BY: ALAN PITT, MD, and CORY PITT
Illustration by Cap Pannell
Would You Share Information to Gain Better Care?
What if we told you that we could help you live three or five years longer — would you want to hear more? And what if we said that this gift wouldn't cost you a thing — that it involves neither surgery nor experimental drugs — all you have to give us is your data. All those likes, those posts, all those things you're doing anyway. Would you be willing to sacrifice some privacy so that you or a loved one could live a longer, healthier life?
This is a story about data: Where we've been, where we are and where we could go. Data is everywhere and offers huge opportunities for payers, hospitals, providers and ultimately patients to improve care and reduce costs. However, risk and responsibility accompany the reward.
DATA 1.0
Paper Records
The ubiquity of electronic medical records now makes it easy to forget the days when records were kept on paper. The rooms that housed these paper charts resembled Byzantine libraries, with shelves stacked to the ceiling with files. Consulting a chart to review a patient's history could mean pulling pounds of paper containing other clinicians' (often illegible) notes. Creating the charts wasn't much more pleasant: medical students could spend hours writing up a patient's history and physical examination findings. Senior physicians were known to cut corners and scrawl a line or two. Academic publishing required researchers to read through illegible or incomplete charts, and it often took months of legwork transferring information to another "database," usually an Excel spreadsheet, for further analysis.
Education, research and finding answers to patient conundrums required trips to the library. The actual, physical library! An early version of the scientific article database MEDLINE went live in 1971 and boasted 25 simultaneous users. However, it wasn't until the advent of the World Wide Web in the 1990s that we gained widespread access to medical literature. Until then, doctors were akin to oracles — the keepers of knowledge and experience inaccessible to the public. The web blew the doors off and the evolution to a paperless chart was inevitable.
DATA 2.0
Paper to Paperless
"Anything on paper is obsolete!" — Craig Reucassel, Comedian
Both health care software companies Epic Systems and Cerner were founded in 1979 (though they bore different names then). We reached out to Judy Faulkner, Epic Systems' founder and chief executive officer, and asked her whether a certain event precipitated the launch of two behemoths in the electronic medical record space, but she could recall no specific catalyst. Adoption of the medical records systems was slow at first. Cerner released its first product PathNet in 1984. The client base grew steadily.
A number of factors in the 1990s catalyzed the adoption of technical innovation. The personal computer drove electronic medical record implementation costs down. Government regulation further incentivized conversion to digital; in 1996, the Health Insurance Portability and Accountability Act (HIPAA) was introduced to improve health care coverage, privacy and security, and in 2003 a tipping point occurred — the managed care organization Kaiser Permanente adopted Epic. Today, roughly 90% of hospitals use computerized systems for medical records and other processes, and more than half of the American public has its medical records stored in Epic.1
Although it is clear that we won't be going back to paper records, the road to better care through technology hasn't exactly been smooth. Costs associated with electronic medical records include financial strain (which can exceed a billion dollars for large systems),2 endless infrastructure maintenance, and the drain on practitioners, doctors and nurses, who often feel more like data-entry drones rather than healers.
In his excellent article entitled "Why Doctors Hate Their Computers," Atul Gawande describes how the transition to electronic medical records was supposed to help, but in many ways ultimately fractured the doctor–patient relationship.Notably, when asked why clients adopted Epic in the early days, Faulkner confirmed that early adopters of Epic saw it as a way to improve patient care. Today, however, the decision to use electronic medical record systems is often made by committees and legal teams seeking to improve the bottom line and cover their bases. Clinicians are still involved, but administration and compliance teams typically have the final word. Holistic assessments of computer systems are rare, and decisionmakers often seem to overlook how new technology will affect every sector of an organization. Of course, the greatest cost for care delivery is staff! With electronic medical records, clinicians are working longer hours but are burning out quickly. These indirect costs are rarely included in the total cost of progress.
DATA 3.0:
Evolving into a Human–Machine Partnership
"One machine can do the work of 50 ordinary men. No machine can do the work of one extraordinary man." — Elbert Hubbard, Writer
Alan Pitt, one of the authors of this article, has written before about compassionate capitalism — essentially, we as a society will always take care of the sick and less fortunate, but to do so over the long term requires a business model. The justification for electronic medical record systems mostly relates to revenue reporting and quality issues; however, these are problems for health care systems, not for the providers who work there. Even though hospital systems ought to resolve the issues associated with electronic medical records, the deficiencies of the technology trickle down onto the everyday system users.
