In 2016, CHRISTUS Health's Department of Academics consolidated all the residency programs in CHRISTUS under one Designated Institutional Official (DIO) and one Graduate Medical Education Committee (GMEC). This consolidation allows for easier intra- system elective rotations, mitigates the risk of accreditation problems, improves retention of residents as physicians after graduation, and provides a more consistent experience for our medical residents. Part of this standardization included a standard, system-wide curriculum for medical residents on topics related to mission and ethics. The curriculum is only for residency programs sponsored by CHRISTUS Health. The curriculum began in June 2018 and will finish its first cycle in June 2020.
The goals of the curriculum are to: provide the information related to mission and ethics necessary to practice in CHRISTUS facilities; help residents build the skills they need to identify, analyze, resolve ethical issues in their patients' care;1 and convey this material in a manner relevant to their clinical practice.
CURRICULUM CONTENT
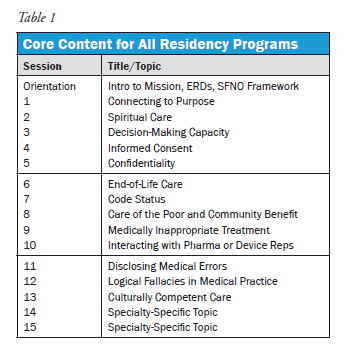
In developing the curriculum we discovered there is little literature on how to best teach ethics to residents or what content to teach them.2 Some specialty groups have specific guidance, for example the American Academy of Pediatrics has a guide on what topics to teach and teaching aides to assist faculty.3 However, most specialties do not have such guidance. Thus, our curriculum is based on a combination of the existing literature, specialty recommendations as they exist, and our own experience of what residents should know. From these sources we developed a core set of topics that all medical residents should receive, regardless of specialty. (Table 1) The core curriculum includes a 90-minute orientation session for all first-year residents, and five 60-minute sessions each year, totaling 16.5 hours over the three-year residency. The sessions are primarily case based. Certain topics have a combination of didactic content and role play.
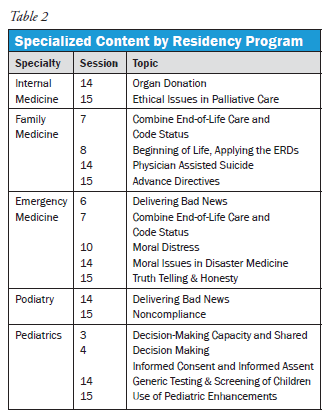
 To meet the third goal mentioned above, the sessions are tailored specifically to each program in three ways. First, each specialty receives some sessions unique to its field of medicine. (Table 2) The core curriculum includes two specialty- specific sessions but, for some specialties, we combine or eliminate sessions to make room for others. For example, the Emergency Medicine curriculum combines End-of-Life Care and Code Status into one session to make room for a session on Delivering Bad News. Second, the cases for each session are chosen specifically for each specialty. For example, while all specialties receive the same content for informed consent, cases for internal medicine are different from those in emergency medicine. Third, since our residency programs span two states, sessions discuss state-specific laws where relevant such as those regarding advance directives.
To meet the third goal mentioned above, the sessions are tailored specifically to each program in three ways. First, each specialty receives some sessions unique to its field of medicine. (Table 2) The core curriculum includes two specialty- specific sessions but, for some specialties, we combine or eliminate sessions to make room for others. For example, the Emergency Medicine curriculum combines End-of-Life Care and Code Status into one session to make room for a session on Delivering Bad News. Second, the cases for each session are chosen specifically for each specialty. For example, while all specialties receive the same content for informed consent, cases for internal medicine are different from those in emergency medicine. Third, since our residency programs span two states, sessions discuss state-specific laws where relevant such as those regarding advance directives.
The content for each session is developed at the CHRISTUS Health System Office, either by an ethicist or another content expert for the mission sessions. Each session is delivered locally, in-person, by the local ethicist, mission leader, ethics committee chair, an ethics committee member, or a content expert (e.g., director of spiritual care for the session on spiritual care). We hold a train-the-trainer program by webinar before the first session and record it for local facilitators who cannot attend.
