BY: BETSY ADERHOLDT AND JEFF LOCKRIDGE
Historically, a "we versus them" relationship among many hospital administrators and physicians has bred mistrust and poor communication. Relationships became even more strained in the 1990s, after hospitals bought physicians' practices and then sold hundreds of them. In many cases, physicians responded by opening delivery centers of their own — competing outpatient surgery and imaging centers and specialty hospitals.
Today, though, change is in the air. Health reform's coordinated care delivery models, new payment arrangements and a stress on accountable care offer inducements for physicians and hospitals to put negativity behind them and move forward together. Physicians are seeking financial security through traditional and innovative compensation arrangements with hospitals, and hospitals are recognizing the need to partner with physicians to improve clinical outcomes and reduce inpatient costs — understanding that preventable readmissions, hospital acquired conditions and costs now may result in penalties.
Further, to position themselves as accountable care organizations (ACOs) and participate in bundled payment arrangements, providers need adequate physician participation. A survey of 1,000 physicians across the U.S. by PwC's Health Research Institute1 found that a large majority already have aligned financially with hospitals through employment, joint ventures or directorship, and most indicate they want to move toward an even closer relationship by participating in governance and leadership.
But physicians and hospitals, plagued by years of contention, may be ill-prepared for the close-knit relationships they will be entering, especially those that involve physician employment. At a minimum, cultural change and aligned incentives are needed for these relationships to work.
One form of physician-hospital alignment emerging as a model is a shared ownership known as co-management. Of the 1,000 U.S. physicians surveyed by PwC, 8 percent are already part of a co-management company. Genesys Regional Medical Center, part of Michigan-based Genesys Health System and the national Ascension Health, is among those organizations that are using this model as a component of its long-term vision to position itself as a "hospital of the future" — one in which administrators and physicians align and work together in carrying out the mission to extend the healing ministry of Jesus. Since physician investors of the co-management companies have become more engaged with the day-to-day operations of the organization and integrated into its strategic decision-making, their work has, in turn, become more aligned with advancing the mission of Genesys.
EMPOWERING SPECIALISTS
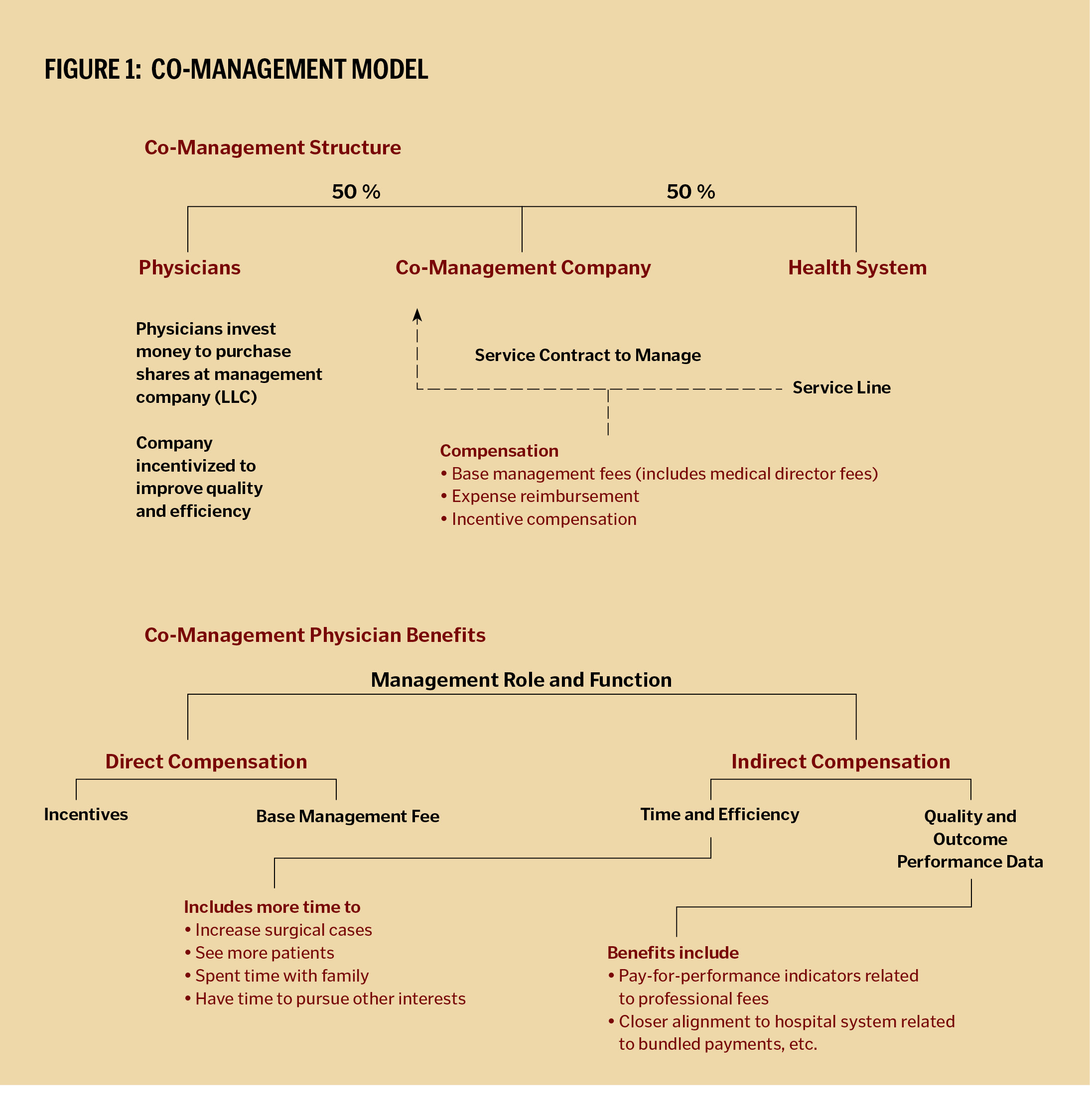
A co-management arrangement, illustrated by Figure 1, allows a hospital to contract with physicians and give them greater input and authority over quality and operational improvements. In exchange, physicians can be compensated for their role in managing a given service line as well as for the achievement of certain performance metrics. The results are more efficient operations, better patient care outcomes and more satisfied physicians, who have a seat at the table as decisions are made.
