.
 ATTENTIVE CARE for the seriously ill and dying is an essential part of the church's mission. This commitment flows from Gospel teaching, as evidenced by the early Christians' care for victims of plagues, the founding in the fourth century of the earliest "hospitals," the formation of religious orders to care for the sick and dying, and the eventual spread of Catholic-sponsored health care institutions across most parts of the world. From the beginning of the church, service to the poor, the hungry, the sick and the dying has been a mark of the Christian in the world.
ATTENTIVE CARE for the seriously ill and dying is an essential part of the church's mission. This commitment flows from Gospel teaching, as evidenced by the early Christians' care for victims of plagues, the founding in the fourth century of the earliest "hospitals," the formation of religious orders to care for the sick and dying, and the eventual spread of Catholic-sponsored health care institutions across most parts of the world. From the beginning of the church, service to the poor, the hungry, the sick and the dying has been a mark of the Christian in the world.
Persons serving in the Catholic health care ministry have embraced this mission today and continue to carry it out by working cooperatively with a wide variety of people with diverse convictions and perspectives, who are nevertheless devoted to the dignity and care of the human person. However, among Catholics, there are differences in the understanding and application of church teaching about care for those at the end of life, within and beyond pastoral and ecclesial settings, within Catholic health care and in the public square. Such differences can have significant impact on how issues of advance care planning, palliative care and shared decision-making in the final chapters of life are perceived, interpreted and acted upon. Further, the current culture and practice of American health care poses both challenges to and opportunities for the ministry of palliative care and the ethical guidance it offers for end-of-life decision-making.
Pathways to Convergence, a project supported by The Pew Charitable Trusts, enabled a broad array of clergy, clinicians, practitioners and ethicists to explore Catholic perspectives on these issues for more than a year. Participants engaged in a series of in-depth conversations on how Catholics accompany the sick and dying, how end-of-life medical decisions are made and what role the church has in promoting its message and vision in the public square. It was acknowledged at the outset that although Catholics share many strongly held views that converge, they also hold divergent views and practices that cause confusion and misunderstanding. The