By PAMELA SCHAEFFER
Data dashboard identifies hospitals potentially overprescribing the drugs
"A post-antibiotic era in which common infections and minor injuries can kill — far from being an apocalyptic fantasy, is instead a very real possibility for the 21st century" ... one that is "no longer a prediction for the future" but "is happening right now in every region of the world."

Photo courtesy of St. Vincent's HealthCare
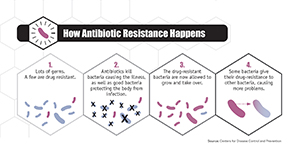
That was the assessment of the World Health Organization in April 2014, when it issued its first report on the global problem of antimicrobial resistance, an umbrella term for a group of drugs that includes antifungals, antiprotozoals, antivirals and those bacteria fighters of most immediate concern — the antibiotics.
Fast-forward 14 months to June 2015, when representatives of 150 organizations attended the White House Forum on Antibiotic Stewardship to showcase their strong commitments to combatting antibiotic resistance. Among participants, which included food companies, retailers and other stakeholders in human and animal health, was St. Louis-based Ascension.
Ascension was among only four participating health care organizations, joining Hospital Corporation of America, Intermountain Healthcare and Kaiser Permanente.
Ascension's contribution was its five-year plan to fully implement antimicrobial stewardship programs in each of the 131 hospitals nationwide that is part of Ascension Health, then in outpatient settings and nursing homes.
Ascension started its system-wide approach to optimizing antibiotic use two years ago. Initially, a focus on selected antibiotics led to establishing criteria for their use at all hospitals. Then, a national multi-disciplinary antimicrobial stewardship committee consisting of physicians, pharmacists and other expert medical professionals was formed to provide best practice recommendations for implementation. Heading up this committee are Dr. Mohamad Fakih, Ascension's national infectious diseases physician leader, and Roy Guharoy, Ascension's chief pharmacy officer.
Precious resource
Reducing resistance to antibiotics is critical, Guharoy said, "because the number of antibiotics is limited and few new antibiotics are coming on the market — including very few new agents that can overcome very resistant bacteria."


Ascension's hospital program began with "a lot of data mining," Guharoy said, gathering information on antibiotic usage at large and small hospitals throughout its system, determining the acuity level of patients receiving antibiotics and the presence of antibiotic resistance.
What the data showed was counterintuitive and pointed up the need for greater oversight and education, said Fakih: Antibiotic usage was greater at smaller hospitals than at larger, though in general, the patients are less sick. He attributed the imbalance to lack of guidance for medical professionals at smaller hospitals on when to order antibiotics, which ones to use and how long to use them before switching to a more targeted antibiotic or stopping antibiotics altogether.
The results highlighted the need for system-wide protocols governing antibiotic use.
Overcoming resistance
Ascension's next step was to begin work on an infrastructure that would provide for system-wide monitoring of antibiotic use, one of seven core elements of the antimicrobial stewardship program promoted by the Centers for Disease Control and Prevention.
"We began immediately by getting involved with our local hospital leadership to begin working on usage criteria" to promote optimal use of antibiotics, Guharoy said. "It is very complex work, because antibiotics are used very frequently."
Guharoy said the committee anticipates — and is prepared to deal with — a bit of balking by some physicians. In such cases, the national committee will partner with the local committee to engage any doubters. "Already thousands of pharmacists are engaged," he said.
Local accountability
Fakih said Ascension's national antimicrobial stewardship committee operates as a think tank, proposing plans that are then approved by the Therapeutic Affinity Group. All decisions taken at the Therapeutic Affinity Group are required to be implemented by local facilities.
"We are working on establishing local antimicrobial stewardship teams at every hospital," he said. The goal is for every hospital to have at least a dedicated pharmacist and physician accountable for implementing the improvements locally. Hospital leadership, usually the chief medical officer, is essential to the local success by supporting the team. "We need accountability at the local level in order to adopt best practices across the system and standardize the treatment of common infections" — infections such as community-acquired pneumonia. Fakih added that standardization of care for common conditions will lead to better outcomes. Antimicrobial stewardship ties in to previous efforts to reduce healthcare-associated infections and organism transmission. Ascension continues to engage nurses with protocols to reduce infection risk to patients, and it plans to educate patients and families on the importance of judicious antibiotic use.
Meanwhile, the national antimicrobial stewardship committee closely monitors and engages underperforming hospitals throughout the system and promotes the use of best diagnostic practices, including ordering the most precise tests possible to assure the most effective use of antibiotics. "We want to make sure that whatever test is being ordered reflects the best care of the patient and will help us get the right diagnosis," said Fakih.
When antibiotics are used inappropriately, "they can cause tremendous patient harm," Guharoy said. Negative side effects can range from damage to cells and organs to a virulent and sometimes deadly form of diarrhea caused by the bacterium Clostridium difficile, commonly known as "c-diff."
