Gina Fullam
Saint Louis University
Albert Gnaegi Center for Health Care Ethics
[email protected]
Editor's Note: Graduate students in health care ethics were invited to make submissions in a student essay contest. This essay is one of the entries. Several others will be published in subsequent issues of HCEUSA.
Introduction
Though in vitro fertilization (IVF) has become common treatment for unexplained subfertility,1 concerns about the practice linger. The risks to women posed by all-too-common IVF-associated multiple pregnancies, and the heightened risks of prematurity and congenital disabilities for IVF-conceived babies, are troublesome to those of all moral sensibilities. Furthermore, spare embryos and the practice of fetal reduction are disconcerting to those even outside of anti-abortion circles. Finally, the costs of IVF treatment raise serious questions of justice and access. Surprisingly, a Cochrane review finds that the assumed efficacy of IVF for unexplained subfertility relative to other more natural treatments is not sustained by empirical evidence. Given these ethical concerns, and the unproven relative efficacy of IVF, I argue that standard care for unexplained subfertility should favor more natural options, including expectant management. I also consider the promising preliminary evidence for Natural Procreative Technology (NaProTechnology), an infertility treatment approach that seeks to identify and address the underlying cause of a couple's infertility. Though I acknowledge the need for further empirical studies on NaProTechnology's effectiveness, I argue that couples seeking treatment for unexplained subfertility should at least be informed of NaProTechnology's methods. Moreover, Catholic health care can and should take a lead role informing patients of and treating patients using NaProTechnology's methods.
Standard Infertility Treatment
Infertility, the inability to become pregnant after one year (or six months if a woman is 35 years or older) of normal sexual intercourse without contraception, affects an estimated 10 percent of couples of childbearing age in the United States.2 Infertility can be devastating for a couple who wishes to have children of their own. Many couples feel that their marriage is unfulfilled if they do not have children, and involuntary childlessness may lead to "low levels of self-esteem and to feelings of anger, denial, depression and frustration."3 Today, however, infertility need not mean a couple will never give birth to a child of their own. Mainstream medical practice has developed infertility treatments which enable the desires of some of these couples to become reality.
Generally when a couple is having difficulty conceiving, a family physician or gynecologist will encourage the couple to continue to engage in regular sexual intercourse for a few months.4 If the couple has not achieved pregnancy after that time, the doctor may suggest timed sexual intercourse and show the woman how to chart her body temperature (in order to more accurately know when she is fertile) and also perhaps start the woman on fertility drugs, such as clomiphene citrate, to regulate her cycle. If these attempts are also unsuccessful, the couple is recommended to a fertility specialist or clinic. Here both the man and woman are physically examined and their complete medical and social histories are taken. In further effort to identify the cause of infertility, blood tests, urinalysis, sperm analysis and postcoital tests are performed, and the woman will undergo a hysterosalpingography (X-ray of uterus and fallopian tubes).
At this point, some relatively simple procedures, such as artificial insemination in the case of male infertility due to poor sperm motility or low sperm count, may be attempted. In artificial insemination, a sample of the man's or donor's sperm is obtained, usually through masturbation, the sperm is "washed" so as to optimize chances of fertilization, and the washed sperm is injected into the woman's vagina or uterus during the woman's fertile period. Artificial insemination gained popularity in the United States in the 1960s.
If these efforts are still unsuccessful, more advanced assisted reproductive methods, in which both sperm and egg are handled, may be attempted.5 These assisted reproductive methods are known as artificial reproductive technologies (ARTs), and may make use of donor gametes and surrogate mothers. Sperm is retrieved and prepared in the same way as it is in artificial insemination. The egg retrieval process is lengthier and more invasive. Though even more invasive at one time, today a woman will take ovarian stimulation drugs (which must be injected) for three to four weeks, and then one or more of her eggs are retrieved through transvaginal ultrasound guided egg aspiration.
ARTs include, but are not limited to:
(1) In vitro fertilization (IVF) and embryo transfer: Developed to remedy blocked or damaged fallopian tubes and first successful in 1978, today IVF is the most well-known and commonly practiced ART. IVF involves the mixing of sperm and egg in a petri dish and the placement of one or more resultant embryos into the uterus 2-5 days after fertilization.
Embryos not selected for placement into the uterus are discarded or frozen for later usage. When more embryos implant than would be healthy for the woman to carry to term, fetal reduction is recommended.
(2) IVF with intracytoplasmic sperm injection (ICSI): A specific form of IVF developed to circumvent sperm-related infertility, ICSI involves the injection of a single sperm directly into an egg (in vitro), and the placement of the resultant embryo into the uterus.
(3) Zygote intrafallopian transfer (ZIFT): A process similar to IVF, though only performed when infertility is not caused by tubal blockage, ZIFT involves the transfer of one or more zygotes (fertilized in vitro) to one of a woman's fallopian tubes immediately after fertilization with the hope that the zygote will then arrive and implant into the uterus naturally.