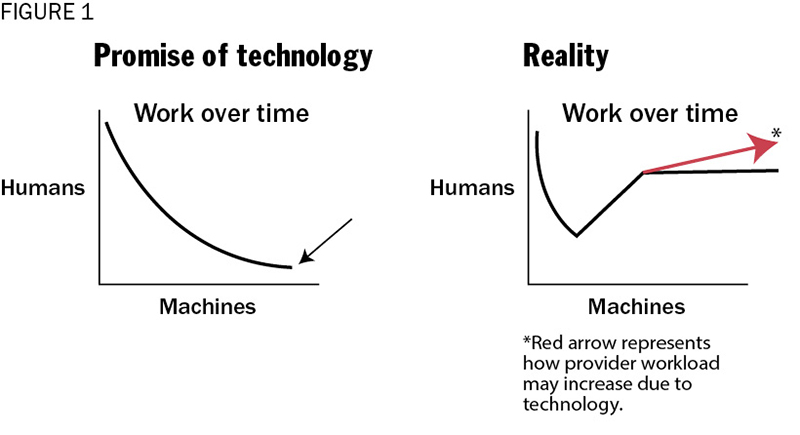
Another way to think about this is represented in Figure 1. The graph on the left captures the promise of automation. If you think about the multiple steps of a given task, machines should gradually take on more of the workload, freeing up time for humans to do what they do best — lead, talk, engage with other people — and humans also carry out the remaining portion of the task that cannot be automated (the small black arrow). However, the reality is often different. Monolithic systems, like electronic record systems in health care, are built to solve the hospitals' administration problems. Gaps are filled in by asking more of the workforce.
The graph on the right, meanwhile, more accurately reflects the reality. For example, doctors believe that it takes longer to see the same number of patients than before the adoption of electronic medical records, even though drug reconciliation and other information may offer a safer patient outcome. However, the institution has addressed revenue and quality issues by implementing the records system (often a major undertaking), so the institutional interest in additional investment or change tends to plummet. The user workload may grow as the platform provides opportunities for additional detail and quality reporting (red arrow). This increase in workload and decrease in job satisfaction is a recipe for burnout and, ultimately, employee turnover.
While Data 2.0 digitized data, the emphasis was on digitalization for administrative purposes — not for patient care. Data 3.0 seeks to rehabilitate attitudes toward data for hospitals, providers and patients. Data 3.0 is a powerful tool that not only allows for the analytic strengths of a machine, but that also leverages human behavior, creativity and intuition. But just as revenue and compliance drove electronic medical record adoption, Data 3.0 requires a business justification.
Spending double the amount spent by the rest of the developed world, American health care is moving from volume to value, or in general terms, from transactional care to care with greater focus on results. Cost-effective value-based care requires management of the whole population one patient at a time. Thus, the right resources must be applied to the right patient.
Let's explore Data 3.0 using an example. Let's say we have a 65-year-old retired hospital worker named Joe, who has congestive heart failure, a complex condition with four stages. Early on, congestive heart failure can be treated with lifestyle changes. As the disease progresses, it results in dietary restrictions, medications, and (rarely) surgical intervention. Patients with congestive heart failure may have low energy and, as fluid builds up in the lungs, many patients describe feeling like they are drowning. Home visits and remote patient monitoring are options, but they are expensive. Payers and hospital systems have to decide whether Joe needs these resources, but case managers can't always identify patients at greatest risk for readmission.
Back to Joe. His health has been good, but after a minor heart attack he started taking medications for high blood pressure and occasional chest pain. He sees a local doctor, but the visits are brief. He's started having difficulty walking far and suspects the new medication is a problem, so he stops taking it. He would love to ask his doctor more questions, but she's just so busy. He looks online, but Google search results are vague. One night, Joe feels like he can't breathe. He calls an ambulance and is taken to the hospital.
At the hospital, the doctors have none of Joe's records. Unaware of all the details of his medical history, they keep him in the hospital for five days. The doctors dutifully document in the electronic medical record, complete all discharge forms, prescribe Joe new medications, educate him on his condition, and direct him to follow up with his doctor.
