BY: ROBERT M. PESTRONK, M.P.H., JULIA JOH ELLIGERS, M.P.H. and BARBARA LAYMON, M.P.H.
The Commonwealth Center for Government Studies reports that the moment has come to take a fresh look at traditional practices and relationships and to develop new approaches that will serve our communities better and more efficiently.1 The center also recommends that hospital governance take oversight for both system-wide community benefit policies and programs and for the hospital's role and priorities in the realm of population health. Although many different solutions are now being proposed, most informed observers are unified on one point: The value and the quality of services should correspond to the size of the investment in the clinical care and public health sectors.2, 3
Local health departments, too, are being asked to re-examine and reprioritize their approaches to improving the public's health4 through proof of capacity,5 continuous improvement of the activities they perform6 and oversight for the outcomes achieved or desired by the public health and health care sector.7 The National Association of County and City Health Officials (NACCHO), representing the 2,800 local health departments across the country, sees this time as a true opportunity to improve the public's health.
As collaborative relationships between hospitals and local health departments become the new normal, opportunities abound. The new "community benefit" definition and requirements in the Affordable Care Act (ACA)8 require hospitals to conduct a community health assessment and produce a community improvement plan. Local health departments are required to produce an assessment and improvement plans. Why not plan and conduct these in a collaborative fashion, making use of the assets, capabilities and capacities which each can offer?
Assessment is a core function of public health. Many local health departments have traditionally conducted community health assessments9 — approximately 60 percent in the last five years.10 Many hospitals also have conducted or participated in community health needs assessments related to community benefit programs. Collaborative work will allow local health departments and hospitals around the country to build upon their existing expertise, relationships and experiences to conduct various improvement initiatives partnering together around specific goals.
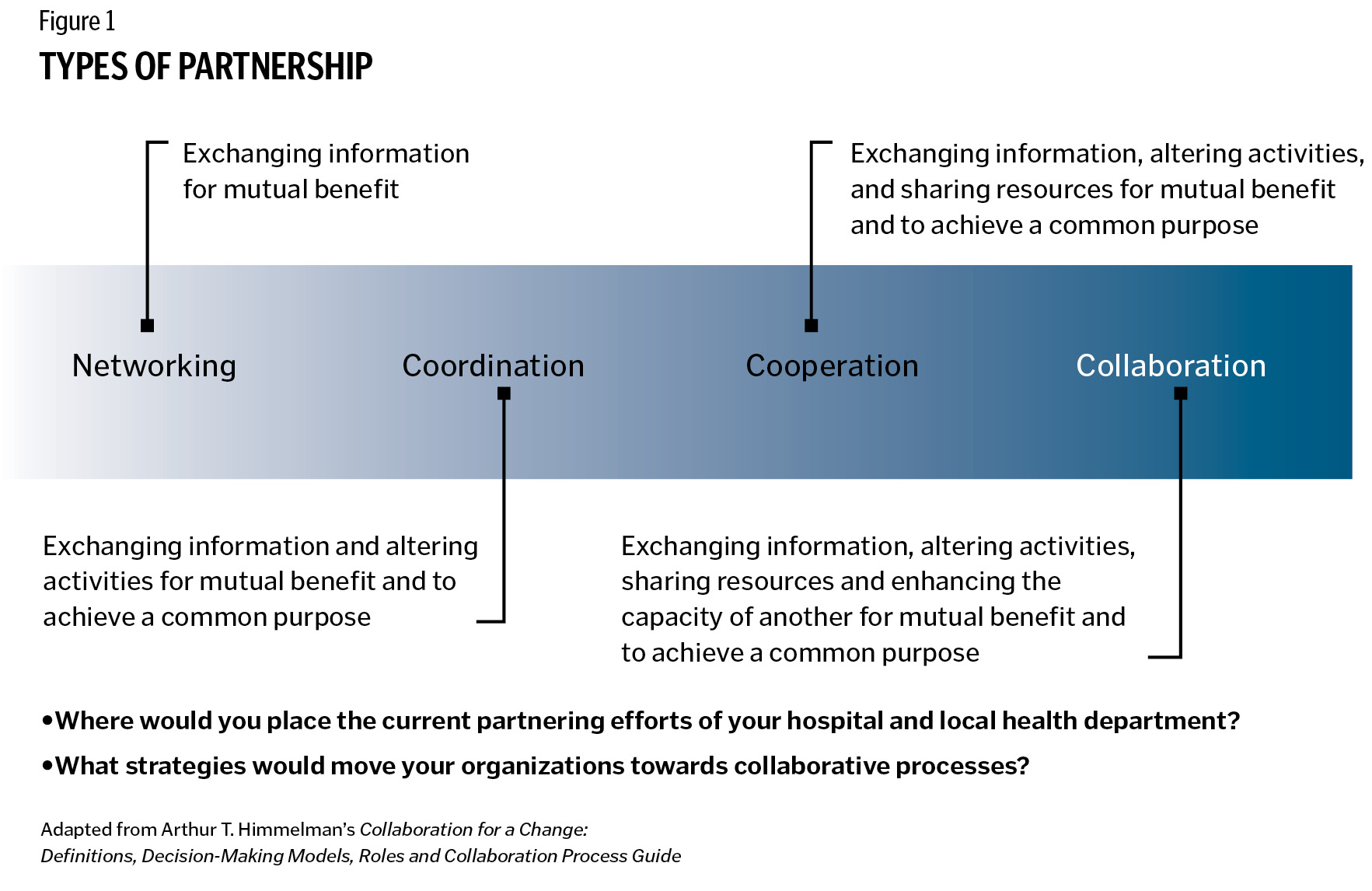
These efforts to partner around community health assessment and improvement planning span four types of strategies: networking, coordinating, cooperating and collaborating. With such collaboration, community health assessment and improvement activities can be precursors to real gains in population health and an integral part of continuous improvement processes towards that goal.
KEYS TO SUCCESSFUL COLLABORATION