(4) Gamete intrafallopian transfer (GIFT): In this process, sperm and egg are mixed in vitro but transferred to one of a woman's fallopian tubes before fertilization has occurred.
All of these procedures can be assisted by preimplantation genetic diagnosis (PGD) and prenatal genetic diagnosis, which test embryos for genetic disease prior to and after implantation, respectively.
The Centers for Disease Control and Prevention (CDC) estimates that slightly more than 1 percent of total U.S. births are the result of ART.6 The number of ART cycles performed in the United States nearly doubled from 19997 to 20108 (87,636 cycles in 1999 compared with 147,260 cycles in 2008).9 In 1999, 30,629 infants were born as a result of these ART cycles. The number of live births has also steadily increased, with 61,564 ART-conceived children born in 2010. Specific to this paper, couples with unexplained infertility are represented in 9.5 percent,10 or about 14,000, of these cycles, and about 4,700 live births. IVF and IVF with ICSI accounted for 99.9 percent of all ART cycles in 2010; hence the focus of this paper on IVF is warranted.
IVF: Risks to Women and Children
IVF and other related procedures are not without risk to either women participating in fertility treatment or the children to be created through these technologies. In 2010, for ART cycles using fresh nondonor eggs or embryos, the incidence of twins was 28.8 percent and the incidence of triplets or more was 1.5 percent.11 For ART cycles using frozen nondonor embryos, the incidences of twins and triplets were 22.8 percent and 1.1 percent respectively. For ART cycles using fresh embryos from donor eggs, the incidences of twins and triplets were 36.7 percent and 0.8 percent respectively. These numbers compare to a 1.05 to 1.35 percent rate of twins and 0.01 to 0.017 percent rate of triplets in the general population.12 Maternal mortality is seven times greater in multiple pregnancies than in single pregnancies13 due to "increased incidence of preeclampsia, placenta previa, placental abruption, premature rupture of the membranes, postpartum hemorrhage, and Cesarean section."14 Perinatal mortality rates quadruple for twins, and sextuple for triplets.15 Furthermore, twins are 9.6 times more likely than singletons to be very low birth weight, and thus susceptible to a multitude of problems, and triplets or more are 32.7 times more likely than singletons to be very low birth weight.16
Even singleton IVF babies, however, are at increased risk for preterm delivery, low and very low birth weight, Caesarean section, admission to neonatal intensive care unit, and perinatal mortality.17 ART-conceived children, including singletons, are two to four times more likely to have heart problems, cleft lip, cleft palate and abnormalities in the esophagus or rectum.18 Other studies indicate a link between ARTs and developmental delay, cerebral palsy, and autism spectrum disorders.19 It is important to note that the long-term effects of IVF are unknown, as the first IVF conceived baby is now only 34 years old.
Fetal Reduction and Spare Embryos
In an effort to reduce the risks to women and children, fetal reduction is often performed in the event that a multiple gestation pregnancy results from IVF. The practice of fetal reduction involves selecting the fetus or fetuses to be eliminated either by chromosomal abnormalities, ease of reach, or sex, and injecting a shot of potassium chloride into the heart of each selected fetus. The fetuses are left to be absorbed by the woman's body. The CDC does not report the frequency of fetal reduction in ART treatment.20 "This is a very sensitive topic,"21 explains David Grainger, now past president of the Society for Assisted Reproductive Technologies (SART). Nevertheless, investigative journalist Liza Mundy finds that the practice, though often unmentioned, is common.22
Although the practice of fetal reduction associated with IVF has not received the same backlash from the anti-abortion movement as abortion — perhaps because fetal reduction is not as much in the public eye — even women who undergo fetal reduction do not do so without concerns. The procedure itself carries a 16 percent or greater risk that the remaining fetuses will be preterm, and the same degree of risk that the entire pregnancy will be lost before 24 weeks of gestation.23 It is also not irrelevant that the most recent Gallup poll reports that 50 percent of Americans consider themselves pro-life, compared to 41 percent identifying as pro-choice.24
The spare embryo issue related to IVF is also a bit of an anomaly in the typical divide between pro-life and pro-choice. It is not uncommon for ten embryos to result per IVF cycle; only one to three of which are typically implanted into the woman's uterus. The remaining embryos are then frozen and stored. The question, with which many couples and individuals with frozen embryos struggle, is what to do with these embryos. Their choices are: use for further reproduction, discard the embryos, donate the embryos for reproduction, and donate the embryos to science. Interestingly, one study found that 72 percent of couples, even after an average 4.2 years of storage, are unsure of what to do.25 Their embryos remain frozen indefinitely, contributing to the estimated one half million frozen embryos in storage in the United States.26 Couples cite discomfort with having another couple gestate and raise their children and the idea of their embryos as "virtual" children among their reasons for indefinite freezing.27
Costs of IVF
The high costs of IVF treatment also raise noteworthy ethical questions. Per cycle estimates in the United States usually range between $7,000 and $11,000. The bulk of this cost is out of pocket, as many insurance companies do not provide IVF coverage. This cost in itself is prohibitive to many infertile couples. Interestingly, only 38.5 percent of infertile couples have ever used infertility services,28 and not using infertility services is correlated with lower income and lower education levels.29 Mundy argues that those lower income couples (already disproportionately infertile due to lack of prior access to treatment for initially preventable infertility causes) who do seek infertility treatment are endangered by non-access to IVF and/or follow-up care.30 When the only treatments lower income couples can afford are fertility drugs, which will be taken without monitoring or follow-up appointments, their risks for multiple pregnancies and ensuing complications are exceedingly high.
