By LISA EISENHAUER
After dramatically reducing the number of women dying from pregnancy-related causes, California is now looking at ways to improve outcomes for black women, who, as a group, are still dying from pregnancy and childbirth complications at a rate about three times higher than the general population.

Nurse Tierra Dean checks on a patient and her newborn at SSM Health St. Mary's Hospital in St. Louis. The hospital delivers more babies than any other in the SSM Health system. Like other hospitals, it has put vetted practices in place to prevent maternal deaths and complications.
Courtesy SSM Health
The efforts being led by the California Maternal Quality Care Collaborative are among others across the nation targeting the racial disparity in maternal mortality rates.
The collaborative was founded at Stanford University School of Medicine with support from the state of California in response to rising rates of death and profound complication among pregnant women. It counts almost all hospitals with maternity units in the state among its members, including those in the Providence St. Joseph Health and CommonSpirit Health systems.

Registered nurse Elizabeth Mueller steadies newborn Blaike Jackson on the chest of his mother, JaiDa'h Jackson, just after his birth at SSM Health St. Mary's Hospital in St. Louis, in June 2017. The hospital is among many that use multiple measures, such as cesarean section rates, to judge if its efforts to improve outcomes for pregnant women are working.
Laurie Skrivan/St. Louis Post-Dispatch/Polaris
The decrease in maternal deaths in California has come as the rate for the nation has increased. Since 2006, when the collaborative was founded, the California Department of Public Health says the rate has dropped 55 percent from 16.9 deaths per 100,000 live births to 7.3 deaths in 2013, the last year for which publicly released data for the state are available. In contrast, the national maternal mortality rate climbed from 15.7 in 2006 to 17.2 deaths per 100,000 live births in 2015, according to the Centers for Disease Control and Prevention. But in both California and the nation, pregnancy-related deaths among black woman remain nearly three times the overall rate.
Data driven
Cathie Markow, the collaborative's administrative director, says data analysis indicates that the disparity in the rates are not explained by risk factors such as obesity or high blood pressure. The collaborative's website cites data that shows "even in the absence of risk factors such as age over 35 years, lack of health insurance, inadequate or no prenatal care and less than high school education, the U.S. system of health care is not protecting Black mothers and birthing people from experiencing higher numbers of deaths or life-threatening complications during pregnancy and childbirth."
"That data starts to suggest that the usual suspects are not the driver and it is impossible to avoid the idea that there is racism at play within (health care) institutions that needs to be addressed," Markow says.
To specifically target the disparity, the collaborative this year launched an initiative called the California Birth Equity Collaborative, a partnership with hospitals, advisory groups and community-based organizations led by black women.
The goal of the initiative is to "improve care, experiences, and outcomes for, by and with black mothers and birthing people during hospital births," according to its website. Its work product is expected to identify best practices for hospitals and knit together clinical and sociocultural interventions by community-hospital partnerships.
Models of success
Dr. David Lagrew is the executive medical director and executive leader of the Women and Children's Services Institute for the Southern California region of Providence St. Joseph Health. He is on the executive committee of the California Maternal Quality Care Collaborative. He says the equity collaborative is setting up a two-year pilot study on disparities in maternal mortality that will involve several hospitals and test potential interventions to improve pregnancy outcomes for black women. Exactly what those interventions will be is still being decided.

Lagrew
Lagrew says it's clear that the race-based disparity in maternal deaths is tied to equity of care within the health care system at large. "It really does get back to care and how we counsel patients and how we listen to patients," he says. "There are some real lessons to be learned."
SSM's efforts
Like those in California and elsewhere around the country, hospitals in the St. Louis-based SSM Health system have put special practices in place to prevent birth-related deaths and complications. "We've developed order sets, we've developed protocols, we developed education for staff, we do simulations to learn to treat this stuff," says Pam Lesser, nursing director of perinatal services at SSM Health St. Mary's Hospital in St. Louis.
Lesser says St. Mary's has been the lead in initiating those practices and resources for SSM Health's four-state system because it handles more deliveries than any other hospital in the system — about 3,300 a year — and because of its designation as a high-risk pregnancy referral center.

