BY: DAVID LICHTER, DMin
As the health care environment in the United States continues to evolve, so does the profession of chaplaincy. In Catholic health care particularly, the men and women who serve in the spiritual care ministry have seen the makeup of their ranks and responsibilities change dramatically during the past 20 years.
In 1997, Catholic health care's spiritual or pastoral care workforce was composed of nearly 79 percent Catholic chaplains who were religious women, priests and some local clergy, according to studies conducted by the Catholic Health Association and the National Association of Catholic Chaplains.
By 2007, that percentage had dropped to 59 percent Catholic, with a growing interfaith presence. Most likely the 2018 numbers will show closer to 35 percent Catholic and an even more varied faith representation among chaplains, which allows for a rich diversity that is important for serving people of all faiths and no faith.
However, the decline in qualified, board-certified Catholic chaplains is felt by Catholic systems across the country as they seek to fill chaplain positions or look for qualified Catholic spiritual care professionals to assume director and manager roles. Since 1997, the NACC has recorded the decrease of chaplaincy board-certified religious women from more than 1,700 to 400, priests from more than 630 to 360, and a modest and insufficient increase — from 980 to 1,150 — of Catholic laypeople serving as chaplains, most of whom are board certified.
Sufficient staffing for spiritual care services is likely to remain a major challenge for Catholic health care until there is a greater awareness and promotion of professional chaplaincy as a lay vocation.
The profile of a hospital's spiritual care department is very diverse. Along with board-certified chaplains and those who have met minimum requirements but have yet to complete board certification, noncertified chaplain associates and an occasional representative of a specific religion will fill out the team. Some pastoral care departments have piloted the use of trained volunteers for initial spiritual care visits or limited spiritual screening. Their roles, on the whole, are carefully limited, and the volunteers work under the supervision of board-certified chaplains, not as a replacement for them.
IDENTITY
The chaplain often has been perceived as a representative of a specific faith denomination who works in a specific hospital or hospital unit, generally on his or her own, and devotes time to paying initial visits to patients. A chaplain was expected to offer a listening presence with no agenda, praying with someone as needed, being a keeper of the ministry and a pastor to the staff.
Over the years, the chaplain's identity has made a significant evolutionary shift. He or she now needs to be working at the touch point of service, whether it is in an acute, outpatient or virtual setting. Julie M. Jones, executive director, mission and ministry at Mercy, St. Louis, and other spiritual care leaders at Mercy, categorized the evolution of chaplaincy as changes in identity, focus and priorities.
Although chaplains in Catholic health care recognize their service to be part of Christ's healing mission, they more readily understand that service as tending to the spiritual and emotional needs of patients, families and staff of all faiths or of no faith. Thus, the chaplain — who may be of any personal faith background — is a spiritual care specialist within the interdisciplinary care team and an integral part of mission integration.
As a specialist, the chaplain is an educator/facilitator/coach who aids other staff members in identifying and screening for spiritual and emotional needs that either the staff member can attend to or that require a more in-depth spiritual care assessment. If such assessment is necessary, the chaplain conducts it, develops appropriate goals of spiritual care and communicates them to the rest of the interdisciplinary team.
The chaplain provides a ministry for patients, families and staff that includes rituals to facilitate profound moments of meaning. The chaplain also partners with local clergy, congregations and religious organizations to meet spiritual or religious needs in that area.1
FOCUS AND PRIORITIES
The chaplain's focus has had to expand from primarily a one-on-one setting in response to immediate needs, including trauma, dying and bereavement, to building relationships with other professionals — such as mission leaders, physicians, nurses, social workers, religious and other community leaders. Chaplains now contribute to the interdisciplinary team's healing outcomes, the health system's strategic priorities and the community's health and wellness outcomes.
Professional chaplaincy priorities thus have moved from mainly trying to see every patient and respond to every crisis, code, trauma and death within a facility. Now the chaplain must reorganize and regularly triage the workload in consideration of department priorities, referral systems, consults and the diverse modes of service delivery (face-to-face, phone, eChaplaincy, video conferencing, etc.). In short, the spiritual care department's goals now align with the health care system's strategic priorities.
CRITICAL SUCCESS FACTORS
Over recent years, the critical success factors for effective spiritual care are ones all Catholic systems are working on together. The more our collaborative efforts lead us to learn from one another and grow, the higher the quality of spiritual care we can offer to our patients and families, staff and leaders.