Even couples who can afford the base price tag associated with IVF, however, may not be able to afford IVF's associated costs. As Robert Blank correctly notes, an accurate figure must take into account the number of failed cycles often undergone before a live birth is achieved, as well as the "costs of all subsequent procedures that occur more often with IVF pregnancies, such as high-risk obstetrical care, Cesarean sections, and neonatal care."31 A 1994 estimated cost per live birth including such indirect costs was $66,667 for successful birth after one IVF cycle, and $114,286 for successful birth after six cycles.32
Efficacy of IVF for Unexplained Subfertility
In the face of these concerns about risks to women and children, fetal reduction, spare embryos, and costs, it is worth asking if there are not other equally effective methods of treating infertility and, specifically, unexplained subfertility, which is the focus of this paper. Given that IVF and fetal reduction are gravely contrary to the moral law,33 it is especially important for Catholic health care to ask if there are not other equally effective methods of treating infertility. Surprisingly, a systematic Cochrane review has found that although IVF is a widely accepted treatment option for couples with unexplained subfertility, "its effectiveness has not been rigorously evaluated in comparison with other treatments."34 The Cochrane review assessed all randomized control studies that compared the effectiveness of IVF in achieving live birth to the effectiveness of one or more of the following: expectant management, clomiphene citrate, intrauterine insemination, intrauterine insemination with controlled ovarian stimulation, and GIFT. Randomized clinical trials are the "gold standard for experimental evaluation of medical or surgical infertility therapy."35
In comparison with expectant management, the Cochrane review found that IVF attained significantly higher clinical pregnancy rates (odds ratio 3.24; 95 percent confidence interval 1.07 to 9.8).36 However, the review does not allow conclusions to be drawn from this data given the studies' small sample sizes (35 and 51 participants) and inadequate follow-up with participants. The duration of follow-up was three months in the first study and six months in the second. The systematic review found no studies comparing IVF with clomiphene citrate.37 Studies comparing IVF with intrauterine insemination either without or with ovarian stimulation did not exhibit any difference in live birth rates (odds ratio 1.96; 95 percent confidence interval 0.88 to 4.4 and odds ratio 1.15; 95 percent confidence interval 0.55 to 2.4, respectively).38 Though periodically updated, the Cochrane review's conclusions have remained unchanged since 2005.
A 2008 randomized study39 compared the effectiveness of expectant management, clomifene citrate, and unstimulated intrauterine insemination as treatment for unexplained subfertility. This study was not included in the Cochrane view as it did not examine the effectiveness of IVF relative to these treatments. However, I include the study here given the lack of data comparing IVF with clomiphene citrate noted in the Cochrane view. S. Bhattacharya et al. randomly assigned each of 580 couples with infertility for over two years to one of three study arms. Those assigned to the expectant management arm did not receive any follow-up treatment or advice. Differences in live birth rates after six months (17 percent for expectant management, 14 percent for clomiphene citrate, and 23 percent for unstimulated intrauterine insemination) across the three arms were not statistically significant.
Allowing the Bhattacharya study to inform the Cochrane review suggests an important point. Given that the Cochrane review finds no statistical difference in live birth rates between IVF and either unstimulated or stimulated intrauterine insemination, and given that the Bhattacharya study finds no statistical difference in live birth rates among expectant management, clomifene citrate, and unstimulated intrauterine insemination, it may follow that there is no statistical difference between IVF and expectant management, clomifene citrate, or unstimulated intrauterine insemination.
Challenges of Research
In fairness, I note that there are unique challenges to research examining the efficacy of infertility treatments, and treatment for unexplained subfertility in particular, especially to meet the high standards of Cochrane reviews. If anything, however, these challenges give IVF an advantage over more natural treatment options in research studies.
D. Guzick and J. Queenanjr observe, for instance, that there is always a probability that a couple will achieve pregnancy during treatment that is not a result of the treatment under study.40 Studies suggest spontaneous pregnancy rates as high as 60 percent.41 Additionally, large sample sizes are necessary to overcome differences in IVF success rates among fertility clinics.42 As such, randomized clinical trials require the cooperation of multiple fertility clinics. Thirdly, patients and physicians participating in studies may have preconceived notions of what constitutes "best" treatment.