project was established with the hope that, through a respectful exploration of the convergence and divergence of views, participants could recognize a path forward that would enable Catholics to speak more clearly and distinctly about these issues to one another and to others as well. The effort was intended to confirm common affirmations, recognize divergences and offer proposals to improve understanding and increase the clarity of the church's common witness and the strength in its ministry and service, particularly in the areas of palliative care and support for advance care planning, where its influence may be viewed as increasingly prophetic.
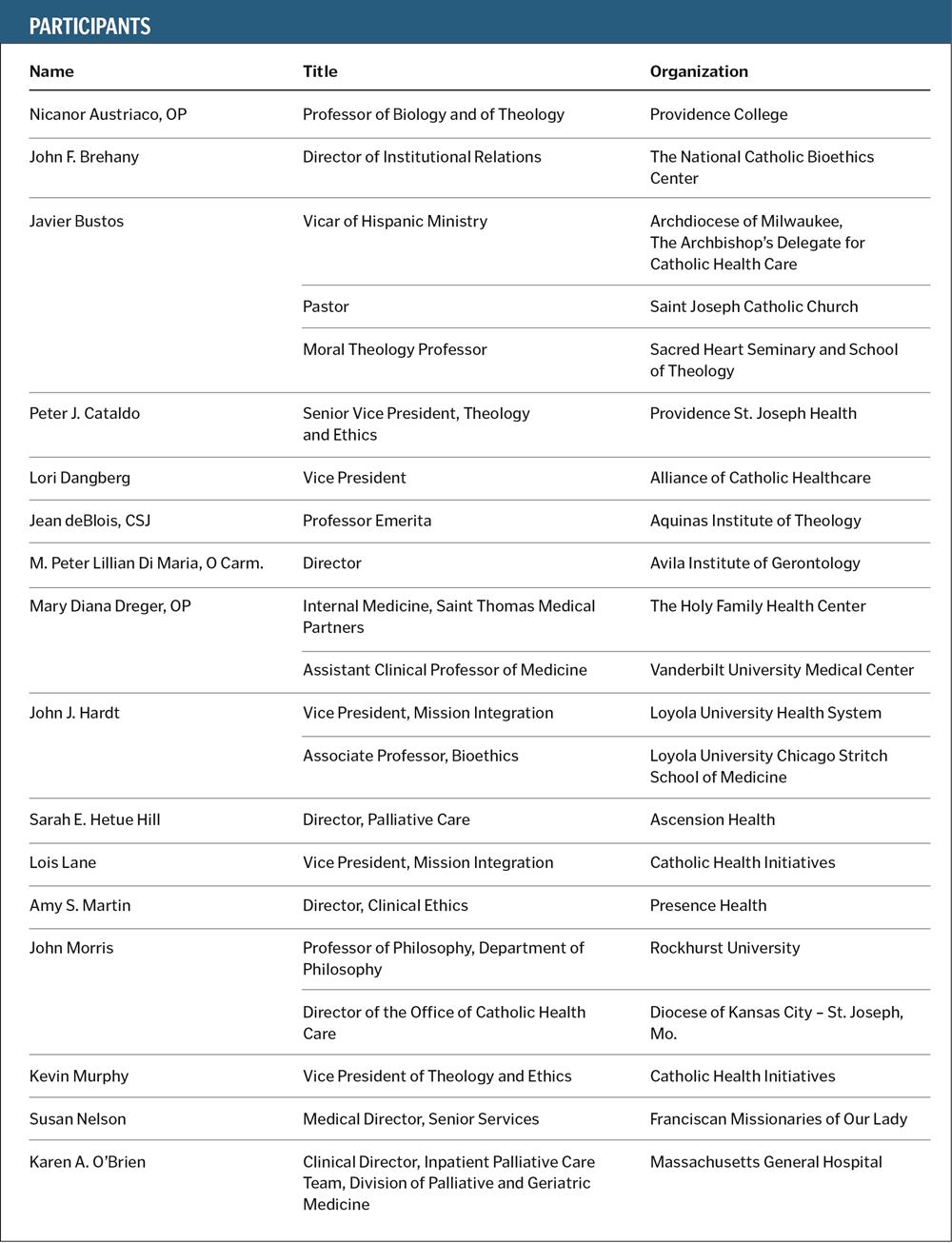
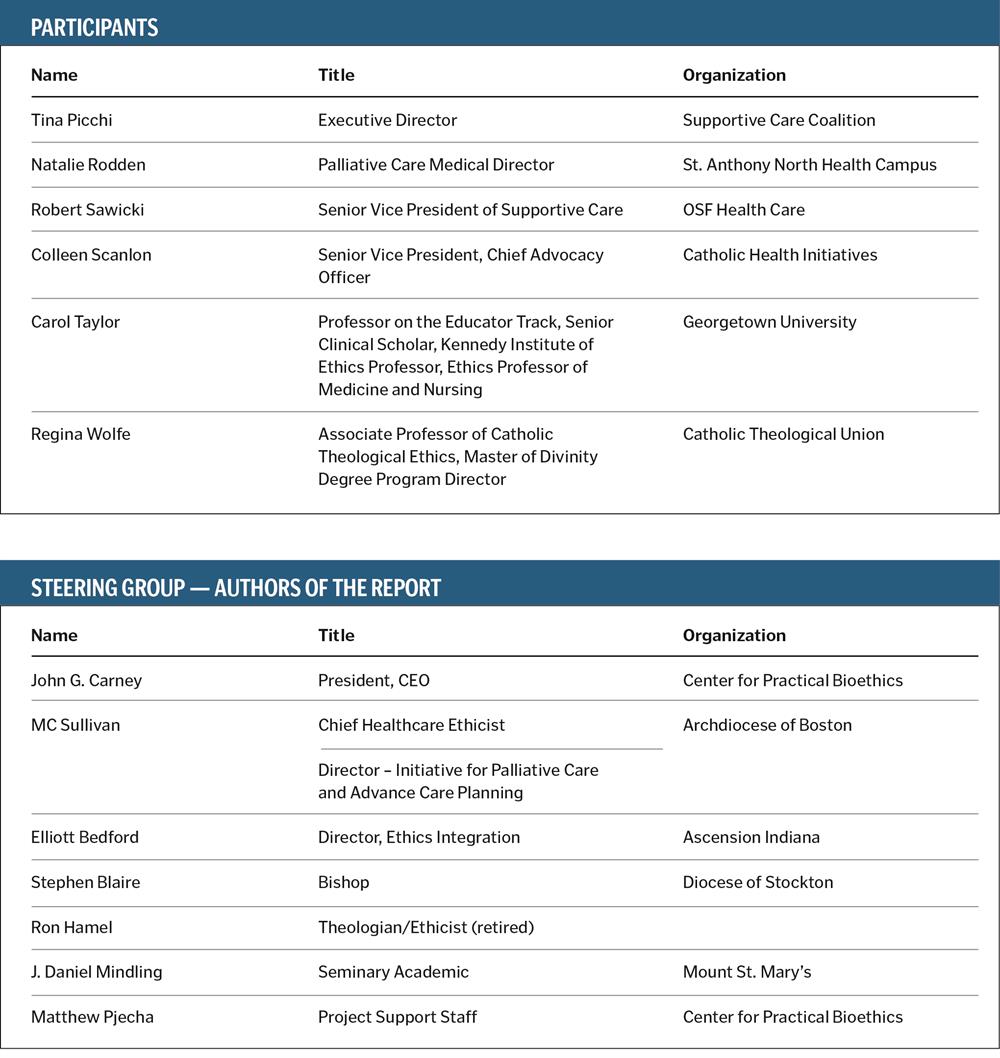
During the initial formation of Pathways to Convergence, a small group of leaders established a steering group that independently designed and directed the effort. That initial group soon identified an additional two dozen leaders from diverse professional perspectives, educational backgrounds and geographic regions to join in the work. Working groups were established in three areas: the public square, the moral tradition and clinical practice, with co-leaders named to facilitate each work group. These work groups sought first to identify areas in which there was a convergence of understanding and application of church teaching to palliative care and end-of-life decision-making. They also sought to locate points where there were divergent views or applications in practice. After a series of six online sessions that involved structured and open-ended dialogue over a three-month period, the work groups brought the results of their deliberations to a day-long meeting of the entire group in Chicago. This conference was a collegial exploration of the intersection of Catholic theory and practice on advance care planning, palliative care and shared decision-making during the final chapters of life as it pertains to both the clinical and public arenas. The appendix lists the participants and their affiliations.
This report seeks to faithfully capture and represent the main themes from a robust, wide-ranging and candid discussion by the participants at the Chicago meeting and serve as a catalyst for further collaborative dialogue within and beyond the church on these important matters.
 CULTURAL CONTEXT
CULTURAL CONTEXT