A cardiac nurse is helping with hospital accreditation. She visits Joe but spends most of her time reading his chart and moving his data from the electronic medical record into her database, because she needs to do that as part of her job. She wishes she could get patients to weigh themselves every day, as fluctuating weight can be a sign that more intervention is needed and such care might help lower the 30-day readmission rate.
Joe goes home, but fills only four of the five new prescriptions — the co-pay was too high for one. He continues his previous diet, which is high in salt, and before you know it — he's back in the hospital. This time there is a financial penalty for the hospital from the Centers for Medicare and Medicaid Services and, because the hospital is an accountable care organization, the overall reimbursement to providers is reduced.
How would Joe's story end differently with Data 3.0? Three main technologies make up the new wave — the ABCs of artificial intelligence, blockchain and collaborative medicine.
Artificial Intelligence Since the 1950s, artificial intelligence, or AI, has facilitated interpretation of large data sets, which have revealed unique relationships among certain variables. Of course, artificial intelligence has seen a series of hype cycles followed by disappointment; however, with the advent of faster chips (thanks to the gaming industry), AI is beginning to show its worth. Think of artificial intelligence and its close cousin, natural language processing, as expert assistants perched on your shoulder, reading what you write in real time. AI reads Joe's chart in an instant — all of it. It checks for drug–drug interactions and can predict what will likely happen based on comparing Joe to millions of other Joes. AI sees that Joe not only has congestive heart failure, but also complex diabetes mellitus, and reminds the physician to document that this is a sick patient — the admission is entitled to higher reimbursement.
Importantly, artificial intelligence should be thought of as an assistant rather than as a replacement for people. When the reigning chess champion, Gary Kasparov, lost to IBM's Big Blue back in 1997, he created a new chess league that brought together three groups of competitors: humans, machines and humans with machine assistance. The third group leveraged the analytics of the machine with the creativity and intuition of the human. More recently, Cloudmedxhealth, the organization where Alan Pitt, one of the authors of this piece, works at as chief medical officer, used its AI to take a mock medical exam. Again, three groups were assessed: medical residents, software, and medical residents with software. Scores were roughly 70%, 80%, and 90%, respectively. After the exam, the residents reported that the software was increasingly useful as the exam wore on, and as they fatigued.
Blockchain The first blockchain was invented in 2008 as an attempt to democratize financial data. Popularly known as the basis for Bitcoin, blockchains provide distributed ledgers of transactions, removing the need for any single entity to act as a middleman for what's valid or not. Think of it this way: You give your money to the bank and although it provides a monthly statement based on your transactions, it essentially has complete control over your funds. If you make a payment, the bank validates you have the proper funds. If the bank suspects fraudulent activity, it will be quick to freeze your funds. Furthermore, while the bank holds your money it invests it, making some money in addition to whatever fees it charges you for the account. In a similar fashion, banks, hospitals and modern applications act as custodians of your data. You may generate your data and even have certain privileges to your data. Yet, most businesses have taken the approach that they own what they store. Any solution would require a cross-enterprise, trustable record of who owns what — where no single entity has the ability to abuse or misuse the data.
Blockchains provide the immutable, secure and distributed solution to this dilemma of siloed information. Given that no single entity owns the ledger, the overall administrative costs are markedly reduced and information exchange between entities is more fluid. Even further, rather than having individual governing entities owning and isolating data, data can achieve cross-border sovereignty by cross-enterprise shared truths of who is given permission to access what. When it comes to medicine, think of electronic medical records, personal health records, insurance contracting and electronic health care information exchange. These functions demand secure, transparent exchange of information. As the patient exits the halls of one hospital and enters the next, his data should not be stuck at the door. One example of blockchain in health care is Personal Digital Spaces, which provides application services for data rights. Cory Pitt, coauthor of this article, is a product manager for this platform. As data move from party to party over time, Personal Digital Spaces provide a ledger showing that relationship. Similar to a bank showing transactions, Personal Digital Spaces provides a ledger storing custodial history of that data. These rights can in turn offer solutions such as a personal health record, or other examples of the patient-centric aggregation of encounter data across federated databases, providing a single, patient-permissioned view of a patient's journey through care. These systems could involve a hierarchy of permission views, where a patient could indicate which data he or she wanted people to see.
