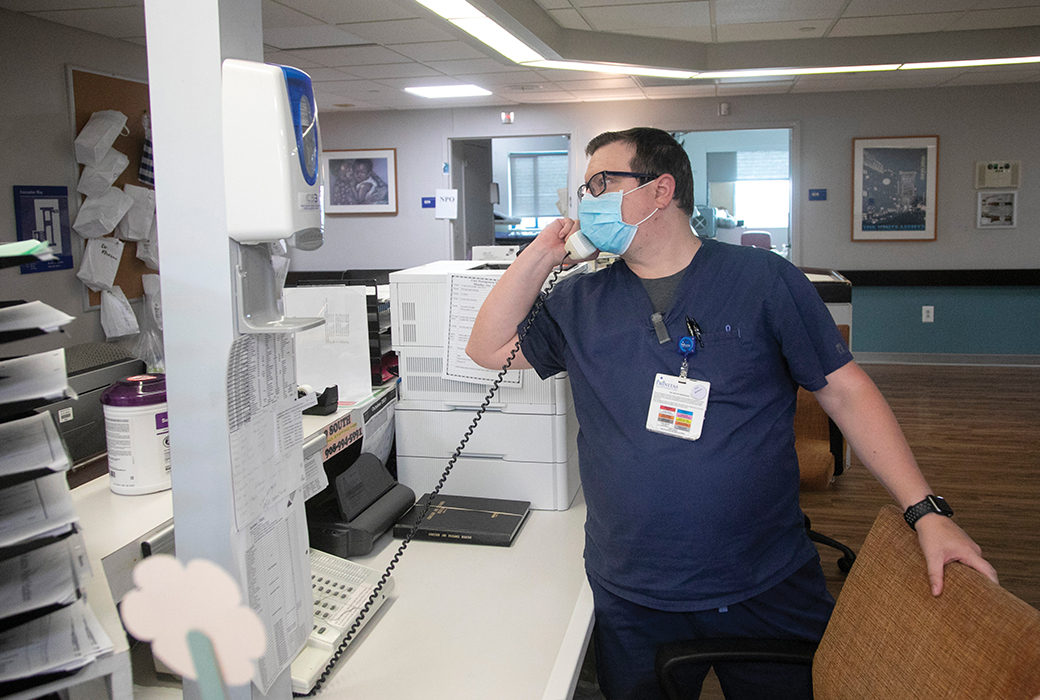
Photo by Aristide Economopoulos
"This Was the First Time, I Think in My Career, Where You Couldn't Go to a Playbook."
TIM CLYNE, DNP, RN
Nurse Manager of the COVID-19 Ward
I close my eyes and I can think of the first COVID-19 patient who came into our intensive care unit, intubated. At the time, March 2020, we knew nothing about COVID," recalls Tim Clyne, Trinitas Regional Medical Center nurse manager. "I remember vividly the nurse that took care of the patient. She said to me, 'You know, I'm not really scared about taking care of this patient, but I'm more scared about bringing this home to my family members.'"
From that first one, the number of patients increased exponentially. Clyne, who now manages the COVID ward, says, "One of the most challenging things in the beginning was: Where are we putting all of these sick patients? I'm still in awe about how all the different disciplines showed their expertise in their areas, not just physicians and nurses but our respiratory therapists, environmental services team and facilities engineers."
Keeping up with all the COVID-related studies as well as shifting protocols could be frustrating. "This was the first time, I think in my career, where you couldn't go to a playbook."
Clyne contracted COVID in the first wave of the pandemic. "I hate to say this but getting sick gave me a real understanding of how to truly treat patients, about the importance of symptom management and about providing exceptional nursing care." This included things like supporting them to get out of bed — when possible — for their health and helping them to eat properly.
"Before we had our first patient in the U.S., I actually sat with my wife, Sheryl, and we talked a lot about what would happen if this pandemic happened here, and how we would quarantine and manage our lives if I got sick. So there was some mental preparation before we even got to that point. The nursing profession sometimes thinks of the worst and hopes for the best."
Trinitas staff were working long hours, and as a manager trying to be available to care providers doing shift work, Clyne was tired. He thinks he was sick for a couple of weeks without knowing he was positive, because at the time it could take about a week to get test results. His first fever spiked on a Saturday morning and that following Monday, March 23, he had already taken the day off because it was his wedding anniversary. That day became his first day of quarantine. It wasn't easy to be at home in isolation and sick during such a critical time.
"I've never felt so sick in my life," he says, so depleted he sometimes crawled to the bathroom. He also kept his wife out of the room. "She didn't get sick, thankfully. After about four weeks I returned back to work and that was very difficult. My body was beaten up, I had lost about 30 pounds and I was just exhausted. When I look back, the day I returned we had the highest number of positive COVID patients ever in the hospital — about 200. However, it was very validating to go back and be able to carry out what I needed to do."
Caring for COVID patients brought a lot of uncertainty. It was hard to know how a COVID patient would progress, as the illness can lead to a very quick decline. "A seasoned nurse has some understanding of how to prioritize who needs the highest level of care," says Clyne. But with COVID patients, almost everyone needed the utmost care. "You do your best, use all the resources you have and delegate to others to help support these patients through some really tough times. You hope for the best and you pray sometimes. I'm a Catholic — I've always worked for Sisters of Charity organizations and sometimes the (end-of-life stage care you give) is just about using your spiritual side to deliver dignity before one passes away.
"I'm an oncology nurse and I've become very comfortable with palliative care and mortality in many ways, but it's different supporting somebody when their family members can't be at the bedside (due to wanting to limit disease spread) and you're doing it virtually. Having to tell family members they can't come in is tough.
"The advent of some new medications — like monoclonal antibodies — has led to improved patient outcomes," he says.
At times, he's pondered the question: Why am I doing this, nursing through this pandemic? "I think that at the end of the day, it's about giving to those who need care — and making it the best possible situation — during the worst possible time."
— Betsy Taylor