In this Michigan market, primary care physicians had been the ones contracting with third party payers through an established Genesys Physician-Hospital Organization (PHO). Although numerous PHO models across the United States were unsuccessful, Genesys, with 160 full-time-equivalent primary care physicians in its PHO, had enjoyed a decade of success with this model, based on risk-based capitated managed care contracts. Through "preferred provider panels" of specialists, the primary care physicians pre-selected which specialists they would work with. The primary care physicians, through the PHO organization, successfully worked on clinical care improvement teams and managed resources through effective control of admissions, length of stay and outpatient ancillary utilization. However, the primary care based PHO structure had not effectively engaged specialists in making improvements inside the acute care setting. While there was convenient access to 160 primary care physician referrals, often the specialists did not have much influence in strategic decision-making and felt marginalized. A divided culture was evolving, the upshot of which was gaps in trust and frustration on both ends as the providers lacked tools for engaging specialists in plans aimed at improving care.
Because strong specialist engagement is vital to improving both service line and overall health system performance, Genesys, in consultation with PwC's Health Industries Group, began to review various models for integrating specialists in the acute care setting. Whichever model was decided upon needed to be complementary to the primary care strategy, which Genesys did not want to disrupt. It was a goal to touch as many specialists as possible, with the fewest number of new arrangements. The two organizations believed the co-management model fit that bill.
The co-management model is a team approach to improving the quality of care. It drives physician leadership and ownership toward outcomes and quality goals, which ultimately results in a significant cultural shift in physician-hospital relationships.
The objective of the Genesys co-management model is to align with specialists to improve quality and efficiencies, which can ultimately benefit primary care physicians and the PHO. The model complements the PHO's primary strategy and allows Genesys to touch specialists across three service lines, cardiovascular; orthopedics, neurosurgery and podiatry; and surgical services — up to 250 specialists in all.
At Genesys today, both primary care physicians and specialists are happy with the co-management model. But that acceptance did not come easily. The idea of co-management, which involves the provision of leadership not clinical services, took the convincing of many people. A series of town hall meetings occurred to explore with the medical staff whether or not the model made sense. The primary care physicians were curious to see if giving specialists more of a voice in decision-making would affect their finances and their control.
Management went to great lengths to demonstrate the large upside potential for the primary care physicians and the specialists, with minimal risk. A co-management model was being put in place to improve quality, patient satisfaction, safety and operating efficiencies, and to position the health system for health care reform. Following a full year of communication as results materialized and the physician-management teams gained practice working together, the skepticism started to fade and the cultural issue began to resolve.
CO-MANAGEMENT SUCCESSES
Since the model was implemented by Genesys in July 2009, co-management has led to increased patient satisfaction, among other improvements. While some hospital departments' overall patient satisfaction scores didn't move as quickly, the scores for patient satisfaction with physician-related components improved dramatically at Genesys where co-management is used — in some instances, achieving the 99th percentile in satisfaction as compared to other hospitals in the country. In March of 2009, prior to co-management implementation, the cardiovascular department was at the 60th percentile and the surgical services and ortho-neuro-podiatry departments were each at the 23rd percentile.