Participants noted that commonly used phrases or terms often are reinterpreted in the current health care delivery environment and within society at large. The meanings of "human dignity," the "dignity of the person" or even the "sanctity of life" have become muddled. Many participants also agreed that the voice of Catholics and the church on end-of-life care often is muted, misunderstood and occasionally dismissed when it is raised to affirm that the life of every person has value, no matter how incapacitated or dependent the person becomes. This affirmation is commonly referred to within Catholic teaching as the inherent dignity that emanates from recognition that humans are "created in the image and likeness of God." An increasingly secular culture, however, associates or even equates dignity with independence and autonomy.
Catholic palliative care takes a different perspective, recognizing "gratuitousness";1 that life is a gift and that we are stewards of the gift. For Catholics, the religious belief that holds "God is the Lord of life" is based on the commandment "Thou shalt not kill." It stands in contrast to what secular culture values: placing primary emphasis on personal choice or, within a cultural context, an individual's autonomy over stewardship. Catholic teaching and practice are based on recognizing the dignity of each person, the gift of human life, the social nature and solidarity of all humankind and the authentic common good. Many within the church believe this view of solidarity is marginalized or even interpreted as a threat by those who champion "individual freedom."
Beyond the tensions posed by the values of personal choice and solidarity in end-of-life decisions, effective palliative care and, especially, hospice care can be seen as proposing a conflicting set of values. On one hand, the embracing of a culture of autonomy holds that the denial of death may judge the discontinuation of treatment as a failure of medicine, reinforcing the "rights" of persons to continually seek aggressive curative measures. Pathways participants readily acknowledged this assumption as a hurdle in effectively fostering conversations and family-supported discernment of end-of-life care options. Simultaneously, this denial-of-death culture counterintuitively fosters autonomy through aid in dying, as some states recently have legalized what are commonly referred to, in secular terms, as death with dignity laws.
Participants recognized that advocacy of palliative care demands greater clarity of the wording we use. It must confront deliberate confusion over terminology (e.g., assisted suicide versus death with dignity) as well as a cultural drift that emphasizes autonomy in a way that diminishes the attractiveness of accompaniment and palliative care. Educational efforts with providers, ethicists, Respect Life leaders, ecclesial representatives and theologians will require collaboration, sustained communication and professional updating on the science of palliative care, as well as jointly hosting public relations efforts in the public square.
