LISA MUSGRAVE, RN, BSN, MHA
Ascension Senior Vice President of Post-Acute and At-Home Services
 Illustration by Alice Mollon
Illustration by Alice MollonIf you have chronic health care needs, perhaps due to diabetes or high blood pressure, you may often find yourself frustrated by the incredibly complex health care system. You may be a working member of the "sandwich generation," caring for both children
at home and elderly parents with increasing health care needs of their own. Managing the health care services needed by you and your loved ones likely includes visits to multiple locations, often telling your stories repeatedly. Your goal: get the
care you need and get home.
At times, navigating health care may feel like a full-time job: trying to get appointments, selecting the right providers, arranging transportation, communicating between providers, and getting answers to your questions. What if the health care you need
could just come to you?
As part of Ascension's strategic planning process, health system leaders noted several swings supporting a shift to care in the home. Some of the key factors include:
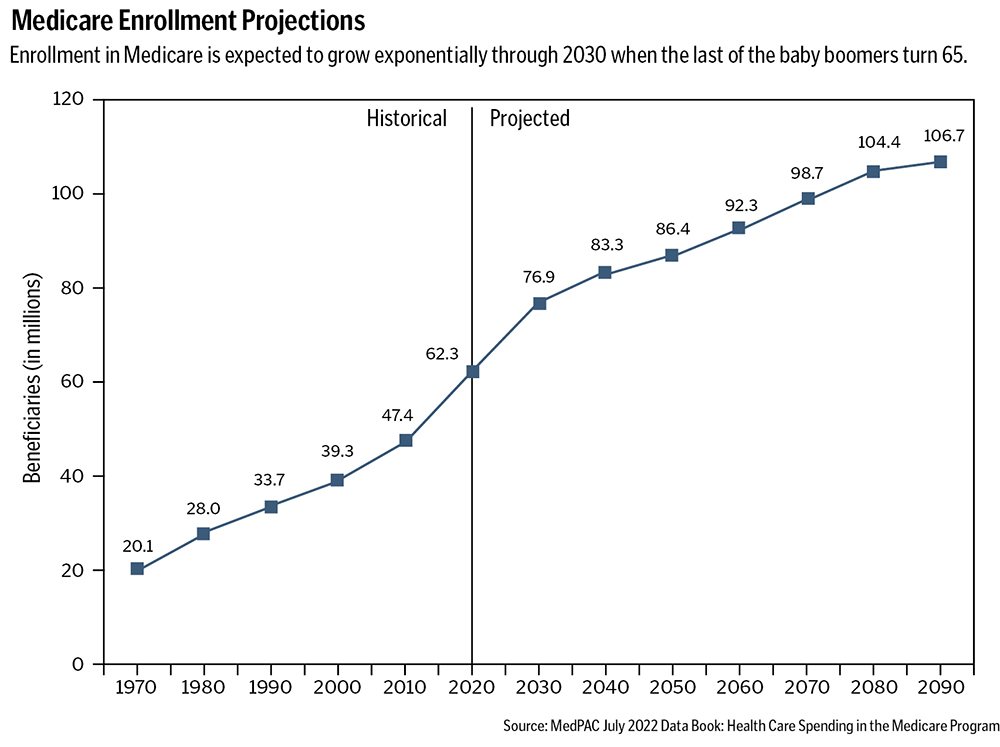
- More than 10,000 people are becoming eligible for Medicare every day, and by 2030, every baby boomer will be 65 or older.1, 2
- More than half of Americans have one or more chronic condition.3
- A growing number of people expressed in a recent national survey the desire to "age in place" or live in their own homes independently for as long as possible.4
- There is an increasing desire for more affordable concierge-style medicine, specifically care in the home.5
In response to these increasing factors and shifting demands, Ascension Post-Acute recognized a need to simplify the path to care by bringing multiple levels of it to the patient where they live, providing a satisfying alternative to multifacility care
through one integrated program.