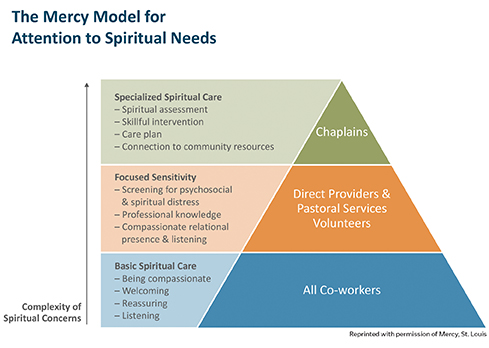
The first critical step is to consider how the system visualizes and conveys the focus of its core spiritual care services. This model developed by St. Louis-based Mercy, is an example. Conveyed in a simple graphic (see page 68), it helps all employees visualize their role in the system's commitment to spiritual care while highlighting chaplains' specialized spiritual care work.2
Name the benefits and make a business case for them. Although spiritual care is essential to Catholic health care, the more effectively we describe the benefits of our services for patients, families and staff, the more likely health care leaders will make decisions to integrate spiritual care.
For instance, we can offer evidence-based research that shows patients whose spiritual needs are addressed as they approach the end of life spend less time in ICU and experience higher satisfaction with their care, and their families also are more satisfied. When chaplains help with patient-clinician communication, it can lead to patients better managing their own care, which in turn contributes to lower emergency and aggressive care costs.
Also, see the suggestions from the CHA Pastoral Care Advisory Committee and NACC for how to describe what chaplains do and the resulting benefits.3
Establish evidence-based efficacy: Much research on the evidence-based outcomes of spiritual care and professional chaplaincy is currently being done on the national and international levels. The professional chaplaincy associations created the impetus and backing for the Transforming Chaplaincy and Joint Research Council.
George Fitchett, DMin, PhD, at Rush University Medical Center in Chicago, has summarized significant research in the field (see The Evidence-Based Spiritual Care Paradigm) and highlights studies on the importance of spiritual care to patients and families and the impact of spiritual care on patient satisfaction, the patient experience and patient outcomes.4 Every health care system can partner with its spiritual care department to develop interdisciplinary research projects to study chaplain interventions. (see Measuring Pastoral Care Performance)
Strengthen the system of referrals to the spiritual care specialist: This is challenging, because health care systems have not standardized screening questions or training for clinicians to help them diagnose patients' spiritual distress or recognize complex emotional/spiritual issues that need to be referred to a spiritual care specialist.
Describe patients' spiritual needs in medical records: Chaplains are key communicators to other members of the interdisciplinary team about the patient's spiritual and emotional needs. Charting in the medical records a clinically clear and understandable picture of who the patient is, what he or she is feeling and values, how important or not are the person's spiritual or religious resources, and how all these might affect the goals of care is critical for the clinical team's deliberations on the patient's treatment plans.5
 Diversify the delivery system: Currently several systems, such as Ascension Health, Mercy in St. Louis and Mercy Health Cincinnati, are dedicating personnel to determining how best to embed spiritual care in outpatient and clinic settings through diverse delivery methods, such as eChaplaincy, on-call, phone consults and video conferencing. Many systems have invested in pilot projects in this area to improve the effective use of their spiritual care personnel.
Diversify the delivery system: Currently several systems, such as Ascension Health, Mercy in St. Louis and Mercy Health Cincinnati, are dedicating personnel to determining how best to embed spiritual care in outpatient and clinic settings through diverse delivery methods, such as eChaplaincy, on-call, phone consults and video conferencing. Many systems have invested in pilot projects in this area to improve the effective use of their spiritual care personnel.
Develop and implement system-level standards for spiritual care: An important step to strengthening spiritual care is developing and implementing system-wide standards. The benefits include providing clarity on the role, purpose, direction and content of the spiritual care services within the system, as well how it structures its spiritual care services and personnel. Several systems, such as Providence St. Joseph, Trinity and Bon Secours, have developed and continue to refine their standards.6
Commitment to chaplain preparation, credentialing and compensation: A chaplain's board certification entails extensive education and preparation.7 Some Catholic systems have made strides to improve the classification of a master's level, clinically trained and board-certified service provider; others still need to complete this work.
CONCLUSION
Spiritual care is an essential and integral service at the heart of Catholic health care. Part Two of the Ethical and Religious Directives for Catholic Health Care Services states, "The medical expertise offered through Catholic health care is combined with other forms of care to promote health and relieve human suffering.
For this reason, Catholic health care extends to the spiritual nature of the person… Directed to spiritual needs that are often appreciated more deeply during times of illness, pastoral care is an integral part of Catholic health care."8
Catholic health care's commitment to pastoral and spiritual care further emphasizes the integrity or wholeness of the human person as care that "embraces the physical, psychological, social and spiritual dimensions of the person." Our commitment to pastoral care keeps before us our mission to view and treat patients and families with dignity and recipients of our compassionate care, and not as market share, objects for study or a disease to cure.
DAVID LICHTER is executive director of the National Association of Catholic Chaplains in Milwaukee, Wisconsin.
