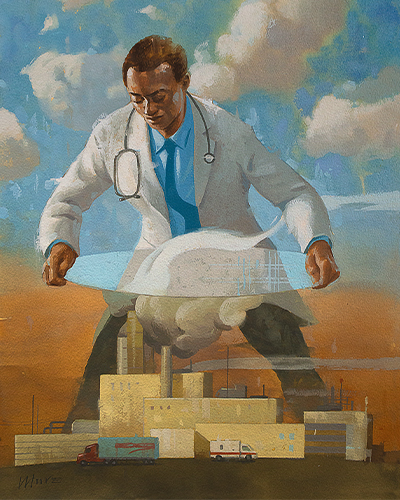
Illustration by Larry Moore
SARA SHIPLEY HILES
Contributor to Health Progress
The first rule of medicine is "do no harm." Yet the health care industry itself is a major source of pollution, accounting for about 8.5% of U.S. greenhouse gas emissions in the United States and a similar share of major air pollutants.1 If the American health care industry were a country, it would rank ahead of the entire United Kingdom in emissions — and the numbers keep rising.
Dr. Jodi Sherman, an anesthesiologist at Yale University and a leader in researching the environmental footprint of the health care sector, co-authored a study in 20162 finding pollution from health care causes as much death and disability as preventable medical errors, first documented in a landmark Institute of Medicine report two decades ago.3
Just as that report sparked a revolution in patient safety practices, attention is needed now to cut health care's pollution burden, said Sherman, who also serves as medical director of sustainability for Yale New Haven Health. "There's very little accountability as to how we use resources as providers. We've known for a very long time that our expenditures are out of control, but that information is not motivating behavior change," she said. Understanding that there is actual harm caused by the care provided, "that is new information; that is the game changer."
LESS IS MORE
Climate change and the COVID-19 pandemic are driving awareness of the urgent need for the health care industry to behave more sustainably — and change is happening rapidly, if unevenly. The 2020 report of the Lancet Countdown, an international collaboration tracking health and climate change, presented its "most worrying outlook" ever, citing concerns about increased heat waves, floods, droughts, wildfires, storms, disease outbreaks, crop failures, food insecurity and rising sea levels.4 Climate change and COVID both disproportionately affect vulnerable populations, the report said, and they require global, aligned responses. Now the health care sector is starting to take action on emissions. "Just as it did with advancements in sanitation and hygiene and with tobacco control, growing and sustained engagement from the health profession during the past five years is now beginning to fill a crucial gap in the global response to climate change," the report said.
In the thick of the pandemic, England's National Health Service last year announced its goal to become the first national health system in the world to achieve carbon net-zero, or adding no more emissions than are removed through offsets such as tree planting.5 Nick Watts, NHS's new chief sustainability officer, said at Yale University's recent "Care Without Carbon" symposium that the health care service can't fulfill its mission to provide "high quality care for all, now and for future generations" without responding to climate change. "We know that we can't deliver health care without that," he said.6
The NHS committed to being carbon neutral in its own operations by 2040 and to driving the same reduction among its suppliers by 2045. "Within the decade," Watts said at the symposium, "the NHS will no longer purchase from anyone that does not meet or exceed our commitments on net-zero."