This last challenge is evident in the Bhattacharya study. Bhattacharya et al. found that 94 percent of women randomized to clomifene citrate and 96 percent of women randomized to unstimulated intrauterine insemination found the process of treatment acceptable, compared with 80 percent of women randomized to expectant management. Although differences in satisfaction rates did not correspond to any difference in anxiety and depression scores (these scores were even across the three groups), Bhattacharya et al. conclude that "women with infertility are reassured by active treatment and are less satisfied with an expectant approach."43
NaProTechnology: Unexplained Infertility
Having now observed the ethical concerns surrounding IVF, as well as the dearth of evidence demonstrating the efficacy of IVF relative to other treatments in achieving live births for couples with unexplained subfertility, I argue that standard care for unexplained subfertility should favor more natural options, including expectant management. Above all, standard care for unexplained subfertility in Catholic health care should favor natural options. Specifically, I recommend that the second step of standard infertility treatment, the period of time which involves testing and simple fertility treatments, be significantly expanded. At the same time, I urge further research into best treatment for unexplained subfertility, which again can and should be spearheaded by Catholic health care.
Pope John Paul II's Donum Vitae in 1987 and the Congregation for the Doctrine of Faith's Dignitas Personae in 2008 expound that sexual intercourse is not to be stripped of its unitive dimension via assisted reproductive methods which replace or substitute for the conjugal act.44 The marriage bond, the dignity of the child, the right of the child to be conceived, carried in the womb, brought into the world and brought up within marriage, and the respect due to the child's origin all add additional weight to this teaching. Thus the Catholic Church rejects many mainstream infertility treatments, including AI, IVF, IVF with ICSI and ZIFT. The Church also condemns the destruction of spare embryos and practice of selective fetal reduction associated with IVF and related ARTs. Catholic health care, then, has a special obligation to inform patients of and offer natural options for treatment of unexplained subfertility, and a special obligation to invest in research into natural treatment for unexplained subfertility.
Both inside and outside of Catholic health care, it should be obvious that best treatment for unexplained subfertility would include diagnosis of the cause of subfertility. In fact, rarely does the medical professional encourage a band-aid treatment approach. Knee-replacement surgery, for instance, is not medically indicated when the functionality of the knee can be restored. Still, literature reports that fertility specialists diagnose between 25-30 percent of all infertility as "unexplained."45 N. Gleicher and D. Barad point out that the diagnosis of unexplained infertility is in fact a misnomer, as unexplained infertility only indicates that more diagnostic testing remains to be performed.46 They urge: "A better effort should be undertaken to develop reliable tools to diagnose, hitherto often undiagnosed, conditions of endometriosis, tubal disease, premature ovarian ageing and immunological infertility, which are often misdiagnosed for UI [unexplained infertility]."47
Unbeknownst to Gleicher and Barad, and in fact little known to the fertility field, Thomas W. Hilgers, MD and colleagues at Creighton University and Saint Louis University Schools of Medicine over the last thirty years have worked to develop Natural Procreative Technology (NaProTechnology), an approach to infertility that seeks to identify and address the underlying cause of a couple's infertility.48 Though only a handful of studies demonstrating the effectiveness of NaProTechnology have been published, and at that, only one in a peer-reviewed journal, the success of NaProTechnology in diagnosing the underlying cause of a couple's infertility is promising.
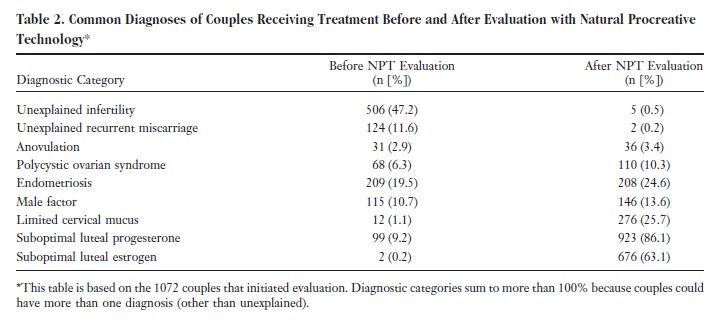
In the Journal of the American Board of Family Medicine September-October 2008 issue, Drs. Joseph B. Stanford, Tracey A. Parnell, and Phil C. Boyle presented their study of 1,072 couples who received NaProTechnology treatment between February 1998 and January 2002 at a clinic in Galway, Ireland.49 Table 250 shows the diagnoses of couples after complete evaluation using the Creighton Model FertilityCare™ System's charting method for ovulation in conjunction with timed blood samples and reproductive hormone testing. As indicated in Table 2, while 506 (47.2 percent) of couples' infertility was unexplained prior to evaluation, only 5 couples' (0.5 percent) infertility remained unexplained after evaluation. Boyle notes in a separate article that, "The timed hormonal blood tests for both progesterone and estradiol help us to identify subtle deficiencies that are simply not diagnosed with a day 21 blood test [standard practice] that does not pay any attention to the time of ovulation."51 The Ireland study indeed offers preliminary evidence that the more reliable methods to diagnose unexplained infertility that Gleicher and Barad urge can be, and in fact have been, developed.