TRANSITION TO HOME-BASED CARE
When the COVID-19 pandemic emerged, the mandate to safely increase access to care in the home became even more clear. People expressed a desire to avoid facility-based care when possible, preferring
the convenience of receiving care in their own home. New technologies, programs and capabilities for providing care in the home were initially shown to be cost-effective and the quality greater than or equal to facility-based care.6 For
example, remote patient monitoring, once a helpful tool but intermittent and cumbersome, can now be enhanced through algorithms and analytics that support clinical insights and facilitate early intervention by medical providers. This option became
a lifeline for sending patients home for care during the pandemic when hospital capacity was limited. COVID-positive patients could be discharged home from the emergency room by arranging for remote monitoring of their oxygen status and other vital
signs. Providers were alerted to any significant changes early enough for prompt intervention without requiring hospitalization, reserving beds for the sickest patients.
Virtual care is another area that catapulted forward during the pandemic. Virtual care — or telemedicine — services can be leveraged in the home to provide primary and specialty care, home health, and outpatient mental and behavioral health
visits. Other models that emerged or expanded rapidly during the pandemic included home dialysis, skilled nursing facility care at home, urgent/emergent care at home and hospital at home. Hospital-at-home programs that have been in existence in England,
Australia, Israel and Canada for years have had limited growth in the U.S., mostly due to limited reimbursement, but they grew significantly during the pandemic because of facility capacity constraints and a waiver from the Centers for Medicare and
Medicaid Services providing a path to Medicare reimbursement.7
In a desire to meet the evolving demand, Ascension Post-Acute, while always committed to ensuring that patients receive care in the most appropriate setting, made an at-home strategy one of its top imperatives. Ascension became a founding member of Moving
Health Home, an alliance of stakeholders working together to advance home-based care policy at the state and federal level to enable the home to be a more prominent clinical site of care.8 Ascension believes we can shift up to a quarter
of the care that in the past was provided in traditional health care facilities to the home setting, creating value for consumers, payers and providers alike.
CONSUMER BENEFIT
The American Journal of Accountable Care finds that at-home care models increased patient satisfaction, improved functional recovery, improved outcomes, decreased admissions and readmissions, reduced preventable
adverse health events and lowered family member stress.9 As noted earlier, a national consumer survey — released in 2021 by Moving Health Home and conducted by Morning Consult — clearly illustrated a desire for and comfort with
receiving care in the home: 88% of adults were satisfied with the clinical care services they received in the home, and 85% of people who had an experience with care in the home responded that they would recommend it to family and friends.10 For the consumer, being home means remaining in their familiar space with their family and pets, eating food they like, and sleeping better without noise and disruption. It also promotes trust and communication as services are delivered on the patient's
home turf where they have more control.
Through at-home care, health care professionals get an intimate look at the day-to-day lives of people they are caring for: meeting their pets, grandchildren and neighbors; seeing all the things that bring joy into someone's life; and most importantly,
seeing their priorities. Seeing people at home also gives glimpses into real risks: pills that have been dropped on the floor and remain unseen and untaken, or never picked up from the pharmacy at all; a home full of handwoven rugs just waiting to
be tripped on; and the day-to-day stressors that impact health, including limited food, unpaid bills, strained relationships with friends and family, and even loneliness. While the health system may not be able to solve all those issues, providing
health care in the home allows us to really emphasize the "care" piece of what we do and to address some of these social determinants of health that we may not ever become aware of until we have a glimpse into the home setting.
