By KATHLEEN NELSON
CHESTERFIELD, Mo. — The first visuals to greet visitors to Mercy's new Virtual Care Center — $54 million worth of tech and virtual virtuosity that is part of the system's roadmap to the future — invite contemplation.

A small lake and a stand of trees enhance the tranquil grounds of Mercy's Virtual Care Center, which hosted a grand opening Oct. 6 in Chesterfield, Mo. In this view, the main entrance is on the right side of the building.
The four-story glass and steel open architecture building is perched on a lakeshore and nestled amid a stand of trees in a quiet and relatively secluded setting, given that it's just a few hundred yards from a busy intersection in suburban St. Louis. The facade is enhanced by a tall, vertical light feature called the Lantern, which symbolizes Mercy's call to share light with others. The chapel is just inside the front entrance. And, dominating the first-floor atrium is the Pioneer Wall, an array of 10-foot video screens that project photos from the late 1800s and early 1900s of the system's founders, the Sisters of Mercy. The order is known as the "walking sisters" because they sought out, and walked among, those they served.
"Like the walking sisters before us, we are extending care to those people who need it," said Lynn Britton, Mercy's president and chief executive. "We're not waiting for people to come to us. We're bringing care to them."
But Catherine McAuley, founder of the Sisters of Mercy, could not have envisioned a facility like the Virtual Care Center with 330 internists, neurologists, nurses, nurse practitioners, intensive care specialists and support staff, but not a single patient inside its walls.
The services now clustered at the Virtual Care Center augment direct patient care in five states. Telemedicine is used to enhance access to services particularly in rural and remote areas, where the demand for physicians often exceeds the supply.
Clustering services
"Everything in this building was going on in some form elsewhere in one of our facilities," said Dr. Randy Moore, president of Mercy Virtual. "But here, there's room to grow each program and more opportunity for collaboration."
Nurses such as Trina Cooper are available 24 hours a day to answer medical questions through the Mercy Nurse On Call program, which has been expanded since the opening of the Mercy Virtual Care Center.
The bulk of Mercy's virtual programs are housed on the second floor. The centerpiece is Mercy SafeWatch, which the system hails as the largest single-hub electronic intensive care unit in the nation. That service doubled its work space from its original home at Mercy Hospital St. Louis. Nurses with an average of 18 years of ICU experience work with a team of doctors to monitor patients in 30 of Mercy's ICUs, including its St. Louis flagship hospital nearby. Dr. Christopher Veremakis, medical director of inpatient services at Mercy Virtual, said that the virtual ICU staff provides "a second set of eyes, a second layer" of monitoring and has not changed staffing levels in the ICUs.
SafeWatch is linked to the electronic medical records system at each hospital. In addition to monitoring vital signs, lab reports and staying alert for warnings of sepsis, the SafeWatch team can talk with and see patients through a two-way audio/video system in each room. Veremakis noted that two ICUs using SafeWatch are outside of Mercy's system. In addition, 10 more ICUs from other health systems are in some stage of contracting with SafeWatch. Mercy Virtual also supports 32 remote clinics with services such as pediatric neurology, genetic counseling, maternal fetal medicine, and behavioral health.
Other telemedicine programs at the center include:
Telestroke: Hospitals without a neurologist on-site connect with Mercy neurologists who make decisions on whether clot-busting drugs should be used in the critical hours following a stroke.
Virtual hospitalists: A team of doctors at the center supplement in-patient medical care at client hospitals.
Home monitoring: In-home telehealth equipment transmits vital signs and data from home care patients to the Virtual Care Center. Patients using the monitoring system are at high risk for relapse after their discharge from the hospital. The goal is to spot emerging problems and notify attending physicians, who can act to stabilize the patient and avoid a rehospitalization.
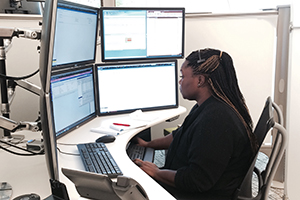
Nurse on call: At this, the second of Mercy's nurse call centers, nurses talk to patients by phone and use a bank of four computer screens at each station to call up patient records, use assessment tools to help in diagnosis, and view a network map to guide a patient to the nearest facility, if necessary.
Creative space
The third floor is shell space for future growth, "wherever that might take us," said Julie Jones, executive director of mission and ministry for Mercy. That could be training simulations for staff, new telemedicine programs or growth in the existing virtual coverage areas.
The fourth floor has been nicknamed the "workshop/garage," and is designed to be conducive to creative thinking and collaboration among associates throughout Mercy's system, as well as with current and future business partners outside the system. Meeting rooms are dubbed Think Tank 1 and Think Tank 2. The central area features a fixed wall of 30 contiguous video screens and moveable walls to configure the space as one large area or several small ones. Each of the moving walls is covered floor to ceiling in white boards.
"We want to learn together, from everyone," said Michael Chappuis, Mercy Virtual's chief administrative officer. "We're welcoming health systems who want to bring care in a different manner. Let's collaborate."
Time and money
Mercy proudly declared at the official opening of the Virtual Care Center on Oct. 6 that its facility is the first in the world dedicated entirely to care for patients outside the facility's walls.
Moore noted that Mercy was beginning to see cost savings in such programs as SafeWatch, which reported a 15 percent reduction in length of stay for patients versus the national predictors. Such savings can benefit Mercy and its telemedicine clients directly in the future, as care moves away from fee-for-service to value-based reimbursement.
"We're going to be paid more lump sums to manage health care," he said. "With our ability to share resources here, that will work to our advantage." So far, though, Medicare has been reluctant to pay for virtual medicine except for patients in rural areas, and other insurers have followed that lead.
To those who say that compassionate caregiving is sacrificed when clinicians are miles away, Moore responds that "virtual care never replaces personal care but it augments it. In fact, it can free up some care providers to spend more time with patients. The more we can do here, the more time that doctors and nurses in the hospital can spend with patients."
| Virtual Care Center built to withstand external hazards The technology and electrical systems at Mercy's Virtual Care Center have built-in redundancies to ensure the facility will not lose power or experience a service disruption due to a tornado, earthquake, or disruption of the power grid, according to Maryann Copenhaver, executive director of business partnerships for Mercy Technology Services. The safeguards include: - Data lines that enter the building in three separate places and run to two separate data rooms in the building. Each of the data rooms is independent of the other and backs up the other in case one becomes nonoperational. Copenhaver said the system's applications and servers all reside in the Mercy system's Washington, Mo., central data center.
- A pair of uninterrupted power supplies, which turn on automatically in the event of a power outage and run continuously to maintain power in the building until the generator kicks in.
- An on-site diesel-powered generator that can maintain core function for 24 hours without refueling. "Our practice would be to refuel every eight hours until power is restored," Copenhaver said, adding that the generator is tested weekly.
- No copper is used outside the building to prevent damage from lightning strikes.
|
Copyright © 2015 by the Catholic Health Association
of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.