Mark Repenshek, Ph.D.
Director, Ethics Integration
Ascension Wisconsin
Glendale, Wisc.
Mark.repenshek@ascension.org
Core Competencies for Healthcare Ethics Consultation, 2nd edition from the American Society for Bioethics and Humanities, poses a challenge to ethicists in the opening section on Evaluating Healthcare Ethics Services, "Healthcare ethics consultation services should be able to demonstrate their value to those who pay for the service, as well as to those whom the service is intended to serve."1 A similar, yet somewhat more inflammatory challenge to the field was made nearly 25 years ago by Hoffman, "The fact that some legislatures and courts, and a powerful body like [The Joint Commission], appears to have wholeheartedly embraced these [ethics] committees is truly surprising given the paucity of data on their impact or effectiveness."2 Our field has vigorously responded to this critique and we continue to develop tools and metrics to assess the quality of the services provided.3 A more difficult task has been to determine how to measure the value of clinical ethics consultation services.4
This article will focus on three metrics that attempt to capture the value of a clinical ethics consultation service. Each of the three metrics will utilize quality data from the Premier Quality Advisor Database in order to establish deviations between observed and expected to value the outcome. By using deviation between observed and expected, the methodology avoids some of the critiques appropriately levied against outcomes-based assessments as a proxy "to the demands of the medical marketplace."5 Whether the outcomes-based assessment utilizes cost avoidance models,6 reductions in length-of-stay,7 or impact on treatment,8 each methodology may implicitly suggest ethics consultation should be utilized to reduce costs, lengths-of-stay or to achieve particular clinical outcome.9 In other words, deviation in observed versus expected avoids claims that clinical ethics consultation services should be operationally motivated to reduce cost or lower lengths of stay thereby creating "misalignment between outcomes-based assessment[s] and the intrinsic nature of clinical ethics consultation as a service."10
Methodology
Similar to a 2009 study in Health Care Ethics USA,11 this study utilizes the Microsoft Access database Ethics Tracker at Ascension Columbia St. Mary's in Milwaukee, Wisconsin. These data include clinical ethics consultations from 2009-2012.12 Clinical ethics consultation services throughout that period were based on the definition provided by ASBH's Core Competencies for Health Care Ethics Consultation which could be characterized as a service model that uses an ethics facilitation approach framed by the mission, vision and values of the health ministry. These data include consultations requested by any member of the health care team with direct patient contact as well as those from the patient, family member(s) or surrogate decision-maker(s).
In addition to data captured from the Ethics Tracker database, aggregate quality data was accessed from the Premier Quality Advisor Database for the following fields:
LOSexp Expected LOS (length of stay) is the risk-adjusted patient LOS.
LOSobs Observed LOS is the actual amount of days attributed to the patient's in hospital stay.
Chargesexp Expected Charges are the risk-adjusted charges associated with the LOS.
Chargesobs Observed Charges are the actual charges related to the in hospital stay.
Readmissionexp Expected Readmissions is the risk-adjusted readmission rate within 30 days of discharge from the index visit.
Readmissionobs Observed Readmissions is the actual 30 day readmission rate of the defined cohort in the proposal.
Each of these fields was used to compare observed versus expected for the outcome under analysis (e.g., LOS, charges, readmissions). Utilization of the Premier Quality Database on deviation of expected versus actual was found throughout Ascension's Clinical Excellence Programs which provided a statistically validated dataset for analysis.
Deviation, for the purposes of this study, is defined as the difference between the actual value and the expected (risk-adjusted) value for the outcome under analysis. A negative deviation (-) implies that the actual outcome was lower than predicted based on patient's characteristics when they were compared through Premier's risk adjustment methodology to similar patients in the comparative group. A positive deviation (+) implies that the actual outcome was higher than predicted based on the patient's characteristics when they were compared through Premier's risk adjustment methodology to similar patients in the comparative group. Deviation amount is expressed in the unit of measure for a particular outcome, for example, the deviation amount for LOS is days, charges is in dollars, etc.
