Representatives of multiple health care facilities serving the safety net population in St. Louis say that working together through the St. Louis Integrated Health Network has helped them to coordinate specialty care effectively. And this in turn has enabled them to address the health care needs of marginalized people in a patient-centered way.

SSM Health is part of the network. Dr. Saida Kent, a hospitalist with SSM Health Saint Louis University Hospital, said the network is a great resource for directing her patients to the help they need.
She said most of her patients are uninsured or underinsured, and it's usual for her to talk extensively with them about the barriers they face to care and to point them to solutions.
"It's our role as physicians that — even though we can't solve all the issues — we need to acknowledge the issues patients have," Kent said. "I need to view my patients as a whole — not just as a body. It's important to know your patient and to, at a bare minimum, see the person in front of you."
Need for care coordination
The Integrated Health Network is the result of efforts by the St. Louis Regional Health Commission to better coordinate the care of vulnerable patients. The commission wanted the providers to collaborate to improve care access, enhance care quality, achieve cost efficiencies, and improve patient outcomes.
In November 2003, the commission launched the Integrated Health Network. The network has evolved over the years and now includes four federally qualified health centers, three hospital systems, two medical schools and two public health departments.

One of the Integrated Health Network's programs is the Care Transitions Initiative, which in turn has its own program called the Community Referral Coordinator Program. Through that initiative, 12 community referral coordinators work on-site at hospitals and two work in the community.
The hospital-based coordinators meet with acute care patients to help them navigate their movement between inpatient units, the emergency department and outpatient providers.
The coordinators focus on patient education and preventive care. They help patients find a primary care home, schedule appointments, and set up transportation and connections to social services. The Integrated Health Network's website says the coordinators have had more than 220,000 patient encounters in the hospitals and community since 2007.
The Integrated Health Network also offers programs to educate patients on the levels of care available to them, including primary care, urgent care, living well, specialty care and emergency care.
'A team sport'
A main reason the network is successful is that the safety net providers take a systems approach to improving care delivery, making sure that they function as a whole rather than as separate facilities, explained Aramide Ayorinde, CEO of the Family Care Health Centers, a federally qualified health center that is part of the network.

Karen Bradshaw, regional director of community health for SSM Health — St. Louis and Southern Illinois, said the organizations in the network all are represented on a board of directors and a task force. Between these groups, the network members meet regularly to talk about how to improve the way patients move through the system.
The network members connect through electronic health records, jointly develop community health needs assessments, partner on programming, and share resources including grant dollars in some cases.