The recent weakening of formal positions against assisted suicide by some professional membership organizations at state and national levels has raised serious concerns among some Catholic writers. Those authors have leveled charges that the shifts from official positions opposing assisted suicide to "do not support" or "studied neutrality" in essence undermine those who maintain absolute opposition. Others worried that it might contribute to the misperception that palliative care is nothing more than "stealth euthanasia." In discussing the charge levied by the writers, however, Pathways participants did not endorse this argument. They acknowledged that leveling the claim, and its acceptance in some circles, underscored the need for greater clarity in what defines and distinguishes palliative care, along with the call to more clearly present the distinct Catholic perspectives and positive arguments for the benefits it offers.
For Catholic health care providers and policy advocates to respond effectively to these concerns about physician-assisted suicide, we need a more complete understanding of the cultural context from which such concerns arise. Patient autonomy, personal choice and quality of life deserve consideration, but they must be understood as part of a broader context of church teaching that is not widely understood. To achieve a better understanding of what autonomy, choice and quality of life mean, a concerted effort must be undertaken (i.e., to properly reflect how a Catholic understanding can effect a positive change for clinicians, policymakers and, particularly, the "people in the pew").
Pathways participants conceded that, although evidence is anecdotal and inferential, there is, for some, a kernel of truth to these claims. Examples of allegations of misuse include inappropriate use of opioids or withholding food and water. Unfortunately, allegations of such abuses and associations have fostered a limiting defensiveness, a fear and caution, even incorrect generalizations about what palliative care actually is. These concerns give rise to calls for greater "protection of life," so much so that a label of "vitalist" has been assigned to some proponents.
Vitalism holds that the preservation of human life is an absolute imperative in every case, regardless of moral consideration of futility or burden. Palliative care professionals must balance these views against the long-standing tradition of the church that recognizes the sacredness of life but does not hold that the preservation of human life has absolute value. Concerns about treatments, however, may lead to delays in appropriate and beneficial palliative care. While those who call attention to the potential risks in limiting treatments should be heard, their call affirms the need for vigilance among Catholics and for redoubling the demand for greater leadership in promoting authentic palliative care that truly respects human dignity.
 PALLIATIVE CARE
PALLIATIVE CARE
Pathways participants saw benefit in working from the World Health Organization (WHO) definition,2 which appeared comprehensive and compatible with the Ethical and Religious Directives for Catholic Health Care Services, 5th ed. They endorsed Pope Francis' description: "Palliative care is an expression of the truly human attitude of taking care of one another, especially of those who suffer. It is a testimony that the human person is always precious, even if marked by illness and old age. Indeed, the person, under any circumstances, is an asset to him/herself and to others and is loved by God. This is why, when their life becomes fragile and the end of their earthly existence approaches, we feel the responsibility to assist and accompany them in the best way."3 Palliative care thus provides us with a new opportunity to love those in need.
Pathways participants expressed some diverse (and at times divergent) nuances around the idea of palliative care. They embraced the idea that such care should really begin at the first medical encounter in the presence of serious or chronic illness. Some opined that a distinctive Catholic approach to palliative care optimally should include the intentional formation or support of a community of discernment or a community of care around a plan of compassionate care. Palliative care includes the formulation of such a plan.4 A number of participants spoke about how palliative care can embody a pastoral theology of accompaniment that should characterize a Catholic approach.5 A few raised a strong voice that accompaniment should reflect a pastoral theology of invitational evangelization, suggesting that those to whom we offer palliative care should be invited, even explicitly, to an encounter with Christ in order to find meaning in their life and to see the reality of redemptive suffering that is available only through him. Participants also discussed divergent ways in which the palliative care team can offer spiritual care and witness the presence of Christ, who accompanies the sick and dying.
After exploring the language of "good death," or even "holy death," the group did not embrace the terms. Instead, several participants referenced physician Ira Byock and the language of "dying well" as properly expressing the way in which death can become meaningful to the patient and family.6 Many participants found resonance with the "Whole Person Care Initiative of the Alliance of Catholic Health Care and the California Catholic Conference of Bishops."7 This project creates closer working relationships between Catholic health care and parishes in providing a ministry of whole person care so that "persons in our congregations, communities and hospitals are loved, wanted and worthy and will be prepared for and supported in health and serious illness through the end of life."8
There was general convergence and even enthusiasm around the prophetic witness that palliative care provides, not merely as a counter to those who claim that compassion means sanctioning assisted suicide, but as a fundamentally positive call to action affirming our duty to offer compassion to all those who are suffering and dying, because they bear the image of God.