Efficacy of NaProTechnology in Achieving Live Births
Promisingly, the Ireland study suggests that NaProTechnology is not only successful in the identification of the underlying cause of a couple's infertility, but also has live birth rates comparable to those of IVF. NaProTechnology's methods include surgical means to restore fertility;52 however the Ireland study only evaluated NaProTechnology's medical protocols (as surgical means were unavailable at the clinic at the time). Richard Fehring provides insight into these medical protocols:
Treatment involved having the woman patient track her fertility with the CrM system [Creighton Model FertilityCare™ System] (which focuses primarily on the estrogenic changes in cervical mucus), assessing the timing of intercourse, evaluating the quality of cervical mucus production, measuring luteal phase lengths, and determining levels of progesterone and estrogen on certain days of the menstrual cycle. When menstrual cycle deficits were detected, treatment included the use of clomiphene (to stimulate ovulation), medications to stimulate cervical mucus production, and progesterone supplementation.53
The average female age of the study was 35.8 years.54 Thirty-three percent of the couples had previously attempted ART treatment. Excluded from the study were couples whose infertility was the result of menopause or azoospermia, which NaProTechnology cannot treat. This is, of course, irrelevant to the present consideration of best treatment for unexplained subfertility.
For those couples that could be treated using NaProTechnology, the Ireland study two-year crude proportion live birth rate was 25.5 percent, and the adjusted proportion live birth rate (adjusted for couples who dropped out of the study as well as couples who were continuing treatment after the two year trial period) was 52.8 percent.55 This success rate is indeed comparable to the estimated 13-28 percent live births resulting per cycle from IVF.56 Especially interesting is that 16 percent of those couples who had previously attempted ART treatment were able to achieve pregnancy and carry the child to term using NaProTechnology.57
Though there are no studies comparing couples' satisfaction rates for NaProTechnology to satisfaction rates for expectant management, the couple's participation in and understanding of the treatment, which is essential to NaProTechnology,58 may very well help to overcome the research challenge of active versus non-active treatment. I also note that the Ireland study suggests NaProTechnology as a viable alternative to IVF for conditions other than unexplained subfertility.
It is obvious that one peer-reviewed study on NaProTechnology's effectiveness does not meet the standards of evidence-based medicine. Indeed, the Ireland report concludes that, "Large multicenter prospective studies are warranted to confirm these results, to explore further the characteristics associated with successful NPT [NaProTechnology] treatment, and to directly compare NPT to other forms of infertility treatment."59 Nevertheless, the preliminary evidence of NaProTechnology's effectiveness in both identifying the cause of a couple's infertility and achieving live birth rates is promising. If no evidence demonstrates IVF's effectiveness over more natural methods such as expectant management for treatment of couples with unexplained subfertility, there is no reason why couples seeking treatment for unexplained subfertility should not also be informed of NaProTechnology during step two of their treatment.
Standards for innovative treatment in the field of reproduction are all but non-existent. As a result of a long-standing government ban on federal funding for research involving human embryos, the fertility field has developed virtually independent of Food and Drug Administration (FDA) or Institutional Review Board (IRB) oversight. Regardless, NaProTechnology possesses no risk of harm that would raise issues even by the standards for innovative treatment in other fields. In fact, the multiple birth rate in the Ireland study was only 4.5 percent, compared with the 23-37 percent60 multiple birth rate associated with ART. Thus, in NaProTechnology, Hilgers and colleagues have developed an approach to fertility that is both in conformity with Church teaching and, at least preliminarily, scientifically sound.
Moreover, unlike IVF, NaProTechnology is often covered by insurance. Over 200 FertilityCare™ Centers featuring NaProTechnology exist throughout the United States and Canada, and additional centers have opened in Ireland, Poland, Taiwan, and Australia.61 NaProTechnology's methods are also easily accessible (for instance, to interested fertility specialists) in the 1244 page volume The Medical & Surgical Practice of NaProTechnology by Thomas W. Hilgers.62
Conclusion
Given IVF's costs, risks to women and children, and the associated issues of fetal reduction and spare embryos, and the lack of empirical evidence showing IVF's effectiveness over other treatments for unexplained subfertility, I agree that standard treatment for unexplained subfertility should favor more natural options, including expectant management. This argument has special urgency in Catholic health care, where treatment such as IVF is morally impermissible. I further submit that couples seeking treatment for unexplained subfertility should at least be informed of NaProTechnology's methods, and again, Catholic health care can and should take the lead in this.
1. I will use "infertility" and "subfertility" interchangeably. Though some distinguish between "infertility" and "subfertility," the distinction is not relevant to the discussion in this paper.
2. I will focus this paper primarily on treatment for unexplained subfertility in the United States. See Centers for Disease Control and Prevention, "Infertility," http://www.cdc.gov/reproductivehealth/Infertility/index.htm#1.
3. The New York State Task Force on Life and the Law, Surrogate parenting: analysis and recommendations for public policy (1988). 12.