Over the past year, NACCHO conducted three focus groups with leaders of health departments and nonprofit hospitals across the country to identify what makes community health assessment and improvement collaborations successful between local health departments and hospitals. Common strategies undergirded successful partnerships:
Formalized mechanisms. Communities where local health departments and hospitals work well together have constructed a formalized forum for dialogue. A memorandum of understanding helps clarify the roles and responsibilities of each entity. Further, a written memorandum of understanding helps ensure that collaborative efforts continue even if leadership at either organization changes. In communities where the local health department and hospital do not have a history of working together, a third party can help. In one Florida community, for example, the local health department and hospital used their health planning council to build and strengthen their relationship.
Vision. Successful collaboration is contingent on a shared vision or goal. One focus group participant said, "There's certainly a difference between what is the focus of public health versus individual care and private health care. But in focusing on some of the common goal areas ... that made a big difference."
Another participant pointed out it is important not only to think about what the product and process will look like, but ultimately to determine "what is the end game around the assessment?"
Communication. Frank, open and candid conversations between leaders and staff of local health departments and hospitals enrich relationships between collaboration partners. One local health department representative noted that department staff members learned about the financial and political realities that confront their nonprofit hospital, and their hospital partners learned about the political and financial challenges of governmental public health practice. Shared learning helped develop mutual respect. Together they were more effective in engaging other community organizations and partners.
Neutral convener. When there is more than one hospital in a community, a neutral convener can be helpful to the process of working together. Many local health departments have staff with facilitation skills that can be used to structure and coordinate collaborative assessment and improvement activities involving usually competitive area hospitals. One hospital executive said, "There are times when you have to put down the competition and raise a flag of collaboration, and that's what we've been able to do. I credit that to the health department for being able to put us all around the table and get some work done."
Champions and Leaders. Effective collaboration requires each organization to have champions who will move the effort forward. The champions can arise from formal leaders or other staff members; each background has advantages. A formal organizational leader can motivate and assign work to staff members, while a staff member's interest, energy and enthusiasm can infect leaders and other staff.