Pathways participants also acknowledged the questions raised by a new population of those seeking legal assisted suicide. This includes the morally complicated and clinically complex issue of voluntary stopping of eating and drinking.
Two different groupings of the Canadian Bishops have offered statements in response to assisted suicide legislation in their country. They have taken divergent approaches to the accompaniment of individuals and their loved ones in this tense environment.9
Pathways participants concluded that compassionate accompaniment means there is an obligation to act as companion, not as an accomplice to either a fear-based vitalism or the plea for assisted suicide. On this matter, there is no conscience-neutral stance. Catholic principles of moral cooperation offer crucial guidance in challenging situations of accompaniment.
ADVANCE CARE PLANNING
 Pathways participants strongly affirmed the significance of advance care planning as both compatible with church teaching and an important component of appropriate palliative care. The group noted that Catholic tradition supports a provider-patient relationship characterized by a social discernment model of advance care planning rooted in the virtues of counsel and prudence. Such social discernment entails all stakeholders involved in care planning to continuously re-evaluate circumstances amid the progression of disease, revisiting decision-making and goals of care accordingly. This ongoing "re-visioning" process stood in contrast to the culturally dominant model in which the isolated patient is an autonomous individual making decisions based on purely informational consultation with providers and family. In the latter model, the patient's plan is to be implemented by the care team and family, regardless of circumstances.
Pathways participants strongly affirmed the significance of advance care planning as both compatible with church teaching and an important component of appropriate palliative care. The group noted that Catholic tradition supports a provider-patient relationship characterized by a social discernment model of advance care planning rooted in the virtues of counsel and prudence. Such social discernment entails all stakeholders involved in care planning to continuously re-evaluate circumstances amid the progression of disease, revisiting decision-making and goals of care accordingly. This ongoing "re-visioning" process stood in contrast to the culturally dominant model in which the isolated patient is an autonomous individual making decisions based on purely informational consultation with providers and family. In the latter model, the patient's plan is to be implemented by the care team and family, regardless of circumstances.
The discernment model relies on a convergence that shared decision-making ought to be promoted, as long as it respects the proper responsibilities and boundaries of each stakeholder, e.g., patient, family, provider. At the same time, participants noted that disagreements about what shared decision-making looks like in practice might be a source of divergence.
A paramount necessity, Pathways participants agreed, is a well-formed conscience provided with adequate education and discernment. It empowers patients and families to make sound prudential judgments in advance care planning and end-of-life decision-making. The group affirmed that medicine is a probabilistic, inexact science; consequently, advance care planning and decision-making always should be placed in context and prudent in nature. Limitations of certitude play a large role in real-life decision-making, and participants recognized that limited certitude may lead to divergence around how individuals might apply the principles of the church's teaching in their lives. There was, nevertheless, strong convergence and agreement on Catholic teaching and principles for end-of-life care and decision-making, but some divergence on their application in particular situations.
There was strong convergence that to help people develop well-formed consciences, the church's teaching and tradition related to palliation and end-of-life decision-making needs to improve dramatically among the general church membership, from those in the pew, to clergy and bishops, to Catholic clinicians themselves. Further catechesis is necessary to help people in their prudential judgments. Finally, there was divergence on how or if one could adhere to the guiding principles of cooperation while at the same time practicing compassionate, invitational accompaniment.
Though there are many tools for documenting well-formed advance care planning decisions, Pathways participants recognized that too few do anything more than serve as tools to comply with state law health care directives, or appointing an agent and clarify instructions. A noticeable convergence arose around the value of having advance care planning tools that can communicate the patient's values and preferences to be considered in the assessment of interventions (e.g., resuscitation or feeding tube) and thereby help avoid concerns raised by diminishing or episodic capacity or in situations of hurried decisions during crises.