In the United States, about 1,200 hospitals are members of Practice Greenhealth, a membership organization supporting sustainability solutions.7 Catholic hospitals and health care systems are some of the leaders in this space, said Jessica Wolff, U.S. director of climate and health for Health Care Without Harm and Practice Greenhealth. "They are so mission-driven and values-driven, that's why they care about this," Wolff said. "It's in their mission to treat the poor and the vulnerable, to care for God's creation." Providence, Ascension and CommonSpirit Health are all members of the U.S. Health Care Climate Council, a leadership group advocating for climate action.8
Providence also announced its ambitious climate goal in the middle of the pandemic: to become carbon negative by 2030 across its en–tire operation, including its supply chain. Beth Schenk, executive director of environmental stewardship, called it the boldest commitment in U.S. health care. In the past year, its hospitals have cut waste to landfills, installed low-flow sinks and solar panels and composted food waste. "Environmental pollution and climate pollution impact the poor and vulnerable more than those who are better protected. It all comes back to a commitment to justice," she said. Providence's "WE ACT" plan focuses on five areas responsible for the majority of its carbon footprint: waste, energy/water, agriculture/food, chemicals and transportation.9
CommonSpirit Health's sustainability plans call for reducing energy and water consumption by 25% and reducing greenhouse gas emissions by 40% by 2030. Already the organization has undertaken efforts, including upgrading lighting and HVAC equipment, planting trees, developing an environmentally-friendly clothing formulary and redesigning patient menus to be plant-based.10 Sr. Mary Ellen Leciejewski, OP, system vice president of environmental sustainability, has been leading green efforts for three decades. "Years ago, it was like pushing the rock uphill," she said. Now, "I think the rock is rolling. The difference I've seen is, there are so many colleagues who come up to me and say, 'This is about the future of my kids and grandkids. What kind of planet will we have for them?'"
(Also in this issue of Health Progress, Ascension unveils its environmental and sustainability objectives and goals in a three-pillar plan, see "Advancing Health Equity Through Climate-Smart Changes: Health Care's Call to Action.")
Wolff pointed to Kaiser Permanente and Cleveland Clinic as other trendsetters in pollution reduction. Kaiser Permanente, for example, already has been certified as carbon neutral for its facilities and energy sources, and the company is working on its supply chain emissions.11
THE CHALLENGES
But not every hospital and health care system is on board. Only about 20% of U.S. hospitals are members of Practice Greenhealth, and a 2018 study found that only 12% of 49 large U.S. health care corporations published a sustainability report, compared with 82% of companies on the Standard & Poor's 500 index.12
Being green isn't always easy. Sherman said most sustainability programs start out focusing on visible waste, like recycling. "Unfortunately it is time-consuming to set up and maintain, and it turns out to be very low-impact" in terms of emissions, Sherman said. "But we didn't know that until we started doing the research."
Disposable masks and gowns are another bugaboo — but they're only the top of the trash heap. Watts of the NHS said that emissions from single-use personal protective equipment, or PPE, were not No. 1 or even No. 10 on his agency's list of concerns. "Do we need to do something with it? Yeah, we absolutely do," he said. "But it's important to get our priorities straight as we think about what a net-zero health care system actually means and actually requires."
Where, then, does pollution hide? The main sources are buildings, transportation and manufacturing of the many energy-intensive products used in hospitals and clinics. The supply chain — including the production, transport and disposal of drugs, food, devices and equipment — makes up 71% of all health care emissions globally, according to Health Care Without Harm.
Big problems require big solutions, and that means more than eliminating plastic straws in the cafeteria. Ultimately, health care organizations should be required to report emissions and draw them down in accordance with science-based targets and timelines, Sherman said. Accountability for environmental sustainability metrics could be enforced through the Centers for Medicare & Medicaid Services' performance improvement payments, she said.
GETTING TO NET ZERO
Health Care Without Harm's 2021 Global Road Map for Health Care Decarbonization report warns that under a "business as usual" scenario, health care's global emissions would more than triple by 2050. To prevent that, the organization highlighted seven high-impact actions to get to zero emissions by midcentury.13
Energy consumption is the driving factor, and solving that problem means replacing fossil fuels with 100% clean, renewable electricity, according to the report. Zero-emissions buildings and transportation are next, followed by sustainably grown food and low-carbon pharmaceuticals. A "circular economy" based on clean, reusable technology is a must. Last, the report suggests establishing greater efficiency and effectiveness by eliminating unnecessary procedures and tying carbon reduction to quality of care.
In the United States, about a third of health care resources go to low-value or wasteful care.14 "We spend more money than anywhere else in the world and our health outcomes are not at the top," Wolff said. It turns out that climate-smart health care is financially smart, too.
Sherman pointed out that sustainability isn't just about climate change — it's about cutting air, water and land pollution and responsibly using limited resources. "If we're overconsuming materials, we will run out," she said.
