By BETSY TAYLOR
U.S. Surgeon General Jerome Adams has been emphasizing the importance of a drug that reverses opioid overdose, calling on health care practitioners, patients using high doses of opioids for pain, those abusing opioids, and their friends, family and even members of the public to learn how to administer naloxone and keep it within reach.

Shaelah Easterday, pharmacy manager for Providence Pharmacy Monroe in Washington state, supports getting naloxone into more hands. The medication can reverse opioid overdose. Wendy Fagan/©CHA
Such steps can be lifesaving, Adams said when he issued an advisory early this year intent on increasing the availability and distribution of naloxone. In a speech at the American Hospital Association's Leadership Summit in July, Adams said, "We are not going to dig ourselves out of this hole unless everyone sees themselves as a first responder — everyone."
Ministry health care providers in Cincinnati, suburban Chicago and Monroe, Wash. — all areas hit hard by opioid use disorder — spoke about how they educate police officers, community organizations and individuals to recognize depressed respiration and other symptoms of an opioid overdose and administer naloxone to reverse the effects. The drug can be injected or administered as a nasal spray.
Naloxone works by binding to the opioid receptor sites in the brain. By preventing the opioid from binding to these receptors, it can reverse an overdose.
Normalizing naloxone
Dr. Stephen Feagins, vice president of medical affairs for Mercy Health's East Market, said that health care system had been working to get naloxone into the hands of more people before the surgeon general issued his advisory in March. (Mercy Health combined with Bon Secours Health System in September to form Bon Secours Mercy Health.)
Dr. Stephen Feagins, vice president of medical affairs for Mercy Health's East Market, administers a depression and a substance abuse screening that Mercy Health uses with all patients.
Photo courtesy of Mercy Health
Feagins, who carries two doses of naloxone in his car, said the surgeon general's efforts to increase the availability and distribution of the drug validates and reinforces the societal importance and clinical relevance of Mercy Health's efforts to combat the opioid epidemic.
Mercy Health is part of a larger effort in the Cincinnati region to get more opioid antidote doses out into the community and train more people to use it in an emergency. ADAPT Pharma, the company that manufactures naloxone under the brand name Narcan, has donated doses of the drug to the effort, Feagins said. In the week he spoke to Catholic Health World training sessions were conducted at meetings of Parents of Addicted Loved Ones, certified athletic trainers and infection control practitioners. Nationally, more school systems and even some public library staffs are training on how to administer the medication.
In training sessions, participants learn to recognize symptoms of an overdose. These include pinpoint pupils, where the center of the eye is very small; the person not waking or responding to voice or touch; fingernails and lips turning blue and breathing that is slow, irregular or has stopped.
The responder delivering first aid can administer naloxone by spraying it into one nostril of the person suspected of opioid overdose. In some cases, a second dose is administered. (ADAPT Pharma emphasizes naloxone is not a substitute for emergency medical care.) Naloxone also can be administered by an injection or through an IV, but that is more often done by medical professionals.
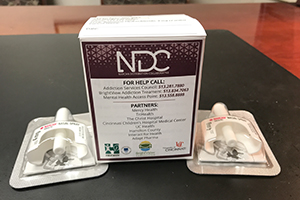
Mercy Health in Cincinnati is part of efforts to get more naloxone out into the community and train more people to administer the opioid antidote in an emergency. Photo courtesy of Mercy Health
Opioids are the main reason that overdose deaths have spiked across the nation. They were involved in 42,249 overdose deaths in 2016, out of 63,632 drug overdose deaths in the country, according to the Centers for Disease Control and Prevention. Adams told the AHA audience that 2.1 million people struggle with opioid use disorder in the U.S., where an opioid overdose claims a life every 12 and a half minutes.
"In most states, people who are, or know someone at risk for opioid overdose can go to a pharmacy or community-based program to get trained on naloxone administration, and receive naloxone by standing order," without a patient-specific prescription, Adams said in his advisory. He told the AHA audience that retail-dispensed doses of naloxone increased 40 percent in the first month after the advisory.