Some participants described positive experiences around the use of Physician Orders for Life Sustaining Treatment (POLST) forms worked out in close collaboration with practitioners and church leaders. At the same time, others raised specific concerns and points of divergence about POLST initiatives, where forms vary state by state. Points of divergence arose around:
- Whether POLST forms are helpful or problematic
- Whether it is prudent to include (as current forms do) crisis and nonrescue (limited) interventions on an immediately actionable document
- Whether there is consistency in the model itself (since forms vary by state)
- Whether the tool is being used consistently across delivery settings
- Whether it is being used voluntarily, as intended
- Whether it is targeting those for whom it is designed (a select patient population nearing the end of life)
- Whether abuses of the instrument in fact ought to invalidate its continued implementation and use
There was, however, convergence that documents and tools that would preclude or eliminate the exercise of clinical judgment or prudence would not be consistent with the Catholic tradition.
 SOCIAL RESPONSIBILITY
SOCIAL RESPONSIBILITY
The social responsibility role of the church and individual Catholics to promote a clear vision of palliative care and end-of-life care was widely affirmed. The group recognized that, given the complexity of the church, Catholics may have different roles and responsibilities for advancing this message.
Catholics are called to speak and act as Christians who are committed to dignity of the human person and sacredness of human life. This responsibility is vital as Western society continues to secularize, in breadth and intensity, in a way that negatively impacts care for the poor and the vulnerable. Catholics have a role to inform society, not just those among the baptized.
Catholics also are called to speak and act as a church, affirming the distinct roles each and every one has — a unified church amid diverse adherents. Recognizing that individual, situational, role-specific diversity of individuals and groups within the Catholic community may also give rise to points of divergence, Catholics can identify opportunities to better understand those divergences and deliberate on how to leverage such diversity to advance palliative care.
Catholics have an equal responsibility to act as diligent citizens. According to their individual role, Catholics should be adequately educated about the church's vision of palliative care and how it should be promoted, both within the church and within their respective local community. This responsibility is especially significant among those who can impact societal change, including health professionals and political leaders.
As caregivers, Catholics have a similarly important role. Among their communities, families and friends, individuals can educate themselves on important topics such as advance care planning, palliative care and related church teaching. And while myriad resources exist, both Catholic and non-Catholic, greater emphasis and intentionality should be given to helping guide caregivers in gaining greater understanding in these shared decision-making matters. All affirmed the significant opportunity to educate caregivers and capture their voice.
In every instance, living out this social responsibility means placing an emphasis on a prophetically pastoral Catholic voice. In both the indicative and the imperative, this voice must speak and seek the truth: affirming the dignity of all, including the marginalized and frail; accompanying them in their suffering; vigilantly rejecting despair and condemning the dehumanizing practices of suicide and euthanasia; researching, developing and improving care techniques, models and care planning tools; proclaiming that suffering and death are realities filled with meaning, especially in light of Christ's own redemptive death and resurrection. Participants recognized that such a grounded but multipronged approach will find challenges in a secular pluralistic society, wherein the notion of "truth" itself often is a point of strong divergence.
Furthermore, strong cultural currents in the public square raise serious questions for Catholics and the church to reflect upon and discern. For instance, political movements such as "Aid in Dying" are driven by nationally identifiable faces and narratives that assert assisted suicide is a compassionate approach to treat the suffering and dying. Do Catholics adequately give voice to an alternative narrative that expresses the comfort and meaning that palliative care provides? How can and should this message be fostered and proclaimed in a way that is personally meaningful and has an impact on broader society? Is this vision being discussed within Catholic schools of medicine and law? Is there dialogue with workers in Catholic health systems, or is this discussed only among thought leaders like those in the Pathways meeting? The participants' strong agreement that the church maintains a role in promoting its vision in the public square indicated that such questions cannot and should not be left unaddressed.
There was some divergence about what is or ought to be said in the public square, both in terms of message and style. Some participants favored strong statements in opposition to assisted suicide. Others emphasized, even in taking a stand in opposition, that a more positive approach and tone, focused on understanding the suffering of those seeking or advocating for assisted suicide, might be more readily received in the public square and lead to more potential collaborations.
Without hesitation, all agreed: More dialogue is needed, both within the church and between Catholics and society, so that Catholics and the church are better informed, more clinically and socially coordinated and society is improved through better access and use of palliative and end-of-life care.
MOVING FORWARD
The participants recognized that neither the process nor the proceeding was comprehensive or exhaustive of the range of questions and issues the church faces as it seeks to advance its vision of palliative and end-of-life care. Within the dialogue, however, certain points emerged clearly:
- Participants recognized that palliative care and end-of-life decision-making faces the challenge of medical specializations that make holistic care both more challenging and, at the same time, more necessary. Palliative care is coordinated and intentionally holistic care.