Collaborative Medicine Previous articles in Health Progress have discussed telemedicine.4 In short, data without action doesn't change the course of care, and meaningful, effective action requires coordination between all parties involved in patient care. When it comes to telemedicine, there are ample opportunities for improving outcomes of chronically ill patients. Collaborative care includes remote patient monitoring — simple devices such as Fitbits and the Apple Watch — through more extensive technologies tied to a service. Collaborative care, which involves communication via text, voice or video, can also provide reassurance for patients, their family or less experienced providers.
Let's revisit Joe, our patient with congestive heart failure. This time, however, let's change his story by leveraging the ABCs of Data 3.0. After Joe suffers that first minor heart attack, his doctor uses AI and discusses expectations with him based on the course of millions of patients just like him. That means realistic predictions of what will happen if he adheres to his diet and takes his medications as prescribed — and what will happen if he doesn't.
Joe's doctor enters the information in her institution's records, but also has a copy sent to Joe's blockchain-based personal health record. Joe controls who can see his data via permissions distributed across enterprise boundaries. Joe's doctor recommends a Bluetooth scale for Joe, which reminds him to weigh himself every 24 hours. Similar to AllState's good driver discount, Joe's insurer gives him a discount if he checks his weight regularly. But Joe still likes his pizza, and he winds up back in the emergency department. This time, the emergency department doctor downloads Joe's personal health record and sees his medications and all of his activities over the past few weeks. The doctor dictates his notes with his natural language processing technology. The AI in the system sees Joe's history and warns the physician that Joe is at high risk for readmission, so the physician contacts the care coordinator, who sets up a personalized admission plan for Joe, including home visits and increased monitoring. The hospitalist's screen time is reduced because the AI makes sure his note accounts for all of Joe's associated comorbidities and even helps him code. No more late-night charting or nag notes from the revenue cycle team.
When Joe is back at home, he has brief daily telemedicine check-ins, which are much cheaper than home visits. Joe can call the nurse, but he can also use the internet to do personalized AI searches based on his medical records, his drugs and other issues he has concerns about. This last application is live on the Medicare website.5
Taking this a step further, the hospital system asks Joe whether he would be willing to share his Facebook data. Although the specifics of his profile will not be shared, Joe's care managers can use this data to help understand Joe's social determinants, to see when he might be getting depressed, or if things are changing in Joe's life or support network. This insight can help his care managers keep Joe on track and can help him live a longer, healthier life.
If you think this technology is far in the future, it's not. AI can take a lot of the guesswork out of health care, identifying individuals most at risk and predicting the future of patients with certain chronic conditions. So, now knowing how it could change your course as a patient, let's revisit the opening question. In this new world of artificial intelligence, blockchain and collaborative care, would you sacrifice some of your privacy to get a few more productive years of life?
What we can do and what we will do is up to us. It's really a matter of figuring out how to keep what makes us human in the context of the evolving technologies.
ALAN PITT is a professor of neuroradiology at the Barrow Neurological Institue Institute based in Phoenix, part of CommonSpirit Health. He is also the chief medical officer of Cloudmedxhealth, a health care artificial intelligence company that provides insights to the health care industry. CORY PITT is a product manager for Personal Digital Spaces, a provider of blockchain application services in health care and other sectors.
NOTES
- Atul Gawande, "Why Doctors Hate Their Computers," The New Yorker, Nov. 18, 2018, www.newyorker.com/magazine/2018/11/12/why-doctors-hate-their-computers.
- Gawande, "Why Doctors."
- Gawande, "Why Doctors."
- For more on telemedicine, see Alan Pitt, "Telemedicine: Health Care Unconfined by Walls," Health Progress 99, no. 5 (September-October 2018). Also Alan Pitt, "Why Your Doctor Seems To Be Ignoring You — They're Playing a Video Game," Healthcare Pittstop, https://healthcarepittstop.com/doctor-seems-ignoring-theyre-playing-video-game/.
- Medicare.gov: https://www.medicare.gov/manage-your-health/medicares-blue-button-blue-button-20/check-your-symptoms.