A successful collaboration needs support from local health officials and from hospital executives. Focus group participants noted that with leadership on board, their staffs, the community and partner organizations then seem to acknowledge the importance of assessment and improvement work. Several focus group participants commented that hospital executives, in particular, bring a level of prestige to assessment and improvement initiatives.
Attitude. Building trust and positive relationships takes time. A representative of a hospital nonprofit commented, "The hospitals that see the community health improvement process as an opportunity to improve community health, rather than an obligation, tend to be more successful." Challenges arise in any relationship. Focus groups revealed some of them. Competitive hospitals usually can work together on community health assessment processes, even if it's difficult for them to work together on other activities. One focus group member said that in her jurisdiction, competing hospitals pooled their resources to make sure the needs and requirements of the community health needs assessment process were met in a collaborative way. The group also included other health care providers (for example, a rehabilitation center) who helped bring in more data and ideas.
One participant observed that when hospitals are highly competitive, it's sometimes difficult to get them both on the same page, but once you get one hospital on board, other hospitals begin to show interest.
The timetable of the new Internal Revenue Service requirement for hospitals does not necessarily coincide with the timing of health department reporting and planning requirements; however, hospitals and health departments can work together to design a process and data management system that produces results they each can use.
Health department jurisdictions may encompass several hospitals. Hospital market areas may span many local health department jurisdictions. Flexible designs and processes among multiple hospitals and local health departments can overcome jurisdictional boundary issues.
TOWARDS HEALTHIER COMMUNITIES
There are many ways that local health departments and hospitals can pool their resources of time, talents, data, knowledge, partner base and funding to support collaborative efforts to achieve healthier communities. Local health departments and hospitals bring complementary strengths in many areas, including:
Data: While local health departments have vital statistics and county mortality and morbidity data on their jurisdictional population, hospitals have data on their patient population. Some local health departments have data specific to census tracks or neighborhoods, data on social determinants of health and data on behavioral risk factors. Further, many health departments have data on the communities' perceptions of quality of life. Some local health departments have conducted forces of change assessments that identify externalities that can have an impact on health, while others have conducted public health system assessments that measure how well local organizations work together to provide essential services. Many local health departments also have collected qualitative data on assets that can be leveraged to solve health problems. When viewed together, data from local health departments and from hospitals provides a more complete picture of a community's health challenges. That picture creates a shared understanding that can inform potential solutions.
Skills and Processes: Many local health departments have skills specific to community health assessment and improvement. Local health departments already have well-established processes for completing community health assessment and improvement processes. In focus groups, several local health department representatives commented that their hospital partners were happy to hear the local health department had a structured process like Mobilizing for Action through Planning and Partnerships (MAPP)11 that would help them meet their assessment requirements.
Local health departments also may have assessment-related experience in data collection, data analysis, community outreach, facilitation, health education and wellness programs. One advantage of the local health department as facilitator is its ability to find and maintain multiple contacts — many champions — within partner organizations in order to manage details which come up in collaborative efforts. Similarly, hospitals may have processes in place to conduct community health improvement work such as patient education, wellness programs, outreach and other activities that can be natural adjuncts to local health department activity.
Partners: Many local health departments have access to a variety of nontraditional and community partners, working directly with community residents and grassroots organizations. Some have staff members with skills in qualitative methods, such as key-informant interviews and focus groups, whose work provides rich context and explanatory power to quantitative data. Hospitals have partners and board members who bring a certain stature to the work of engaging a community, adding legitimacy and the chance of acceptance for initiatives that may bring far-reaching health changes. A health department executive added that it's important to have the right people in the room who are aware of all the resources available from their organizations.
Health Equity: In the community health dialogue, local health departments bring a public health view regarding the central importance of assuring the conditions where people can be healthy. Hospitals bring experience in the care and treatment of members of marginalized populations, and they bring a needed perspective to the health equity conversation.
Through collaborative community health assessment, local health departments and hospitals have been able to implement well-informed organizational strategic plans and collaborative, overarching community-health improvement plans. Collaborative community health assessments have allowed organizations to identify the needs of specific subpopulations and develop solutions to their unique needs. What's more, other organizations then can align and integrate portions of their strategic plans with a community health improvement plan. Further, collaboration among local health departments, hospitals and other entities have resulted in comprehensive assessments that inform grant proposals, public policy and ways for organizations to work more efficiently and effectively together.
