By KEN LEISER
When Arkansas expanded its Medicaid program in January 2014, it opened the door to more than 225,000 people who obtained coverage during the first two years. The Arkansas Health Care Independence Program, a nonpartisan agency, reported the state saw the sharpest decline in the uninsured rate in the nation during that time.
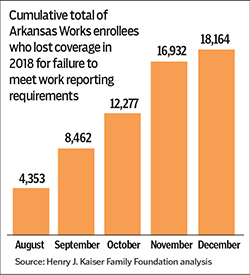 Today, Catholic health systems and others are closely monitoring the new state Medicaid waiver that conditions Medicaid eligibility on meeting work requirements and reporting rules, which Arkansas rolled out in mid-2018. As of December, over 18,000 Medicaid beneficiaries had lost coverage during the previous 6 months, which will likely cause a significant increase in uncompensated care as the number of uninsured is expected to increase from the Medicaid coverage losses.
Today, Catholic health systems and others are closely monitoring the new state Medicaid waiver that conditions Medicaid eligibility on meeting work requirements and reporting rules, which Arkansas rolled out in mid-2018. As of December, over 18,000 Medicaid beneficiaries had lost coverage during the previous 6 months, which will likely cause a significant increase in uncompensated care as the number of uninsured is expected to increase from the Medicaid coverage losses.
Arkansas Gov. Asa Hutchinson in September said the state is committed to ensuring those who qualify under Medicaid expansion keep their coverage. But stressing "personal responsibility," Hutchinson added that it is just as important to ensure those who no longer qualify are removed from the rolls.
"This work requirement not only provides Arkansans with an opportunity to gain employment and move up the economic ladder, but also allows the state to concentrate our limited resources on those who need it most," he said.
Lisa Smith, CHA's vice president for advocacy and public policy at CHA, said, "CHA supports states referring Medicaid beneficiaries to job training and referral programs, but does not support conditioning Medicaid eligibility on work requirements."
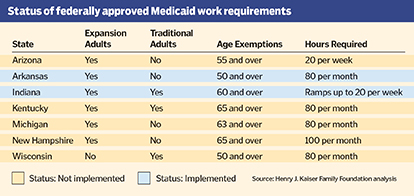 The Arkansas Works program requires thousands of beneficiaries of Medicaid expansion under the Affordable Care Act to document monthly through an online portal or, more recently, the state's Department of Human Services Hotline call-in service, that they have worked for pay, or have been involved in job training or approved volunteer work for a minimum of 80 hours per month.
The Arkansas Works program requires thousands of beneficiaries of Medicaid expansion under the Affordable Care Act to document monthly through an online portal or, more recently, the state's Department of Human Services Hotline call-in service, that they have worked for pay, or have been involved in job training or approved volunteer work for a minimum of 80 hours per month.
Expanded reach
The work requirements initially affected Medicaid beneficiaries age 30 to 49. On Jan. 1, the work requirements were extended to beneficiaries age 19 to 29. Enrollees who fail to comply for any three months lose coverage for the rest of the calendar year and are barred from reapplying for coverage until the following January.
Smith said it is thought that the large losses in Medicaid eligibility likely reflect the difficulties that those who are not exempt from filing monthly reports of their work activity to the state encounter because they either do not have access to a computer and an internet connection or they have difficulty navigating the online reporting portal. The state began allowing people the option to report work activity by phone beginning Dec. 19.
In an issue brief published in January, the Henry J. Kaiser Family Foundation said that many people who are required to report work hours have not been informed of that obligation despite "substantial outreach and education efforts" on the part of the state.
There are limited exemptions to the work requirement including disability or caring for an incapacitated family member, however the exemption must be recertified every two months. Individuals attending school, over age 50, caring for a young child or in job training full-time are also exempt.
Watchful waiting
Ben Barylske is chief financial officer of Jonesboro, Ark.-based St. Bernards Healthcare. He said it's too early to tell if the Medicaid work rules are causing an uptick in the number of uninsured patients at the system's two hospitals in Northwest Arkansas. "We will continue watching the numbers over the next year," he said.

Barylske
In their separate 2016 Community Health Needs Assessment reports, the two hospitals reported significant declines in the uninsured rates for those facilities. They attributed those improvements in large part to Arkansas' Medicaid expansion. In 2013, prior to the expansion, 16 percent of patients seen at the system's CrossRidge Community Hospital in Wynne, Ark., were uninsured. By 2015, that number was 8 percent. At St. Bernards Medical Center in Jonesboro, those numbers were 12 percent and 7 percent, respectively.
Executives of Little Rock, Ark.-based CHI St. Vincent said that it is too early to know how the work rules will impact the payer mix at its four hospitals and more than 70 primary care, specialty care and community clinics in Arkansas.
Bonnie Ward, senior communications strategist for CHI St. Vincent, said, "We don't just look at these changes from that type of a financial perspective. We also look at it from a service perspective, and say, 'Do we have what we need in the community to serve the patients if they are affected by an insurance change, or lose insurance?'"
Seven states secure waivers
So far, the U.S. Department of Health and Human Services has granted waivers to seven states seeking the green light to impose work requirements for Medicaid benefits, according to the Kaiser foundation. Arkansas was the first state to launch its program when it did so last June, and it is one of two currently operational. Indiana started its program in January. A federal judge, for now, has blocked Kentucky from enforcing its Medicaid work requirements.
In Kentucky, CHA joined six other national health care organizations to submit an amicus brief supporting plaintiffs who have challenged the federal government's authority to approve that state's Medicaid waiver, which permitted work requirements. CHA and other organizations argue that work requirements would lead to "mass disenrollment" and worsen health outcomes, impose new burdens and penalties on Medicaid beneficiaries that threaten the coverage of "even the gainfully employed," and expose beneficiaries, providers and the state to potential financial losses.

De Liban
Smith added that CHA and its members have for decades carried the message that health care is a basic human right essential to human flourishing "and we have advocated policies to ensure that everyone has access to affordable health care."
The National Health Law Program, the Southern Poverty Law Center and Legal Aid of Arkansas have sued the Department of Health and Human Services and the Centers for Medicare and Medicaid Services, claiming that, when they enacted the work rules in Arkansas, regulators bypassed the legislative process to fundamentally transform Medicaid.
"What they are trying to do (through an administrative action) is radically restructure Medicaid, something they couldn't achieve in Congress," said Kevin De Liban, an attorney for Legal Aid of Arkansas and co-counsel in the federal lawsuit. "And that is just not appropriate. Medicaid is and always has been a health insurance program. We all recognize that health is a precursor to working. You need health insurance in order to maintain your health ... to be able to work."
De Liban said he hopes the case can be decided by March 31 — the first date Arkansas Medicaid enrollees can be terminated in 2019 under the work requirements.