Expected versus Observed Length of Stay (LOS)
Method:Mean time from the patient's admission date to the date of ethics consultation date is counted in days and stratified in the following way: under 1, 1-5, 6-10, 11-15 and 15+. Cohort comparison analyses are based on the difference between LOSexp and LOSobs on all adult patients in the ICU from 2010 to 2012 to determine whether an early or late ethics consultation impacted the length of stay.
Table 1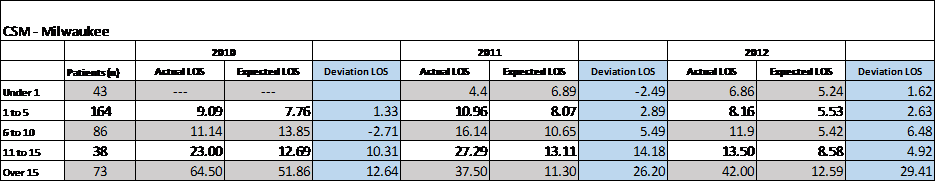
Results: When ethics consultation is called within one day (mean time) of admission, LOSexp versus LOSobs deviations were highly favorable relative to ethics consultation. Although in 2010 these data were not available, in 2011 the LOS deviation for those who received an early ethics consultation were -2.49 days below the risk adjusted expected LOS. In 2012, the LOS deviation was only marginally greater at 1.62. Somewhat favorable results were also seen when ethics consultation was requested one to five days after admission. In 2010-2012 the deviation LOS was 1.33, 2.89 and 2.63 respectively (see Table 1). These data suggest that when ethics consultation is requested close to the patient's admission the patient's observed LOS will closely match the patient's risk-adjusted expected LOS.
Conversely, when ethics consultation is requested well after the patient's admission date — eleven to 15 days or over 15 days — LOSexp versus LOSobs deviations are significantly less favorable. For example, in 2010-2012, when ethics consultation was requested more than 15 days after the patient's admit date, the deviation LOS was 12.64, 26.20 and 29.41 respectively (see Table 1). These data suggest that when ethics consultation is appropriately utilized more than ten days after the patient has been admitted the patient's observed LOS will vary greatly from the patient's risk-adjusted expected LOS.
Expected versus Observed Charges
Method: Similar to the previous analysis, mean time (in days) from the patient's admission date to the date of ethics consultation is stratified in the following way: under 1, 1-5, 6-10, 11-15 and 15+. Cohort comparison analyses are run on the difference between Chargesexp and Chargesobs for all adult patients in the ICU from 2010 to 2012 to determine the financial impact of early or late ethics consultation relative to admission date.
Table 2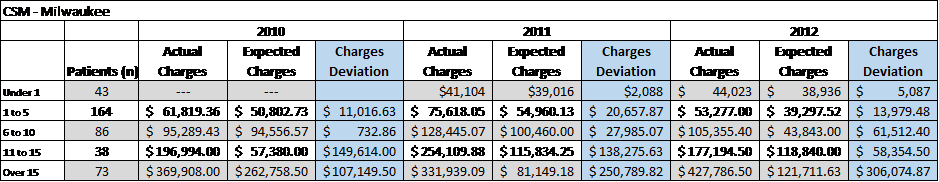
Results: When ethics consultation is called close to admission (within one day mean time of admission) Chargesexp versus Chargesobs deviations were favorable relative to ethics consultation. Although again in 2010 these data were not available, in 2011 the charges deviation for those who received ethics consultation was only slightly above the expected charges at $2,088. In 2012, the charges deviation was only marginally greater
at $5,087. Unlike the deviations in LOS that trended significantly upward when ethics consultation occurred further from the patient's date of admission, charges deviations increased when ethics consultation was delayed by more than a day after the patient's admission. These data suggest that when ethics consultation is appropriately utilized close to the patient's admission the patient's observed charges will closely match the patient's risk-adjusted expected charges.