Partnerships between hospitals and local health departments have proven productive in many communities. Better organized systems of care can assure that both treatment and prevention are artful and evidence-based. Designed attention to the unique goals, roles and needs of hospitals and local health departments will benefit from the strengths and assets each partner offers. Communication and dialogue among hospitals, health departments and other local partners can lead to concurrence and a prioritization based on the community's risks to health and remedies to prevent disease. Other benefits include a shared understanding of problems, transparency about efforts to improve health and treat illness and better public support for each partner and the partnership.
Collaborative community health assessment and community health improvement processes should be standard practice everywhere. Effective collaboration will require intent and patience as very different cultures come to know each other better. Leadership in both organizations must encourage the awkward steps that will no doubt precede the more elegant and practiced choreography of effective collaborations.
What will be discovered on the journey is a better command of the role that each entity can play in a re-forming medical and public health system and, more important, better success with their shared mission of population health.
ROBERT M. PESTRONK is executive director for the National Association of County and City Health Officials (NACCHO) in Washington, D.C.
JULIA JOH ELLIGERS is NACCHO's director, assessment, planning and workforce development, Washington, D.C.
BARBARA LAYMON is lead program analyst for assessment and planning within NACCHO's public health infrastructure and systems team, Washington, D.C.
NOTES
- Lawrence Prybil et al., Governance in Large Nonprofit Health Systems: Current Profile and Emerging Patterns (Lexington, Ky.: Commonwealth Center for Governance Studies, 2012). www.hallrender.com/health_care_law/library/articles/1220/Governance_booklet.pdf.
- Joseph R. Antos, Mark V. Pauly and Gail Wilensky, "Bending the Cost Curve through Market-Based Incentives," New England Journal of Medicine 367 (Sept. 6, 2012), www.nejm.org/doi/full/10.1056/NEJMsb1207996 (accessed 8/3/12).
- Ezekiel Emanuel et al., "A Systemic Approach to Containing Health Care Spending," New England Journal of Medicine 367 (Sept. 6, 2012), www.nejm.org/doi/full/10.1056/NEJMsb1205901 (accessed 8/3/12).
- Institute of Medicine, For the Public's Health: The Role of Measurement in Action and Accountability (Washington, D.C.: National Academy of Sciences, 2010). See more at www.iom.edu/Reports/2010/For-the-Publics-Health-The-Role-of-Measurement-in-Action-and-Accountability.aspx.
- See Public Health Accreditation Board, www.phaboard.org/accreditation-overview/what-is-accreditation/.
- National Association of County and City Health Officials, Operational Definition of Public Health (Washington, D.C.: NACCHO, 2005), www.naccho.org/topics/infrastructure/accreditation/upload/OperationalDefinitionBrochure-2.pdf.
- IOM, For the Public's Health.
- The Affordable Care Act requires nonprofit hospitals to conduct community health needs assessments. The public health field does not limit community health assessments to identifying needs and therefore are using the term community health assessment, excluding the explicit reference to needs. Community health assessments that are limited to uncovering needs do not comprehensively identify community issues and solutions to addressing problems. Often public health community health assessments include information about community assets and other information about forces, quality of life and how different providers work together to deliver services, which provides a comprehensive illustration on why needs and public health problems exist in a community.
- The National Association of County and City Health Officials, Issue Brief: Collaborating through Community Health Assessment to Improve the Public's Health. December 2011. Downloaded at www.naccho.org/topics/infrastructure/mapp/loader.cfm?csModule=security/getfile&pageID=228716.
- National Association of County and City Health Officials, 2010 National Profile of Local Health Departments (Washington, D.C.: NACCHO, 2011), www.naccho.org/topics/infrastructure/profile/resources/2010report/upload/2010_Profile_main_report-web.pdf.
- For more information about the MAPP (Mobilizing for Action through Planning and Partnerships) process, visit www.naccho.org/mapp.
