
Dr. Mark Kantrow still remembers when it clicked for him exactly how important palliative care is in medicine.
It was around 2006, and he had just attended his first conference on palliative care, at a time when the concept was new to him and to many other clinicians. On a cab ride to the airport for his return trip, Kantrow called his program director back home in Baton Rouge, Louisiana.
"I remember telling him I felt like I had just been shown a chapter out of the textbook of medicine that nobody knew about," Kantrow says. "It was like this secret information — like how to engage patients and families and how to address suffering. It was an eye-opening experience for me."
That experience launched Kantrow into a career — nearly two decades and counting — centered on spreading palliative care to as many clinicians and locations as possible within Baton Rouge-based FMOL Health, formerly Franciscan Missionaries of Our Lady Health System.
"What we are doing is addressing patients as a whole person," Kantrow explains. "We are addressing their suffering based on a deeper understanding of what is important to them."
Part of a team
Kantrow says before becoming a palliative care practitioner, he was a hospitalist who had been growing frustrated with having to provide medical care in a way that focused almost solely on patients' medical conditions, and not on the full picture of their broader needs. "I was starting to feel like I had a front row seat to see all of the patients' suffering," he says, "but I didn't have any of the skills to address all the levels of that suffering."
At the prompting of a sister with FMOL Health's sponsoring congregation, Kantrow started to learn about palliative care and immediately saw the value. After studying the approach, he began a palliative care consult service at FMOL Health's flagship hospital, Our Lady of the Lake Regional Medical Center in Baton Rouge. He says even though he worked hard to educate clinicians, patients and family about the value of the consultations, it took a long time for him to gain acceptance and build momentum for his practice. He explains that many staff and patients mistakenly associated his work solely with dying, and that made clinicians reluctant to welcome him into their healing work.
Over time, Kantrow has proven the value of palliative care to greatly enhance patient, family and staff experience and to improve patient outcomes. That has led to great growth in the service at Our Lady of the Lake and paved the way for Kantrow's eventual promotion to his current system-level role.
Branching out
Kantrow's focus is to ensure patients and families can access the whole-person approach to medicine that palliative care promotes. This is a formidable challenge in a system with many smaller, rural hospitals with chronic financial and workforce strains.
He's been working with colleagues throughout FMOL Health's catchment area in Louisiana and Mississippi to build awareness of palliative care and to gain leadership buy-in. He helps ensure staff at the facilities learn about palliative care. He works with leadership to pull together multidisciplinary teams at each hospital to provide palliative care to patients. He is working with academic partners to offer palliative care education to the providers. He facilitates their clinical training in holistic care, incorporating visits to Our Lady of the Lake. He supports the team in-person and through virtual connections.
He's made a video series to educate patients and their families and others on palliative care concepts.
Kantrow also helped establish and now directs a palliative care fellowship at Our Lady of the Lake. Some of those fellows are job candidates for palliative care positions at FMOL Health sites.
Kantrow also serves as president of the board of the Louisiana–Mississippi Hospice and Palliative Care Organization. That organization supports advocacy and education in both states.
For his efforts to advance palliative care, Kantrow recently received the James Block Award for Ethical Leadership in Health Care. The Center to Advance Palliative Care gave Kantrow the award at its national seminar in September. CAPC says in an online biography on Kantrow that he has led efforts to improve access, policy, and workforce training to support patients with serious illness. It says "his work centers on listening to all voices in care — patients, caregivers, and clinicians — to ensure palliative care in the region remains responsive, collaborative, and rooted in dignity."
Mission alignment
Kantrow says a perpetual challenge in palliative care is that it generally does not generate revenue, and so it can mistakenly be seen as a financial drain. But, he says, evidence is showing that palliative care has a positive impact on health care delivery and outcomes and therefore can bolster the services that providers deliver.
Dr. Chris Thomas, FMOL Health vice president and chief quality officer, backs this up. He says that having palliative care providers support patients and families through their suffering "has been critical in improving patient experience measures and length of stay. The expertise of palliative care allows our teams to treat diseases with acknowledgement of families in a manner that truly aligns with our mission."