NOTES
- Brian P. Smith, "Spiritual Care in the Midst of Health Care Reform," Health Progress, 95, no. 5 (September-October 2014): 52. www.chausa.org/publications/health-progress/article/september-october-2014/spiritual-care-in-the-midst-of-health-care-reform.
- Chart reproduced courtesy of Mercy, St. Louis.
- See this example of the importance of making the case: www.handzoconsulting.com/spiritual-care/.
- George Fitchett, "Recent Progress in Chaplaincy Research," Journal of Pastoral Care & Counseling 71, no. 3 (2017): 163-75. http://journals.sagepub.com/doi/abs/10.1177/1542305017724811.
- See this very helpful book addressing charting: Gordon J. Hilsman, Spiritual Care in Common Terms: How Chaplains Can Effectively Describe the Spiritual Needs of Patients in Medical Records (London and Philadelphia: Jessica Kingley Publishers, 2017).
- For more information about the guidelines and system standards, see www.nacc.org/resources/administrator-resources/. Also, see Trinity Health's Standards of Excellence in Spiritual Care, www.trinity-health.org/documents/SpiritualCareStandards.pdf.
- Board of Chaplaincy Certification, "Common Qualifications and Competencies for Professional Chaplains." www.professionalchaplains.org/files/2017%20Common%20Qualifications%20and%20Competencies%20for%20Professional%20Chaplains.pdf.
- United States Conference of Catholic Bishops, Ethical and Religious Directives for Catholic Health Care Services, 5th ed., (Washington, D.C.: USCCB, 2009). www.usccb.org/issues-and-action/human-life-and-dignity/health-care/upload/Ethical-Religious-Directives-Catholic-Health-Care-Services-fifth-edition-2009.pdf.
_______________
THE GROWTH OF COLLABORATIONS TO ADDRESS SPIRITUAL CARE CHALLENGES WITHIN CATHOLIC HEALTH CAREIn October of 2007, the Catholic Health Association and the National Association of Catholic Chaplains co-sponsored a pastoral care summit in Omaha, Nebraska, to establish a vision for spiritual care, along with benchmarks and metrics to measure the effectiveness of spiritual care programs within the Catholic health ministry. The three-day meeting resulted in a vibrant network and a common commitment to address collaboratively challenges all systems faced. In early 2008, CHA and NACC conducted a survey among Catholic health systems on the state of pastoral care, as a follow-up to a similar 1998 study, and a third follow-up study is scheduled for 2018 in order to update the data and highlight long-term trends. CHA formalized the collaboration when it established the Pastoral Care Advisory Committee with representatives from the diverse Catholic systems. Among other offerings, the committee has created guidelines for system-level spiritual care standards; materials for promoting spiritual care and addressing executive concerns; resources for staff care; resources including an e-learning module; approaches to justifying value; determining appropriate staffing levels; and defining core services of chaplains and ways of examining the quality of spiritual care services. In 2013-2014, the pastoral care committee conducted a study of Catholic health care executives' and clinicians' perspectives on spiritual care and chaplains.1 Professional Chaplaincy Associations
The major professional chaplaincy associations represent more than 10,000 chaplains, spiritual care educators and pastoral counselors in the United States, Canada and some international communities. In 2004, they developed and committed to a common set of ethical standards for professional chaplains and common qualifications and competencies for certification of professional chaplains.2 After convening in 2009 for a spiritual care summit, 1,800 members of these associations strengthened their common commitment to improving chaplain practice outcomes and effectiveness of their certification processes through research. They are partners in founding and supporting the think tank Transforming Chaplaincy, which promotes research literacy among chaplains, and an international partnership for evidence-based research through the Joint Research Council.3 The collaboration among these strategic partners in spiritual care is vital to maintaining the highest level of professional preparation, credentialing and advancement of the profession of chaplaincy. Most Catholic health systems require that their chaplains receive their Clinical Pastoral Education training through accredited centers and that their board-certified chaplains be certified by one of these strategic partners. The strategic partnership among these professional chaplaincy associations continues to be strong, with future plans for common professional development offerings, professional ethics oversight and procedures, and ongoing advocacy for the profession. NOTES - David Lichter, "Chaplaincy Surveys Offer Key Insights," Health Progress 95, no. 5 (September-October 2014): 57-59.
- ACPE, www.acpe.edu; Association of Professional Chaplains, www.professionalchaplains.org; Canadian Association for Spiritual Care, www.casc.org; National Association of Catholic Chaplains, www.nacc.org; Neshama: Association of Jewish Chaplains, www.najc.org. The American Association of Pastoral Counselors, www.aapc.org, was also an early partner in the common professional ethics and certification documents but did not continue after 2011.
- For more information about the think tank Transforming Chaplaincy, see www.transformchaplaincy.org, and for more information about The Joint Research Council, see www.transformchaplaincy.org/about/partner-organizations/.
|