ENGAGING HOSPITALS AND PROVIDERS
U.S. health care facilities are trying many strategies to cut waste and lower emissions.
At HealthPartners, a nonprofit health care organization with eight hospitals in Minnesota and Wisconsin, sustainability measures have saved an average of $2.5 million annually since 2013, said Dana Slade, director of sustainability programs. Success stories include safer medication disposal, reducing paper use, embracing telemedicine and installing solar panels.15 The biggest savings have come through energy improvements such as installing LED lights and adding controls that can ramp heating and cooling up or down as needed. "Health care is an energy hog. We use energy 24/7/365," he said. "That's one of the first things to focus on."
In operating rooms — one of the most energy-intensive parts of a hospital — HealthPartners has installed devices called Neptunes that suck up surgical fluids and carry them to the sanitary sewer system. Historically, that material was collected in disposable canisters and treated as medical waste, an unnecessary expense. Another innovation is sending single-use devices such as surgical scalpels and drills for reprocessing.
When asked about lessons learned, Slade said that even small hospitals can be sustainable. "The other thing I'd like to emphasize is sustainability is more than just recycling or energy; it's engaging your community and your staff about the health and well-being of your community," he said.
At Providence Portland Medical Center in Oregon, anesthesiologist Dr. Brian Chesebro has helped to lead a national movement toward greener anesthetics. Chesebro had heard that some common anesthetics were potent greenhouse gases, and he soon learned that one was much worse than the others. Desflurane has 20 times the heat-trapping power of another gas, sevoflurane, and it stays in the atmosphere 14 times as long. Otherwise, the gases work about the same. A self-described data geek, Chesebro obtained detailed records at his hospital and showed his colleagues how they could reduce their own environmental footprints by choosing a different gas. Chesebro likes to compare using desflurane in surgery to driving a Hummer, whereas using sevoflurane is like driving a Prius. Sevoflurane is cheaper to boot.
Now Chesebro speaks to audiences all over the country, and Providence's Oregon hospitals have cut anesthesia emissions by 95%. "Physicians don't like to be told what to do, especially ones that have long-standing clinical habits," said Chesebro, who also serves as Providence's medical director of environmental stewardship in its Oregon region. "The switch is pretty easy, but people need to be led through the science."
At Dignity Health California Hospital Medical Center, a 318-bed, acute-care hospital located in downtown Los Angeles that is part of CommonSpirit Health, Facilities Coordinator Kim Ray has seen a lot of changes in her 14 years on the job. When she first started, there was, to put it charitably, "a lot of opportunity" to improve sustainability.
Today, the hospital has won multiple awards from Practice Greenhealth, including a "Greening the O.R." award, thanks to its switch to better anesthetic gases and use of reprocessed materials.16 The hospital recycles sterile "blue wrap" and uses compostable serviceware in the cafeteria, and it was the first on the West Coast to conduct an extreme heat drill. Ray is most proud of a partnership with community group Homeboy Industries to recycle electronic waste while providing jobs for formerly incarcerated people. "We are five blocks from Skid Row, the largest homeless population in the United States. We are a true safety-net hospital," Ray said. "I like to think if we can do it, anyone can."
SARA SHIPLEY HILES is a freelance journalist and an associate professor at the University of Missouri School of Journalism in Columbia. She is also the executive director of the Mississippi River Basin Ag & Water Desk, a collaborative reporting network.
NOTES
- Matthew J. Eckelman et al., "Health Care Pollution And Public Health Damage In The United States: An Update," Health Affairs 39, no. 12 (December 1, 2020): 2071-2079, https://doi.org/10.1377/hlthaff.2020.01247.
- Matthew J. Eckelman and Jodi Sherman, "Environmental Impacts of the U.S. Health Care System and Effects on Public Health," PLOS ONE, June 9, 2016, https://doi.org/10.1371/journal.pone.0157014.
- Linda T. Kohn, Janet M. Corrigan and Molla S. Donaldson, editors, To Err Is Human: Building a Safer Health System, (Washington, D.C.: National Academies Press, 2000), https://doi.org/10.17226/9728.