MODIFIED SFNO FRAMEWORK
Since mnemonic tools are ubiquitous in medical training, we modified an existing mnemonic device to assist the residents in identifying, analyzing, and resolving ethical issues in their patient's care. (Figure 1) Jim Dubois developed the SFNO framework to assist in analyzing bioethics cases.4
SFNO stands for So Far, No Objections, or Stakeholders, Facts, Norms, Options. Identifying the Stakeholders (who will be significantly affected by the decision), Facts (what facts are relevant or disputed), Norms (what ethical principles, norms, or values are relevant or in conflict), and Options (what solutions are worth considering or compromising on) helps generate a starting point for moral analysis of a case.
Our Modified SFNO Framework places these four items into a three-step process; the added steps assist with the identification and resolution aspects of ethics consultation. The first step, clarify the central ethics question, narrows the focus of the discussion on the primary issue at hand. Too often, conversations and ethics consults focus on ancillary issues or get stuck down rabbit holes. The central ethics question might change throughout the course of a case as more facts emerge. The second step identifies a range of appropriate options. Casting a wide net and eliminating unacceptable options are helpful here. It is better to reject an option for a specific reason than to leave a potentially acceptable option unnamed. The third step, formulate an initial response, works towards resolution of the ethical issue. It is broad enough to allow the resident to resolve the issue on his/her own, present options to a patient or surrogate decision maker, or seek assistance from the ethics committee. It permits the resident to make a recommendation to the decision maker or to refrain from interfering. We stress with residents to not refrain from requesting an ethics consult. It is perfectly acceptable for them to say, "I don't know" as long as they then call someone who does.
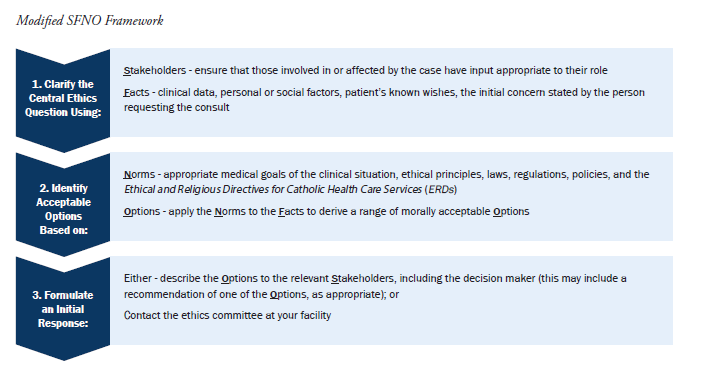
The presenters introduce the mnemonic in orientation and run through several cases with the residents. Throughout the remaining three years of the curriculum, they use the framework to analyze every ethics case discussed in the sessions. By combining the framework with the content, the curriculum prepares residents to identify, analyze, and resolve ethical issues in their own professional practice.
NEXT STEPS
We are conducting a study on the curriculum to contribute to the literature in this area. The study consists of pre- and post-surveys of the residents to evaluate their opinions on the content, length, delivery method, and self- assessed ability to identify, analyze, and resolve ethical issues in their patients' care. The study received approval from the CHRISTUS Health IRB. We plan to publish a detailed review once the study is complete. Afterwards, we anticipate expanding the curriculum to include other specialties and our pharmacy residents as well. We hope this will help others when designing ethics programs for medical residents.
ENDNOTES
- ASBH identifies these three actions as essential features of ethics consultation. American Society for Bioethics and Humanities, Core Competencies for Healthcare Ethics Consultation, 2011, 2nd edition, p 3.
- Manson, Helen. "The need for medical ethics education in family medicine training." Fam Med 40, no. 9 (2008): 658-64. Helft, Paul R., Rachael E. Eckles, and Laura Torbeck. "Ethics education in surgical residency programs: a review of the literature." Journal of surgical education 66, no. 1 (2009): 35-42.
- Diekema, Douglas, Steven R. Leuthner, and Felipe E. Vizcarrondo. American Academy of Pediatrics Bioethics Resident Curriculum: Case-Based Teaching Guides. American Academy of Pediatrics. October 2017.
- Dubois, J. "Solving ethical problems: analyzing ethics cases and justifying decisions." Ethics in Mental Health Research (2008): 46-57.
BECKET GREMMELS, PH.D.
System Director of Ethics
CHRISTUS Health
Irving, Texas
[email protected]