4. Victor Groza and Karen F. Rosenberg, Clinical and practice issues in adoption (Westport, CT: Greenwood Publishing Group, Inc., 1998). 25.
5. Ibid.
6. Centers for Disease Control and Prevention, "2010 assisted reproductive technology: national summary report," (2012).
7. 1999 is the first year for which the CDC collected data.
8. 2010 is the most recent year for which data is available.
9. As the CDC only compiles statistics from reporting fertility clinics, and fertility clinics are not required to report, the true figures are likely higher.
10. The CDC reports 13.9 percent of cycles for couples with unexplained infertility making use of fresh nondonor eggs or embryos; cycles making use of fresh nondonor eggs or embryos represent 68.5 percent of all ART cycles. Couples' diagnoses are only reported for those cycles making use of fresh nondonor eggs or embryos, so the actual numbers may be higher.
11. These numbers reflect live birth rates and do not include multiple pregnancies that miscarried or were reduced by fetal reduction. See Centers for Disease Control and Prevention, "2010 assisted reproductive technology: national summary report."
12. MA Seoud et al., "Outcome of twin, triplet, and quadruplet in vitro fertilization pregnancies: the norfolk experience," Fertility and Sterility 57, no. 4 (1992).
13. R.C Wimalasundera, G Trew, and N.M Fisk, "Reducing the incidence of twins and triplets," Obstetrics & Gynecology 17, no. 2 (2003).
14. Robert H. Blank, "Assisted reproduction and reproductive rights: the case of in vitro fertilization," Politics and the Life Sciences 16, no. 2 (1997).
1. Wimalasundera, Trew, and Fisk, "Reducing the incidence of twins and triplets."
15. B. Luke, "The changing patterns of multiple births in the united states: maternal and infant characteristics, 1973 and 1990," Obstetrics & Gynecology 84, no. 1 (1994).
16. F. M. Helmerhorst et al., "Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies," British Medical Journal 328, no. 7434 (2004); R. A. Jackson et al., "Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis," Obstetrics and Gynecology 103, no. 3 (2004).
17. J. Reefhuis et al., "Assisted reproductive technology and major structural birth defects in the united states," Human Reproduction 24, no. 2 (2009).
18. Dorte Hvidtjørn et al., "Cerebral palsy, autism spectrum disorders, and developmental delay in children born after assisted conception: a systematic review and meta-analysis," Archives of Pediatric & Adolescent Medicine 163, no. 1 (2009).
20. Centers for Disease Control and Prevention, "2010 assisted reproductive technology: national summary report."
21. David Grainger as quoted by Liza Mundy, Everything conceivable: how assisted reproduction is changing men, women, and the world (New York: Alfred A. Knopf, 2007). 254.
22. Ibid.
23. Luke, "The changing patterns of multiple births in the united states: maternal and infant characteristics, 1973 and 1990."
24. Gallup, ""Pro-choice" americans at record-low 41 percent," (May 2012).
25. R. D. Nachtigall et al., "Parents' conceptualization of their frozen embryos complicates the disposition decision," Fertility and Sterility 84, no. 2 (2005).
26. This is a 2007 estimate; numbers are likely higher now. See DI Hoffman et al., "Cryopreserved embryos in the United States and their availability for research," Fertility and Sterility 79, no. 5 (2003).
27. Nachtigall et al., "Parents' conceptualization of their frozen embryos complicates the disposition decision."
28. Infertility services are defined in the study as including any consultation or treatment for infertility.
29. A. Chandra and E. H. Stephen, "Infertility service use among U.S. women: 1995 and 2002," Fertility and Sterility 93, no. 3 (2010).
30. Mundy, Everything conceivable: how assisted reproduction is changing men, women, and the world: 222.
31. Blank, "Assisted reproduction and reproductive rights: the case of in vitro fertilization."
32. PJ Neumann, SD Gharib, and MC Weinstein, "The cost of a successful delivery with in vitro fertilization," New England Journal of Medicine 331, no. 4 (1994).
33. Catechism of the Catholic Church, (New York: Doubleday, 1995). §2376 and 2270-2275.
34. Zabeena Pandian, Ahmed Fathy Gibreel, and Siladitya Bhattacharya, "In vitro fertilisation for unexplained subfertility," Cochrane Database of Systematic Reviews, no. 2 (2005).
35. D. Guzick and J. Queenanjr, "Evaluating the efficacy of intervention," Endocrinology & Metabolism Clinics of North America 32, no. 3 (2003).
36. Pandian, Gibreel, and Bhattacharya, "In vitro fertilisation for unexplained subfertility."
37. Another Cochrane review finds that there is, in fact, "no evidence of clinical benefit of clomiphene citrate for unexplained fertility." See E Hughes et al., "Clomiphene citrate for unexplained subfertility in women," Cochrane Database of Systematic Reviews, no. 1 (2010).