AT-HOME CARE BENEFITS
Payer Benefits
Payers, including commercial payers, Medicare Advantage and traditional Medicare, may see significant benefits from a shift to at-home care. The lower-cost setting may also reduce facility-associated infections
and adverse health events, promote patient compliance, increase coding accuracy and improve overall member satisfaction.11 Some payers may hesitate to provide coverage, concerned that demand for services will increase with the convenience
of care, but just recently, as 2022 ended, a very good sign in the battle for expanded care in the home occurred. The House and Senate passed the Hospital Inpatient Services Modernization Act, which extended the Acute Hospital Care at Home waiver
under Medicare for two more years, signaling their support for high-acuity home-based care models.12
Health System Benefits
For health systems, a shift toward care in the home allows them to free up capacity in their facilities that may be constrained for beds or, more likely, staff, and move lower-acuity care to the home. As well,
systems may be able to approach payers under value-based arrangements using care navigation to guide patients to the right level of care and using higher-acuity, lower-cost care at home as appropriate. Systems like Ascension, with a full continuum
of services available, are optimally positioned to deliver new models of care in the home through high-quality preferred provider networks in conjunction with at-home assets like Ascension At Home's health and infusion services, remote monitoring
through Current Health's Care-at-Home platform and Ascension At Home's advisory services.
Staff/Provider Benefits
Moving care to the home may be one solution to health care provider burnout. The one-to-one provider-to-patient ratio when working in the home provides time to assess, teach and care-manage. This can be highly
satisfying to staff who were considering leaving health care or needing a change. In-home care providers must be highly skilled, highly independent and highly resourceful. In a sense, they are moving into more of the ministry's work in communities
when they leave the facility and go into people's homes. Some patients live in comfort with many resources and others alone in poverty. Comprehending the home environment can help health care professionals better understand their patients and their
health. For example, they may have insight into why a patient with heart failure living on canned foods from a food pantry is unable to stay out of the emergency room for more than a few weeks at a time, and how to help them adapt to improve their
health status simply by giving their canned food a rinse before cooking. It is highly rewarding work.
OUR AT-HOME STRATEGY
Ascension is planning to bring a variety of home services to our patients. The vision for these future services includes a network of options to best suit each person's needs. For someone relatively healthy,
but experiencing an illness, this could be an urgent care visit in their home. For a person with a chronic condition, like heart failure, it may start with an urgent care visit in the home, but it may include a continuing path of care. This may involve
a hospital stay at home with IV medications and advanced imaging of their heart, followed by a transition to skilled nursing facility care at home with therapy to help the person regain strength and nursing to help with medication management. Then,
finally, the path culminates with a care management program that involves remote patient monitoring and virtual nursing support to avoid future returns to the hospital and ensure the person is living a life that includes the things that matter most
to them.
Components of these care choices exist in many systems, but they often stand alone and siloed. Our team seeks to build new offerings in the home and harmonize the experience across our diverse portfolio of services, solving the most frustrating friction
points by leveraging nonhealth care best practices and bringing more services directly to the consumer. For example, in February 2023, Ascension At Home, in partnership with Compassus, launched SNF (Skilled Nursing Facility) at Home in Austin, Texas.
This integrated program offers a combination of home health rehab, skilled nursing and personal care, and as-needed remote monitoring, meal/nutritional support, durable medical equipment and medications.
Anyone who has had to navigate themselves or their loved one through the health care system knows it can be a difficult task, filled with unknown terminology and high emotions, often at a time when you or your loved one isn't feeling their best. We are
leveraging our Ascension digital offerings to connect people to health care professionals who will provide customized care planning and review at-home service availability, simplifying the next steps and providing seamless navigation through options.
In the future, we plan to increase and add new technology to match in-home care programs available to meet patient goals and support them with caregiver communication and scheduling services.
COVID fundamentally shifted the health system's vision for both the type and acuity of care that can be provided in the home, and many in the health care industry are recognizing this transition. Ascension is committed to creating a continuum of care-at-home
programs through which our communities can benefit from high-quality, accessible care. The aging population, the increasing number of chronic conditions, the desire to age in place and increased consumer focus are all pointing us to the home. We look
forward to partnering with our patients to help them reach their health goals. There's no better place than home to do it.