Financial barriers
Illinois passed a law in 2015 to require police officers to carry naloxone, but costs and limited access to training meant that many departments couldn't initially comply. Illinois received federal grants in 2017 and 2018 that provided funds for opioid overdose response training for first responders.
A $311,000 Edward Byrne Memorial Justice Assistance Grant provided additional federal funding that allowed Loyola Medicine and the Cook County Department of Homeland Security and Emergency Management to collaborate on training last year and this year, and to provide the drug when they educate police and other law enforcement officers about how to administer naloxone. The same training also includes lessons on how to apply a tourniquet to control hemorrhagic bleeding from a penetrating injury such as a gunshot wound.
Cook County had more than 1,000 opioid-related deaths last year, according to information from Loyola Medicine, the Maywood, Ill.-based health system which is part of Trinity Health.

Cichon
Loyola Medicine's Dr. Mark Cichon, chair of emergency medicine and director of emergency medical services, said a train-the-trainer approach has resulted in about 300 trainers then educating about 5,000 people, mainly police officers and other law enforcement officers about how to administer naloxone.
Law enforcement officers who participate in the training leave with one dose of naloxone to carry with them and a tourniquet. Paramedics and emergency medical technicians also carry the medication and are trained in administering it, as standard preparation for their jobs. Illinois law also allows non-medical persons to administer naloxone to a person experiencing an overdose.
Cichon said he wants people to know that after administering the opioid antidote, a call should be made to 911 to initiate emergency care. A person who survives an opioid overdose may be receptive to medical detoxification and substance abuse treatment, he said.
Pharmacist support
Shaelah Easterday, pharmacy manager for Providence Pharmacy Monroe in Washington state, said three or four years ago, she was filling about one naloxone prescription a month. "Now we get maybe one a week." She said clinicians are prescribing the medication more often when they prescribe opioids, as a safety net against accidental overdose. (The risk of overdose increases if a person combines opioids with benzodiazepines or alcohol.)
She said she and her pharmacist colleagues have a Collaborative Drug Therapy Agreement filed with Washington state's Pharmacy Quality Assurance Commission allowing them to prescribe and dispense naloxone without a patient having to get a prescription from a doctor. Such agreements are filed yearly and are used for some other widely distributed medications like immunizations.
If Easterday is filling a prescription for someone on high doses of an opioid, she asks if they want naloxone. It may be covered by insurance, sometimes with a co-pay, or can be paid for out-of-pocket at a cost of about $50 for a generic naloxone injection and $160 for Narcan nasal spray. Out-of-pocket costs for the drug can be a barrier. Most people who get the medication can do so only because it's covered by insurance, she said.
"One of our main roles is to educate patients," she said, so she'll explain the signs of overdose, saying people can rub their knuckles against someone's chest or gumline to try to rouse them. If they are unable, she advises people to give naloxone first, then call 911 and begin rescue breathing. She tells people they can administer a second dose of Narcan if the first dose doesn't reverse the overdose.
She said she supports having naloxone in more hands. "It's a safe medication to use," she said. "I think it would be great to make it over the counter and not require a prescription."
Additional materials from U.S. Surgeon General Jerome Adams' office:
Facing Addiction in America — The Surgeon General's Spotlight on Opioids
Other recent materials: https://addiction.surgeongeneral.gov/
|
Circumstances that increase risk of overdose
The Surgeon General's office says there is elevated risk for an opioid overdose if someone:
- Misuses prescription opioids, such as oxycodone, or uses heroin or illicit synthetic opioids, like fentanyl or carfentanil.
- Has an opioid use disorder, especially those completing opioid detoxification or being discharged from treatment that does not include ongoing use of methadone, buprenorphine or naltrexone.
- Recently has been discharged from emergency medical care following an opioid overdose.
- Has recently been released from incarceration with a history of opioid misuse or opioid use disorder. (Dose tolerance falls with abstinence.)
Additionally, patients taking opioids as prescribed for long-term management of chronic pain, especially those with higher doses of prescription opioids or those taking prescription opioids along with alcohol or other sedating medications, such as benzodiazepines (anxiety or insomnia medications), are at elevated risk for an overdose.
|
Copyright © 2018 by the Catholic Health Association
of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3490.