38. Pandian, Gibreel, and Bhattacharya, "In vitro fertilisation for unexplained subfertility."
39. S. Bhattacharya et al., "Clomifene citrate or unstimulated intrauterine insemination compared with expectant management for unexplained infertility: pragmatic randomised controlled trial," British Medical Journal 337, no. aug07 2 (2008).
40. Guzick and Queenanjr, "Evaluating the efficacy of intervention."
41. HKA Snick et al., "The spontaneous pregnancy prognosis in untreated subfertile couples: the walcheren primary care study," Human Reproduction 12, no. 7 (1997).
42. Guzick and Queenanjr, "Evaluating the efficacy of intervention."
43. Bhattacharya et al., "Clomifene citrate or unstimulated intrauterine insemination compared with expectant management for unexplained infertility: pragmatic randomised controlled trial."
44. Congregation for the Doctrine of Faith, "Instruction donum vitae on respect for human life at its origins and for the dignity of procreation," (1987); Congregation for the Doctrine of Faith, "Instruction dignitas personae on certain bioethical questions," (2008).
45. N. Gleicher and D. Barad, "Unexplained infertility: does it really exist?," Human Reproduction 21, no. 8 (2006).
46. Ibid.
47. Ibid.
48. Thomas W. Hilgers, The medical & surgical practice of NaProTechnology (Omaha, Nebraska: Pope Paul VI Institute Press, 2004).
49. J. B. Stanford, T. A. Parnell, and P. C. Boyle, "Outcomes from treatment of infertility with natural procreative technology in an Irish general practice," Journal of the American Board of Family Medicine 21, no. 5 (2008).
50. Ibid.
51. Phil C. Boyle, "NaProTechnology and pregnancy following failed ART," in The Medical & Surgical Practice of NaProTechnology, ed. Thomas W. Hilgers (Omaha, Nebraska: Pope Paul VI Institute Press, 2004), 673.
52. See Hilgers, The medical & surgical practice of NaProTechnology. and Thomas W. Hilgers, "Near adhesion-free reconstructive pelvic surgery " Journal Of Gynecologic Surgery 26, no. 1 (2010).
53. Richard J. Fehring, "Current medical research winter 2008-spring 2009 " The Linacre Quarterly 76, no. 4 (2009).
54. Stanford, Parnell, and Boyle, "Outcomes from treatment of infertility with natural procreative technology in an Irish general practice."
55. Ibid.
56. Pandian, Gibreel, and Bhattacharya, "In vitro fertilisation for unexplained subfertility."
57. Stanford, Parnell, and Boyle, "Outcomes from treatment of infertility with natural procreative technology in an Irish general practice."
58. Hilgers, The medical & surgical practice of NaProTechnology: 22.
59. Stanford, Parnell, and Boyle, "Outcomes from treatment of infertility with natural procreative technology in an Irish general practice."
60. Centers for Disease Control and Prevention, "2010 assisted reproductive technology: national summary report."
61. Chuck Weber, "The state of NaProTechnology," The Catholic World Report, February 2011.
62. Hilgers, The medical & surgical practice of NaProTechnology.
References
Bhattacharya, S., K. Harrild, J. Mollison, S. Wordsworth, C. Tay, A. Harrold, D. McQueen, et al. "Clomifene Citrate or Unstimulated Intrauterine Insemination Compared with Expectant Management for Unexplained Infertility: Pragmatic Randomised Controlled Trial." British Medical Journal 337, no. aug07 2 (2008): a716-a16.
Blank, Robert H. "Assisted Reproduction and Reproductive Rights: The Case of in Vitro Fertilization." Politics and the Life Sciences 16, no. 2 (September 1997): 279-88.
Boyle, Phil C. "Naprotechnology and Pregnancy Following Failed Art." In The Medical & Surgical Practice of Naprotechnology, edited by Thomas W. Hilgers. Omaha, Nebraska: Pope Paul VI Institute Press, 2004.
Catechism of the Catholic Church. New York: Doubleday, 1995.
Centers for Disease Control and Prevention. "2010 Assisted Reproductive Technology: National Summary Report." 2012.
____. "Infertility." http://www.cdc.gov/reproductivehealth/Infertility/index.htm - 1.
Chandra, A., and E. H. Stephen. "Infertility Service Use among U.S. Women: 1995 and 2002." [In eng]. Fertility and Sterility 93, no. 3 (Feb 2010): 725-36.
Congregation for the Doctrine of Faith. "Instruction Dignitas Personae on Certain Bioethical Questions." 2008.
____. "Instruction Donum Vitae on Respect for Human Life at Its Origins and for the Dignity of Procreation." 1987.
Fehring, Richard J. "Current Medical Research Winter 2008-Spring 2009 ". The Linacre Quarterly 76, no. 4 (November 2009): 427-45.
Gallup. ""Pro-Choice" Americans at Record-Low 41%." May 2012.
Gleicher, N., and D. Barad. "Unexplained Infertility: Does It Really Exist?" [In eng]. Human Reproduction 21, no. 8 (Aug 2006): 1951-5.
