By JULIE MINDA
For nurses fresh out of nursing school, jumping immediately into hands-on care for patients can feel as foreboding as plunging into deep water to learn how to swim. Even seasoned nurses can feel a bit at sea when they start a new assignment in a specialized medical unit. By building a standardized education, training and mentorship program for new nurses and for those moving into specialty roles, Providence St. Joseph Health has created the equivalent of water wings for these newbies.

Trepanier
Sylvain "Syl" Trepanier, chief nursing executive for Renton, Washington-based Providence St. Joseph Health, says any newly minted nurse or seasoned nurse entering a new field of medicine in any of the seven-state system's 52 hospitals can take part in Providence Clinical Academy. The program is a requirement for the new nurses and an option for the seasoned nurses. It is available to nurses in all Providence care settings.
The recent nursing graduates enter a nurse resident track; nurses preparing for clinical specialties enter as fellows. Participants pay nothing to take part in the academy. They participate during their working hours.
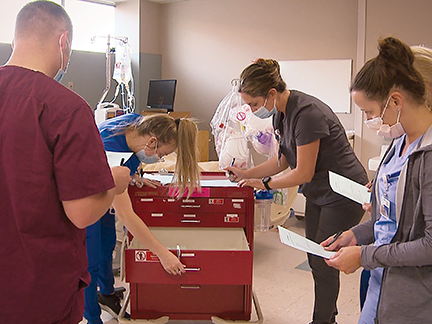
Nurse residents and fellows from Providence Sacred Heart Medical Center and Providence Holy Family Hospital in Spokane, Washington, get familiar with the contents of a code cart. The July 2021 exercise in a simulation lab was part of a Providence Clinical Academy "MedSurg Transition to Practice Class."
The academy provides a mix of online, in-person and training on simulators as well as preceptorships, in which the nurses are paired one-on-one with an experienced nurse for hands-on patient care. For the simulations, the academy usually uses high-fidelity medical manikins.
Trepanier says the academy enables nurses "to avoid the reality shock of transition and this allows for better outcomes for the nurses and for the organization. We've seen that the nurses have an increased level of competency and confidence. We've seen a higher level of engagement and retention with the nurses who go through the Clinical Academy."
'Wrapping our arms around'
The National Academy of Medicine recommends that hospitals have nurse residencies that include preceptorships to close the confidence and skill gap between education and nursing practice. Trepanier says although Providence facilities have offered preceptorships in all patient care settings for decades, before the academy was established there was great variation among Providence hospitals in the orientation protocols for new nurses. Many new nurses at Providence facilities had expressed unease about how ready they were for solo hands-on nursing.
In 2016, around the time that Providence Health & Services and St. Joseph Health merged to form the Providence system, leadership began developing and rolling out the clinical academy at all its sites. "Providence wanted to decrease the variation in practice (in how nurse onboarding was done) and be more mindful in demonstrating value and incorporating data and research into this programming," Trepanier explains.
The academy's programming includes didactic instruction. The curriculum designed by Providence subject matter experts uses content curated from professional nursing organizations. There is instruction in medical-surgical, telemetry, critical care, cardiovascular lab, emergency, perinatal care, oncology, orthopedics, case management, ambulatory, perioperative, pediatrics, home health as well as other areas. Work with a preceptor is a main draw in the fellowship program.
Both the fellow and resident tracks include self-directed training and training delivered to small groups of nurses.
Through the coursework and preceptorship, "we are wrapping our arms around" new nurses and fellows, giving them the support they need to do their jobs to the best of their ability, says Trepanier.
Two tracks
So far more than 10,000 nurses across Providence have graduated from the clinical academy, which does not offer degrees. The program is expanding: the number of graduates doubled from 2020 to 2021. The graduate count is expected to triple from 2021 to this year.
Incoming nurses in the residency program enter a 12-month Clinical Academy track, which includes 10-24 weeks of time with a preceptor depending on the clinical specialty. Participants can learn standard operating practices in clinical quality, safety, self-care and informatics and other areas. They get instruction on how to protect themselves against workplace violence and how to communicate with patients at the end of life, in order to understand their care wishes.
Trepanier says there is a "big emphasis on communication and how to best support mental health for both the nurse and the patients."
Program evaluation has shown that participation in the academy has had a positive impact on nurse engagement and retention and has improved patient care.

Allison
New connections
Laura Allison, a nurse in the medical oncology unit at Providence Alaska Medical Center in Anchorage, completed the residency track of the academy when she joined the hospital in 2018. She is now a preceptor for new nurses going through the academy.
Allison says the program was a safety net for her as she started her first job out of nursing school. Clinical precepting was vital to her confidence and skill building since she didn't get as much hands-on training as she would have liked to have had in nursing school. "You're not just thrown out on the floor, you're given the time and you're at a pace that you can ask questions," she says.
Another big plus was she got the opportunity to build relationships with other new nurses and meet people across the hospital.

Reinhardt
James Reinhardt, a staff nurse at Providence Sacred Heart Medical Center in Spokane, Washington, also was new to nursing when he enrolled in the academy in 2020. He says he learned practical lessons including how to have difficult conversations with patients. "It was comforting to know how I might be able to handle these complex, emotional situations."
He since has moved from the orthopedic unit to the trauma unit to the neurology unit, relying on academy courses to prepare him for each new assignment. Reinhardt says the people who taught the courses and who served as preceptors challenged him to "chase my goals."