"All that we're doing is based on evidence, so if a given infection needs treatment for five days and gets ten, there is no reason for that. We want to be sure physicians abide by the best practice guidelines."
'Hey, do something'
Guharoy leads the effort to evaluate the performance of all Ascension hospitals and their antibiotic use, producing a monthly dashboard showing how many antibiotics are purchased at individual Ascension hospitals across the entire system. Each hospital receives a usage target according to its size. Fakih said hospitals using excessive antibiotics compared to similar-sized hospitals will be highlighted on the dashboard, giving them the opportunity to identify instances, if any, where antibiotics might have been inappropriately used. "This will make a huge difference and affect the behavior of our local hospitals," he said.
Another tool critical to Ascension's quest to improve its antimicrobial use is medication management software, currently being phased in all its hospitals. Guharoy noted that the software gathers information from hospital pharmacy data and matches it with laboratory reports. If there is a mismatch, the pharmacists are alerted that something is wrong. "For example, a patient may be getting an antibiotic he does not need. Or an alert may indicate a more appropriate antibiotic should be used. It basically tells the clinician, 'Hey, do something.'"
Narrow-spectrum therapies
Florian Daragjati, pharmacy clinical manager at the 310-bed St. Vincent's Medical Center Southside in Jacksonville, Fla., said a major goal of Ascension's stewardship program is to be sure doctors use the most effective and specific weapon against particular infections and minimize use of broad spectrum antibiotics, according to the best available medical evidence &mdash evidence indicating that the narrower the spectrum of the antibiotic prescribed for a patient, the less likely that patient will develop resistance.
The national antimicrobial stewardship committee also discourages the unnecessary prolonged use of antibiotics whether for surgical prophylaxis or the treatment of infection. In addition, broad spectrum agents (Ceftaroline and Tigecycline, for instance) are restricted for use only when the bacteria is resistant to other, older established agents.
Broad spectrum antibiotics target a range of different bacteria and are often used when a patient goes to the emergency room with an undetermined infection, Daragjati said. The purpose is to ensure the infection doesn't turn deadly before doctors can identify the organism causing distress and prescribe a more narrowly focused medication.
Sometimes, though, doctors are hesitant to switch medications, especially if the patient is improving and they lack training in infectious diseases.
Showing restraint
Bacterial resistance to antibiotics can develop in a number of ways, but the best way to combat its development is by reducing exposure to antibiotics, Fakih said. So optimal patient treatment indicates using antibiotics only when truly needed and using the narrowest spectrum possible for the shortest possible duration.
Daragjati, a member of the national antimicrobial stewardship committee, said his hospital is among several that already had local antibiotic stewardship programs in place when the national committee was formed. The aim of the national committee, he said, is "to tie everything together for all of our ministries and improve utilization nationwide."
The national committee also will develop guidelines and recommendations for using new antibiotics. For example, Guharoy said, "Maybe an antibiotic will come into the market that would be best used for outpatient only because it can stay in the blood a long time and needs to be taken only every three to seven days."
At the present, he said, antibiotic usage can be tracked across the health system only by analyzing purchase information. But Daragjati anticipates that within a few years, it will be possible to analyze specifics of usage more closely.
Based on purchase-related tracking in just the first year of the program, Ascension can demonstrate some significant success, Guharoy said: a reduction of 17 to 46 percent in four antibiotics (Ceftaroline, Tigecycline, Linezolid and Daptomycin used to treat infections caused by Methicillin-resistant Staphylococcus aureus, or MRSA). The national antimicrobial stewardship committee had targeted these drugs for reduction in use.
Daragjati and others on the national committee credit Ascension leadership for supporting the trailblazing program. "These programs incur costs that are not reimbursed," Daragjati said. "So leadership commitment is absolutely necessary."
 Facts about overuse of antibiotics The Centers for Disease Control and Prevention's Get Smart About Antibiotics Week, Nov. 16-22, is intended to raise awareness of the threat of antibiotic resistance and the importance of appropriate antibiotic prescribing and use. Resources are available at cdc.gov/getsmart/week. According to the CDC:
|
Essential elements of antibiotic stewardship Clearly, antibiotics save lives. However, according to the Centers for Disease Control and Prevention, 20 to 50 percent of all antibiotics prescribed in U.S. acute care hospitals are either unnecessary or inappropriate and may cause serious adverse reactions. The misuse of antibiotics contributes to antibiotic resistance, considered to be one of the most serious and growing threats to public health. As a result, the CDC has made smart antibiotic use a national priority and is urging hospitals to establish programs dedicated to that goal. Below are the core elements the CDC has identified as key to a successful antibiotic stewardship program, such as the one at Ascension.
|