"Health care is a team sport," said Dr. Melissa Tepe, vice president and chief medical officer of Affinia Healthcare, a St. Louis FQHC that is part of the network.
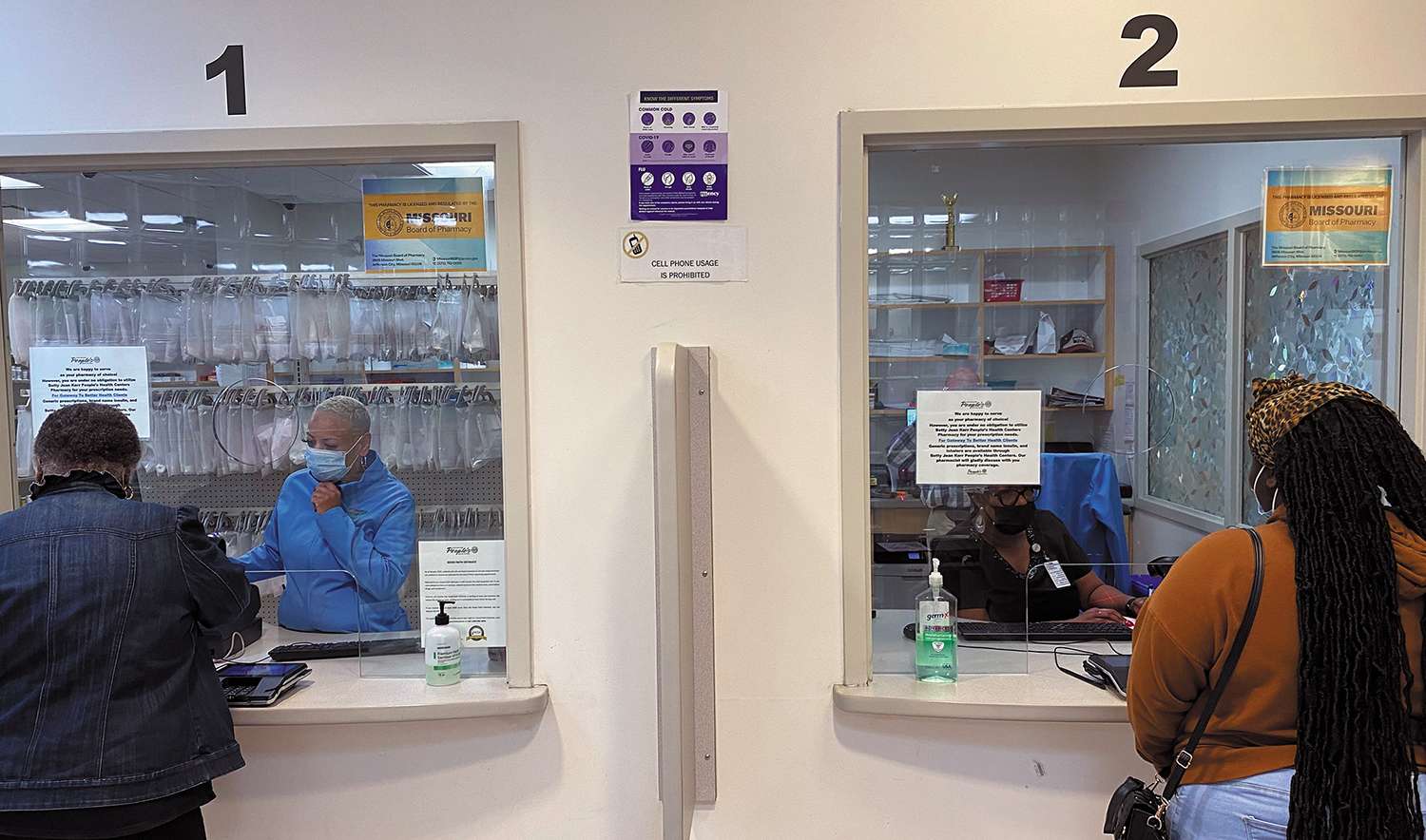
Dwayne Butler, CEO of the Betty Jean Kerr People's Health Centers FQHC, said the coordination happening through the network can have a profound impact on patient health outcomes as well as on the metrics on quality care. For example, he said that care coordination can lead to patients keeping their primary care follow-up appointments after specialty care. Keeping such appointments and adhering to post-care instructions can help people recover better and quicker. And it can lead to lower hospital readmission rates.
Patient empowerment
Kent said in addition to relying upon the Integrated Health Network to ensure patients can move more smoothly through the St. Louis safety net system, as a physician with SSM Health Saint Louis University Hospital, she has access to other resources and approaches to ensure patients' needs are addressed holistically, including when they get specialty care.

First, she said, is that SSM Health Saint Louis University Hospital prioritizes daily face-to-face huddles by the teams treating specialty care patients. In these multidisciplinary huddles, clinicians and other staff flag and address issues patients are facing.
Second, Kent said, is a transitional care clinic, also known as a BRIDGE clinic, which has a staff that meets with patients after their discharge from inpatient care to ensure their needs are met. BRIDGE stands for Bridging Recovery, Informing Decisions and Guiding Empowerment. This navigation includes making sure patients who have transportation needs receive help with that and that patients are set up for follow-up appointments and have all the prescriptions they need and understand how to take them, understand posttreatment care instructions and are equipped to follow them, and that any socioeconomic barriers to recovery are addressed. Kent said this transitional care clinic has been essential to helping patients with the many concerns that can stand in the way of successful specialty care treatment and recovery.
The last key element she mentioned is patient education, which she said should be woven into the entire approach. She said providers must take the time to confirm patients fully understand the path they are on with specialty care. Verifying patient understanding can make a life-or-death difference in their outcomes, she said.
Coordinating care and taking the time to get to know patients and comprehend their struggles and help them address those concerns are key to effective specialty care delivery, Kent said. "When you take care of them in this way, they still have barriers, but you've given them ways to get help. They can feel empowered. As a provider, I'm saying that I can't remove all your barriers, but I can help empower you."
Further reading: In St. Louis, SSM Health partners with other providers to assess and address barriers