LISA MUSGRAVE is Ascension's senior vice president of Post-Acute and At-Home Services, and provides senior management to: Ascension Living, a senior living organization; Ascension At Home, a home health division managed in partnership
with Compassus; Program of All-Inclusive Care for the Elderly (PACE) services; and Ascension's inpatient rehabilitation.
NOTES
- "Aging," U.S. Department of Health & Human Services, April 27, 2022, https://www.hhs.gov/aging/index.html.
- Andrew Meola, "The Aging U.S. Population is Creating Many Problems — Especially Regarding Elderly Healthcare Issues," Insider Intelligence, January 1, 2023, https://www.insiderintelligence.com/insights/aging-population-healthcare/.
- "About Chronic Diseases," Centers for Disease Control and Prevention, July 21, 2022, https://www.cdc.gov/chronicdisease/about/.
- "Americans Want Home to Be at the Center of Their Health," Moving Health Home, December 2, 2021, https://movinghealthhome.org/national-survey/.
- "United States Concierge Medicine Markets Report 2021-2028: Entry of Concierge Medicine Specialists Driving Growth," Cision PR Newswire, February 2, 2022, https://www.prnewswire.com/news-releases/united-states-concierge-medicine-markets-report-2021-2028-entry-of-concierge-medicine-specialists-driving-growth-301473633.html.
- Christine Ritchie and Bruce Leff, "Home-Based Care Reimagined: A Full-Fledged Health Care Delivery Ecosystem Without Walls," Health Affairs 41, no. 5 (May 2022): 689–695, https://doi.org/10.1377/hlthaff.2021.01011.
- "CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge," Centers for Medicare & Medicaid Services, November 25, 2020, https://www.cms.gov/newsroom/press-releases/cms-announces-comprehensive-strategy-enhance-hospital-capacity-amid-covid-19-surge.
- Moving Health Home, https://movinghealthhome.org/.
- James Howard et al., "Improved Cost and Utilization among Medicare Beneficiaries Dispositioned from the ED to Receive Home Health Care Compared with Inpatient Hospitalization," The American Journal of Accountable Care 7, no. 1 (March 2019):
10-16.
- "Americans Want Home to Be at the Center," Moving Health Home.
- Howard et al., "Improved Cost and Utilization"; "Pamela M. Saenger et al., "Cost of Home Hospitalization Versus Inpatient Hospitalization Inclusive of a 30-Day Post-Acute Period," Journal of the American Geriatrics Society 70, no. 5 (May
2022): 1374-83, https://doi.org/10.1111/jgs.17706; Kevin D. Frick et al., "Substitutive Hospital at Home for Older Persons: Effects on Costs," American Journal of Managed Care 15,
no. 1 (January 2009): 49-56.
- Anuja Vaidya, "Spending Bill to Extend Telehealth, Hospital-at-Home Waivers for 2 Years," mHealthIntelligence, December 20, 2022, https://mhealthintelligence.com/news/spending-bill-to-extend-telehealth-hospital-at-home-waivers-by-2-years.
QUESTIONS FOR DISCUSSIONThe work of Ascension and partners to increase health-at-home programs provides a number of ways people can receive care outside of hospital, clinic or doctor office settings. 1. What is your health care ministry doing to increase care in home settings? The evolving approaches will require an increased use of technology and one-to-one relationships in personal settings. What sort of workplace, personal and ethical
issues might arise for care providers and those they serve? Does your ministry have systems in place to consider and address these changes? 2. Increased health at home is viewed as important at a time when more than half of those in the U.S. have one or more chronic conditions. What are some of the most cost-effective, patient-centered and value-driven ways to respond to or
reduce chronic conditions? What changes in a person's environment might make the biggest difference overall? How do you encourage those changes? 3. The article's author Lisa Musgrave, Ascension's senior vice president of Post-Acute and At-Home Services, notes that hospital-at-home programs have existed for years in countries like England, Australia, Israel and Canada. Do you read
or talk to colleagues internationally to learn from them? What mechanisms might exist in your workplace to assist with this? |