Conversely, when ethics consultation is delayed even for a brief time after the patient's admission date, Chargesexp versus Chargesobs deviations are significantly less favorable. The most striking example occurred in 2010-2012. When ethics consultation was requested more than 15 days after the patient's admit date, the charges deviation was $107,149.50, $250,789.20 and $306,074.87 respectively (see Table 2). This suggests that when ethics consultation is appropriately utilized too far after admission, the patient's observed charges will likely vary greatly from the patient's risk-adjusted expected charges.
Expected versus Observed Readmissions
Method: We calculated the readmissions deviation between Readmissionexp and Readmissionobs for those ICU patients who received ethics consultation and for those ICU patients who did not receive ethics consultation from 2010-2012. For the purposes of this final method, only ethics consultations in the adult ICU met inclusion criteria.
Table 3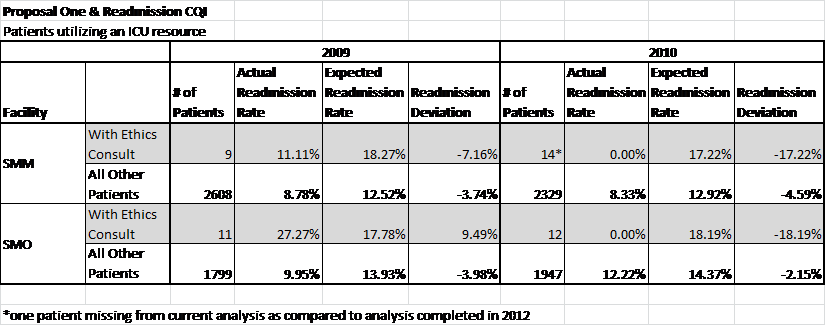
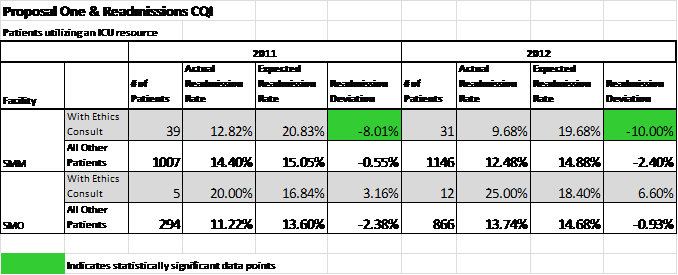
Results: In all years, 2009-2012, readmission deviations were favorable to the risk-adjusted readmissionobs for ICU patients who received ethics consultation. Most notably, readmission deviation in 2011 and 2012 represented a large enough cohort to reach statistical significance (p < 0.001 in green).
If we compare readmission deviation rates for adult ICU patients who received ethics consultation to all other adult ICU patients, the cohort positive for ethics consultation was favorable in all years 2009-2012. Impact on decreasing ICU readmission rates among patients who received ethics consultation continued from 2009 through 2012 even as the number of patients receiving ethics consultation increased. Finally, of note is the readmissionobs rate for 2010 which came in at 0.00% for the adult ICU patient population who received ethics consultation.
One limitation on this particular method is the inclusion of mortality in the readmission deviations rate. Although death is typically seen as a reviewable event from a continuous quality improvement standpoint, ethics consultation in which the patient's hospitalization resulted in death is not necessarily inconsistent with quality. For example, a consultation may recommend withholding resuscitation for a patient with profound comorbidities when the clinical team does not find the medical intervention of resuscitation of physiologic benefit to the patient. The patient's death does not mean the ethical consultation lacked quality.
Another limitation in this method is the relatively small number of patients in the "with ethics consultation"' cohort for 2009 and 2010. Although in 2011 and 2012 the same cohort did reach statistical significance, the field would certainly benefit from larger studies to determine whether these results are unique to the Ascension Columbia St. Mary's Milwaukee location.