Groza, Victor, and Karen F. Rosenberg. Clinical and Practice Issues in Adoption. Westport, CT: Greenwood Publishing Group, Inc., 1998.
Guzick, D., and J. Queenanjr. "Evaluating the Efficacy of Intervention." Endocrinology & Metabolism Clinics of North America 32, no. 3 (2003): 709-23.
Helmerhorst, F. M., D. A. Perquin, D. Donker, and M. J. Keirse. "Perinatal Outcome of Singletons and Twins after Assisted Conception: A Systematic Review of Controlled Studies." [In eng]. British Medical Journal 328, no. 7434 (Jan 31 2004): 261.
Hilgers, Thomas W. The Medical & Surgical Practice of Naprotechnology. Omaha, Nebraska: Pope Paul VI Institute Press, 2004.
____. "Near Adhesion-Free Reconstructive Pelvic Surgery. " Journal Of Gynecologic Surgery 26, no. 1 (1 November 2010): 31-40.
Hoffman, DI, GL Zellman, CC Fair, JF Mayer, JG Zeitz, WE Gibbons, and TG Turner. "Cryopreserved Embryos in the United States and Their Availability for Research." Fertility and Sterility 79, no. 5 (2003): 1063-69.
Hughes, E, J Brown, JJ Collins, and P Vanderkerchove. "Clomiphene Citrate for Unexplained Subfertility in Women." Cochrane Database of Systematic Reviews, no. 1 (2010).
Hvidtjørn, Dorte, Laura Schieve, Diana Schendel, Bo Jacobsson, Claus Sværke, and Poul Thorsen. "Cerebral Palsy, Autism Spectrum Disorders, and Developmental Delay in Children Born after Assisted Conception: A Systematic Review and Meta-Analysis." Archives of Pediatric & Adolescent Medicine 163, no. 1 (2009): 72-83.
Jackson, R. A., K. A. Gibson, Y. W. Wu, and M. S. Croughan. "Perinatal Outcomes in Singletons Following in Vitro Fertilization: A Meta-Analysis." [In eng]. Obstetrics and Gynecology 103, no. 3 (Mar 2004): 551-63.
Luke, B. "The Changing Patterns of Multiple Births in the United States: Maternal and Infant Characteristics, 1973 and 1990." Obstetrics & Gynecology 84, no. 1 (1994): 101-06.
Mundy, Liza. Everything Conceivable: How Assisted Reproduction Is Changing Men, Women, and the World. New York: Alfred A. Knopf, 2007.
Nachtigall, R. D., G. Becker, C. Friese, A. Butler, and K. MacDougall. "Parents' Conceptualization of Their Frozen Embryos Complicates the Disposition Decision." [In eng]. Fertility and Sterility 84, no. 2 (Aug 2005): 431-4.
Neumann, PJ, SD Gharib, and MC Weinstein. "The Cost of a Successful Delivery with in Vitro Fertilization." New England Journal of Medicine 331, no. 4 (1994): 239-43.
Pandian, Zabeena, Ahmed Fathy Gibreel, and Siladitya Bhattacharya. "In Vitro Fertilisation for Unexplained Subfertility." Cochrane Database of Systematic Reviews, no. 2 (2005).
Reefhuis, J., M.A. Honein, L.A. Schieve, A. Correa, C.A. Hobbs, S.A. Rasmussen, and National Birth Defects Prevention Study. "Assisted Reproductive Technology and Major Structural Birth Defects in the United States." Human Reproduction 24, no. 2 (2009): 360-66.
Seoud, MA, JP Toner, C Kruithoff, and SJ Muasher. "Outcome of Twin, Triplet, and Quadruplet in Vitro Fertilization Pregnancies: The Norfolk Experience." Fertility and Sterility 57, no. 4 (1992): 825-34.
Snick, HKA, TS Snick, JLH Evers, and JA Collins. "The Spontaneous Pregnancy Prognosis in Untreated Subfertile Couples: The Walcheren Primary Care Study." Human Reproduction 12, no. 7 (1997): 1582-88.
Stanford, J. B., T. A. Parnell, and P. C. Boyle. "Outcomes from Treatment of Infertility with Natural Procreative Technology in an Irish General Practice." [In eng]. Journal of the American Board of Family Medicine 21, no. 5 (Sep-Oct 2008): 375-84.
The New York State Task Force on Life and the Law. Surrogate Parenting: Analysis and Recommendations for Public Policy. 1988.
Weber, Chuck. "The State of Naprotechnology." The Catholic World Report, February 2011.
Wimalasundera, R.C, G Trew, and N.M Fisk. "Reducing the Incidence of Twins and Triplets." Obstetrics & Gynecology 17, no. 2 (2003): 309-29.
Copyright © 2013 CHA. Permission granted to CHA-member organizations and Saint Louis University to copy and distribute for educational purposes. For reprint permission, contact Betty Crosby or call (314) 253-3490.