- Nick Watts et al., "The 2020 Report of the Lancet Countdown on Health and Climate Change: Responding to Converging Crises," Lancet 397, no 10269 (December 2, 2020): 129-170, https://doi.org/10.1016/S0140-6736(20)32290-X.
- "NHS Becomes the World's First National Health System to Commit to Become 'Carbon Net Zero', Backed by Clear Deliverables and Milestones," Greener NHS, October 1, 2020, https://www.england.nhs.uk/greenernhs/2020/10/nhs-becomes-the-worlds-first-national-health-system-to-commit-to-become-carbon-net-zero-backed-by-clear-deliverables-and-milestones/.
- "Care Without Carbon: The Road to Sustainability in US Health Care," Yale Center on Climate Change and Health, https://ysph.yale.edu/climate/phes/sustainability-health-care-symposium/.
- "Sustainability Solutions for Health Care," Practice Greenhealth, https://practicegreenhealth.org.
- "Health Care Climate Council," Health Care Without Harm, https://noharm-uscanada.org/healthcareclimatecouncil.
- "Learn How WE ACT to Become Carbon Negative by 2030," Providence, https://www.providence.org/about/community-partnerships/work-we-do/government-affairs-and-social-responsibility/environmental-stewardship/our-commitment-to-environmental-transformation.
- "Building Healthier Communities," CommonSpirit Health, https://commonspirit.org/a-healthier-future/building-healthier-communities/.
- "The First Carbon Neutral Health System in the U.S.," Kaiser Permanente, https://about.kaiserpermanente.org/community-health/news/first-carbon-neutral-health-system-in-us.
- Dr. Emily Senay and Dr. Philip J. Landrigan, "Assessment of Environmental Sustainability and Corporate Social Responsibility Reporting by Large Health Care Organizations," JAMA Network Open 1, no. 4 (2018), https://doi.org/10.1001/jamanetworkopen.2018.0975.
- "Global Road Map for Health Care Decarbonization: A Navigational Tool for Achieving Zero Emissions with Climate Resilience and Health Equity," Health Care Without Harm, April 16, 2021, https://healthcareclimateaction.org/roadmap.
- Donald M. Berwick and Andrew D. Hackbarth, "Eliminating Waste in US Health Care," JAMA 307, no. 14 (April 11, 2012): 1513-16, https://doi.org/10.1001/jama.2012.362.
- "Sustainability," HealthPartners, https://www.healthpartners.com/about/community/sustainability/.
- "California Hospital Medical Center Honored for Environmental Sustainability by Practice Greenhealth," Dignity Health, https://www.dignityhealth.org/socal/locations/californiahospital/about-us/press-center/california-hospital-medical-center-honored-for-environmental-sustainability-by-practice-greenhealth.
QUESTIONS FOR DISCUSSIONJournalist Sara Shipley Hiles writes that Health Care Without Harm's 2021 Global Road Map for Health Care Decarbonization reports that under a "business as usual" scenario, health care's global emissions would more than triple by 2050. But the organization's report says that the use of renewable energy; zero-emission buildings and transportation; sustainably grown food; and low-carbon pharmaceuticals will have a high impact. It also calls for reusable technology, the elimination of unnecessary procedures and tying carbon reduction to quality of care. - For leaders in Catholic health care: How is your health care system or facility doing with its work to reduce its environmental footprint? How does it report its efforts to employees and communities?
- Making environmental improvements isn't just about caring for the planet. We know the scale of health care nationally means that choices health care systems make when it comes to supply chain, energy sources, environmental waste and more ultimately impact the health of patients and their communities. At such a busy time in health care, is there a way to prioritize this work? To better support those directly engaged in it? How can you get buy-in and support from senior leadership and boards?
- Do you think Catholic health care has been a leader in sustainability and innovative approaches to protect the environment? What more could be done? Is there a mechanism to inform leadership at your facility if someone has an idea that can lead to environmental improvement?
- Can you articulate how this environmental stewardship work is directly related to the mission and values of Catholic health care?
|