Genesys' co-management companies have become among top performers nationwide, and the physicians are now actively engaged in patient satisfaction and improving scores within the Hospital Care Assurance Program(HCAP), one of the components of the CMS value based purchasing program.
Co-management also has helped educate physicians on how to improve processes and implement changes in the organization that lead to sustainable improvements. The hospital and physicians are now strategically positioned to begin piloting an ACO. Genesys can already demonstrate successes with sharing revenue between the hospital and multiple physician specialist groups through co-management. With contracts ranging from $1.5 million to $2.2 million, co-management has allowed Genesys to create a monthly co-management budget, show transparency in its financials (e.g., whether or not targets were reached), and create transparency on how money is being allocated and distributed.
In addition to the transparency co-management fosters, physicians in the market are looking favorably at Genesys because they are involved and helping to initiate change within the organization, change which improves care for their patients and creates work environments that are more "physician-friendly." In one example, the physicians are helping to build Genesys into a high reliability organization through the adoption of a new surgical safety checklist, based on the World Health Organization (WHO) Safe Surgery Checklist. The checklist is designed so that each necessary step must be completed before proceeding to the next phase of a procedure. During the period of September 2009 through December 2010, the surgical services co-management company operated on more than 8,500 patients and completed 98 percent to 100 percent of the WHO checklist requirements.
Furthermore, the success of the co-management companies is attracting interest from other specialties within the region, such as pediatrics. A number of pediatricians from other hospitals are taking notice and inquiring about opportunities with Genesys because their colleagues in the co-management companies are talking about a new culture of engagement and results at Genesys. Two prominent area pediatricians already have migrated to Genesys to strengthen its pediatrics program and are working with management to develop preliminary plans for a possible new co-management company that would include other pediatricians.
As participants in the co-management arrangement, specialists now have input into how things work, including the operating rooms and inpatient nursing units, which makes the working environment better for all physicians. Genesys has positioned specialists to be successful and survive in a difficult health care market in Michigan, which has high unemployment rates and a shrinking population — all of which affect a physician's patient volume. Cardiologists and vascular surgeons are using co-management as a recruitment tool to attract new physicians to the challenged market. This model creates a more efficient work environment for physicians and allow physicians to have more voice in strategic decision-making.
As a by-product of the physicians' involvement of co-management in service lines, they now understand how to be better leaders and managers. Co-management is transforming the culture of the medical staff by providing better understanding of what it takes to lead change processes across an organization. Furthermore, many physicians are going above and beyond to serve as ambassadors and bring national attention to Genesys and the co-management companies. In fact, the success of the Genesys co-management model has led to it being selected as one of the 12 leading health care practices throughout all of Ascension Health nationwide.
A MODEL FOR MISSION
Genesys has recently launched an educational program to teach other hospitals and health systems how to implement co-management companies, in which some of the investor physicians participate in presentations and panels to provide their insights and advice. Part of their advice to other facilities that are considering creating co-management: spend ample time up front, because it's a new concept and a significant cultural change for hospital and physician leadership. Governance, medical staff officers and the c-suite have to be ready to fully embrace the concepts of transparency and shared decision-making.
Physician-hospital alignment, when done correctly, can change health systems forever. But there needs to be an understanding of health care reform, state regulations and how the current market drivers will affect a health system. Modeling the reimbursement changes and new payment models will clarify all of the opportunities and associated costs with selecting a physician alignment strategy, whether for directorships, leasing, joint ventures or employment.
Vital communities with healthy residents are outcomes that hospitals and physicians should be working together and striving for now and most certainly in the future. In the case of Genesys, it helps to ensure the vitality of one of its community's largest employers, and most importantly, it helps to fulfill its mission of "creating hope through healing." This statement, articulated in 2009 and based on a survey of more than 100 Genesys representatives, including physicians, is rooted in Genesys' heritage as a ministry of Jesus. It reflects respect for the heritage of the organization's founders and its role as a Catholic health ministry.
As the Genesys case study illustrates, developing trust by means of sharing information and collaborating in governance are good first steps for any physician alignment strategy. In particular, since the Genesys co-management companies have proven to be effective at improving safety, quality and patient satisfaction, they represent a proactive model for health care providers to assure their mission thrives in these challenging times.
BETSY ADERHOLDT was president of Genesys Regional Medical Center in Michigan. She was recently named president and CEO of the Genesys Health System in Grand Blanc, Mich.
JEFF LOCKRIDGE is a director in PwC's Health Industries Practice. He is based in Indianapolis.
NOTE
- PwC Health Research Institute, From Courtship to Marriage Part I: Why Health Reform Is Driving Physicians and Hospitals Closer Together, December 2010. www.pwc.com/us/ACOalignment.
Copyright © 2011 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.