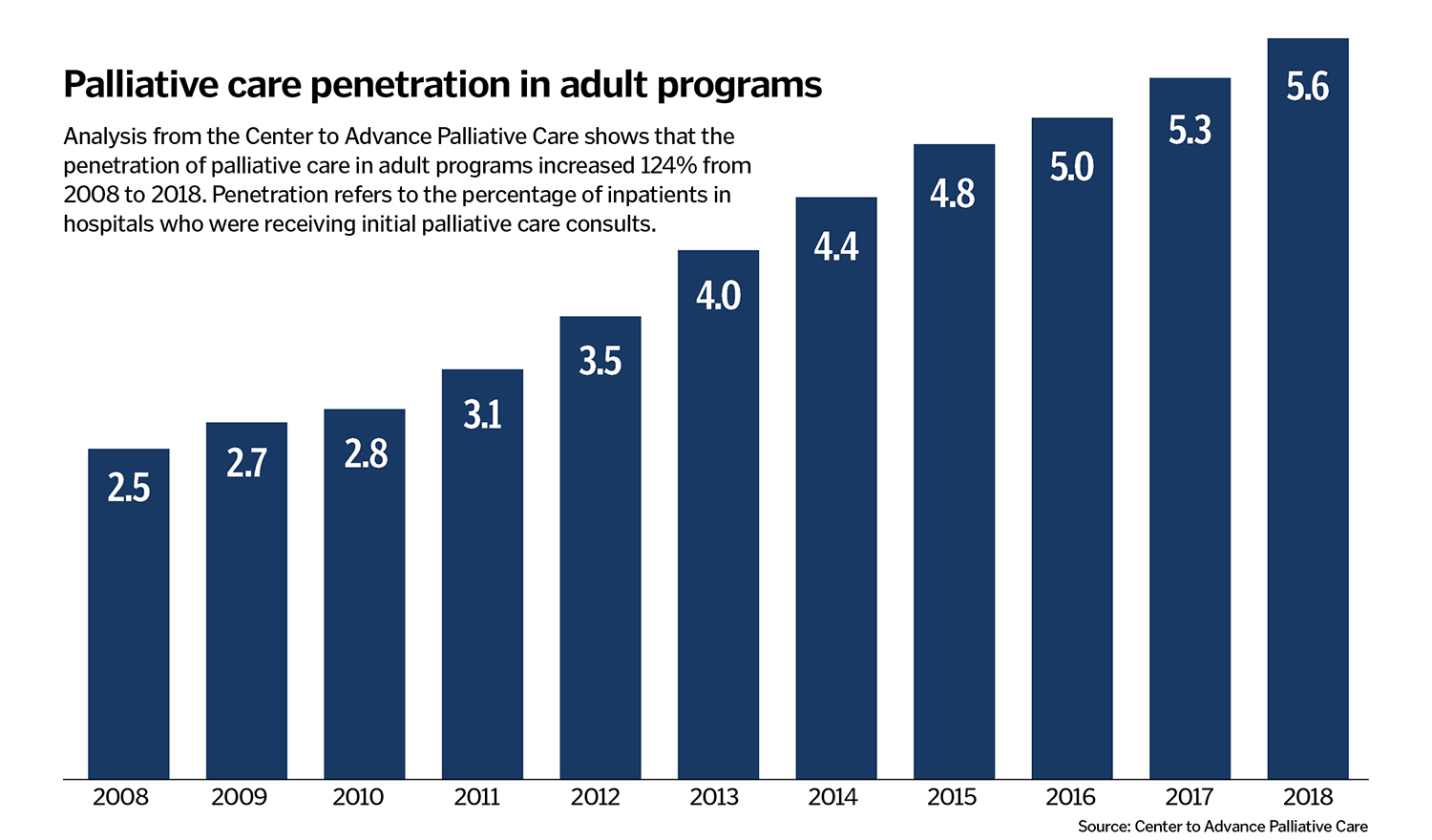
Thomas says that multiple metrics watched by health care leaders are moving in a positive direction because of the influence of palliative care. For example, studies suggest that when palliative care is involved early in the care of cancer patients, quality of life and even survival rates can be improved.
Dr. Mary Raven is a palliative care physician and chief of staff at Our Lady of the Lake. She credits Kantrow for building out FMOL Health's comprehensive palliative care program.
"He not only kick-started the program, but he has been the visionary who has allowed it to grow," Raven says. "It is because of him that we have full-fledged palliative care teams at all of our system's hospitals."
Kantrow deflects accolades, saying FMOL Health leaders and colleagues have been critical to the palliative care programming's success.
He says he is optimistic about how clinicians, other staff, patients, families and others are embracing palliative care at FMOL Health and beyond. He says with anticipated growth in health care needs as baby boomers age, having palliative care in place will be necessary to tend to everyone's needs.
He says, "I view palliative care as absolutely essential, like sheets on the hospital beds or air conditioning and heating. Having robust palliative care to ensure our most seriously ill patients get the very best care possible is an important part of how we will survive and flourish as a health system in the future."