- The group recognized that we need education within the church and clarification of policies and programs within the diverse community of providers, as well as publicity and community education efforts outside the church. The language we have been using is not enough.
- It emerged in our discussion of various forms of POLST in use throughout the country that there still is unresolved tension between proponents and opponents. Many participants were eager to bring the voices of practitioners to these discussions.
- It emerged that the language about end-of-life decision-making frequently focuses on prohibitions of unethical behavior. The group called for a change in tone to give voice to the positive and life-affirming nature of palliative care, the formation of a community of discernment and loving accompaniment at the end of life.
- While the church has a helpful and rich corpus of teaching on matters related to palliative care, the diverse roles, circumstances and perspectives of Catholics entail that an element of diversity and divergence among Catholics is to be expected, especially on matters of practical application, such as POLST. This diversity can be mutually beneficial and internally enriching, as it can help deepen insight and nuance understanding within the church. Further, participants recognized that Catholic support for palliative care was not novel but integral and long-standing to the operations of the Catholic health care ministry in the United States. Moreover, due to this long-standing commitment, Catholic health care providers and individuals are eager to advance and grow palliative care efforts.
Given these emerging insights, the participants considered a number of proposals for how the Catholic community might move the conversation forward. A significant concern about language clarity led to recommendations that documents, especially the Ethical and Religious Directives for Catholic Health Care Services, might be revised and updated to include more explicit and more lay-oriented language in affirmative directives regarding hospice and palliative care.
The identified desire for further sustained, intentional dialogue within the church gave rise to additional proposals. First, that a formal organ for dialogue between the United States Conference of Catholic Bishops and Catholic health care providers, systems, associations and individual clinicians be established. Second, that clerics, theologians, clinicians, ethicists and others be invited to discuss and educate one another, contemplating a consensus-building "moral summit." This could provide a more formal expression to the church in the United States' voice on issues related to palliative care and end-of-life care. Above all, it was recognized that to effectively carry its message to the world, the church must be more intentional about fostering its own consistent dialogue and understanding of palliative care and end-of-life care. The Gospel and healing ministry of Jesus demand nothing less.
NOTES
- Benedict XVI, Caritas in Veritate, para. 34
- World Health Organization, "WHO Definition of Palliative Care." www.who.int/cancer/palliative/definition/en/.
- Francis, "Address to Participants in the Plenary of the Pontifical Academy for Life," March 5, 2015. https://w2.vatican.va/content/francesco/en/speeches/2015/march/documents/papa-francesco_20150305_pontificia-accademia-vita.html. See also Benedict XVI, "Message for the 15th World Day of the Sick," Dec. 8, 2006. http://w2.vatican.va/content/benedict-xvi/en/messages/sick/documents/hf_ben-xvi_mes_20061208_world-day-of-the-sick-2007.html.
- John Paul II, "Address to the Participants in the 19th International Conference of the Pontifical Council for Health Care," Nov. 12, 2004. https://w2.vatican.va/content/john-paul-ii/en/speeches/2004/november/documents/hf_jp-ii_spe_20041112_pc-hlthwork.html.
- Here Pathways participants developed the image of Christ walking with the disciples on the road to Emmaus and the "art of accompaniment" as spoken of by Pope Francis. See Francis, Evangelii Gaudium para. 169. https://w2.vatican.va/content/francesco/en/accompantations/documents/papa-francesco_esortazione-ap_20131124_evangelii-gaudium.html.
- See Ira Byock, "Dying Well," http://irabyock.org/books/dying-well/.
- See Alliance of Catholic Health Care, "Palliative Care/End of Life." www.thealliance.net/index.php/palliative-care-end-of-life.
- "Palliative Care/ End of Life."
- The Catholic Bishops of Alberta and the Northwest Territories, Guidelines for the Celebration of the Sacraments with Persons and Families Considering or Opting for Death by Assisted Suicide or Euthanasia: A Vademecum for Priests and Parishes, (Edmonton: Catholic Bishops of Alberta and the Northwest Territories, Sept. 14, 2016). http://archgm.ca/wp-content/uploads/2016/10/2016-09-14_SacramentalPracticeinSituationsofEuthanasia.pdf?9910a6, and Atlantic Episcopal Assembly, "A Pastoral Reflection on Medical Assistance in Dying," Nov. 27, 2016. http://rcchurch.com/uploads/AEA%20%20Pastoral%20letter%20medical%20assisted%20dying.pdf.