Conclusion
Determining the value of clinical ethics consultations remains a challenge for the field. In addition, it is important in light of this challenge that we not use value as a synonym for quality. Quality in ethics consultation continues to focus on evaluation standards of structure, process and outcome.13 Assessments of structure and process are clearly important to an overall assessment of quality, but a high quality structure and process does not necessarily suggest the service is of value,14 and value is really what is at issue here. Outcome measures face additional critiques for at least two reasons: (a) outcomes are contingent on the nature of the consultation and (b) are often outside the control of the person providing ethics consultation.15 Value, on the other hand, is the demonstration of the contribution the service makes to the overall good of the patient. For Catholic health care that claim is circumscribed by our obligation to our identity and mission.
The proposed methodology offers three metrics to demonstrate the value of clinical ethics consultation relative to the overall good of healthcare delivery for the patient. These metrics are an attempt to contribute to the discussion of value without being subject to the critiques noted above. This methodology allows clinical ethics consultation to demonstrate its impact on established quality metrics rather than attempt to value the service through satisfaction assessments of either the user or recipient of ethics consultation. At the very least, this study attempts to value clinical ethics consultation services in a way that does not fall prey to an outcomes-based approach that may subvert or undermine the very nature of the service provided.
- American Society for Bioethics and Humanities (ASBH). Core Competencies for Healthcare Ethics Consultation, 2nd edition. (Chicago, IL: ASBH) 2011, 34.
- DE Hoffman. "Evaluating Ethics Committees: A View from the Outside." The Milbank Quarterly, v.71, no.4 (2011): 677-701
- R Pearlman, MB Foglia, E Fox, J Cohen, B Chanko and K Berkowitz. "Ethics Consultation Quality Assessment Tool: A Novel Method for Assessing the Quality of Ethics Case Consultations Based on Written Records." American Journal of Bioethics v. 16, no. 3 (2016): 3-14. American Society for Bioethics and Humanities. Improving Core Competencies in Clinical Ethics Consultation: An Education Guide. (Chicago, IL: ASBH) 2009; M Godkin, K Faith, R Upshur, S Macrae, and C Tracy. PEECE Group. Project Examining Effectiveness in Clinical Ethics (PEECE): Phase 1 — descriptive analysis of nine clinical ethics services." Journal of Medical Ethics v. 31, no. 9 (2005): 505-512.
- E Fox. "Evaluating Outcomes in Ethics Consultation Research." The Journal of Clinical Ethics v. 7, no. 2 (1996): 127-138.
- J Batten. "Assessing Clinical Ethics Consultation: Processes and Outcomes." Medicine and Law v. 32 (2013): 141-152; E Fox. "Evaluating Ethics Quality in Health Care Organizations: Looking Back and Looking Forward." American Journal of Bioethics Primary Research, v. 4, no. 1 (2013); B Lo. "Answers and Questions about Ethics Consultation." Journal of the American Medical Association, v. 290, no. 9 (2003): 1208-1210.
- BJ Heilicser, et al. "The Effect of Clinical Medical Ethics Consultation on Healthcare Costs" The Journal of Clinical Ethics v. 11, no. 1 (2000): 31-38.
- LJ Schneiderman, et al, "Impact of Ethics Consultation in the Intensive Care Setting: A Randomized Controlled Trial." Critical Care Medicine v. 28, no. 12 (2000): 3920-3924; MD Dowdy, et al. "A Study of Proactive Ethics Consultation for Critically and Terminally Ill Patients Extended Lengths of Stay." Critical Care Medicine v. 26, no. 2 (1998): 252-259
- LJ Schneiderman, et al, "Effect of Ethics Consultations on Non-beneficial Life-Sustaining Treatments in the Intensive Care Setting: A Randomized Controlled Trial." JAMA v. 290, no. 9 (2003): 1166-1172.
- Batten, 149; Heilicser, et al, 27.
- Batten, 146.
- M Repenshek. "An Empirically-Driven Ethics Consultation Service." HCE USA v. 17, no. 1 (2009): 6-17.
- The study received approval for research from the Research Oversight Committee at Ascension Columbia St. Mary's.
- ASBH, 34.
- Pearlman, 4.
- Batten, 147-148.
Permission granted to CHA-member organizations and Saint Louis University to copy and distribute for educational purposes.