Lesser
The impact of efforts to reduce the maternal mortality rate are hard to track, Lesser and others say, because even though it's a huge cause for concern, the number of women who die due to pregnancy is not itself huge (about 700 a year across the nation) and the annual figures don't come out quickly in part because under CDC rules the rate includes deaths up to a year after delivery.
St. Mary's is among many hospitals using multiple measures to judge if its efforts are improving outcomes for pregnant women. Those measures include looking at how much time birth mothers spend in the intensive care unit, how many undergo cesarean sections and how much blood is transfused to them.
Community effort
When it comes to addressing the racial disparities in health outcomes for mothers, Lesser believes that care providers need to have the social competence to relate to patients of various races and ethnicities. But she also believes that factors beyond the reach of hospitals are at play. She cities social determinants like access to care, insurance coverage and transportation. "Those are really big issues that we are absolutely part of working on," she says.

A lifelike manikin is used in simulation training on an emergency delivery at Providence Holy Cross Medical Center in Mission Hills, Calif.
Photos courtesy Providence Holy Cross Medical Center
The hospital has partnered in various community initiatives to address racial equity overall in the St. Louis region. For example, it is part of a coalition called Generate Health that is trying to "advance racial equity in pregnancy outcomes, family well-being, and community health" by bringing resources to bear on issues effecting vulnerable mothers and babies. The organization runs tours in low-income communities to give medical and nursing students a visceral understanding of how poverty and racism impact upon health inequities.

Kendig
Susan Kendig, women's health integration specialist at St. Mary's, has had a lead role in the development of pregnancy-related best practices by the Council on Patient Safety in Women's Health Care and the Alliance for Innovation on Maternal Health. Both are national initiatives supported by professional organizations. AIMH is also supported by the federal Health Resources and Services Administration. Their recommendations include mental health care and transitioning from maternal to well-woman care. They encourage "a community-wide effort that includes hospitals, clinical providers and community organizations and patients with lived experience to work together to address maternal mortality," Kendig says.
"Reduction of Peripartum Racial/Ethnic Disparities," one of the council's "patient safety bundles," recommends providers:
- Establish systems to accurately document self-identified race, ethnicity and primary language.
- Provide staff-wide education on peripartum racial and ethnic disparities and their root causes and on best practices for shared decision-making.
- Engage diverse patient, family and community advocates who can represent important community partnerships on quality and safety leadership teams.
"That bundle is designed to be overlaid over all of our work," says Kendig.
Like Lesser, Kendig says attempts to end racial disparities in health care have to go beyond clinical settings to succeed. She believes communities have to unite to address issues related to access and equity. "You cannot do this if you're only looking at health care providers," Kendig says.
Collaborative’s recommendations inform care at Providence Holy Cross
When a patient deemed to be at high risk for hemorrhage checks into the maternity unit at Providence Holy Cross Medical Center, a crash cart is parked outside the mother-to-be's door.
The obstetrics team knows what's in it, where everything is located and how to use every item in the event of a life-threatening bleed, according to Julie Masson, a registered nurse who is the perinatal simulation educator at the hospital in Mission Hills, Calif.
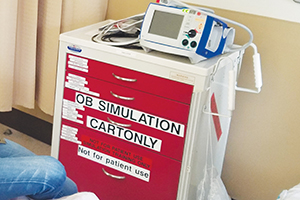
A cart outfitted with items that might be needed in a maternal emergency is part of the simulation training at Providence Holy Cross Medical Center in Mission Hills, Calif.
Holy Cross is part of Providence St. Joseph Health, which operates hospitals and clinics in seven states.
The crash cart contains every item recommended in the California Maternal Quality Care Collaborative's guidance on maternal hemorrhage. "We base everything we do off of their recommendations," says Masson.
Masson credits the collaborative's work for the decrease in maternal mortality and morbidity numbers across the state in recent years. "Everything they present is based on research and best practice," she says. "It's easy to see that by following these guidelines, we are providing the safest and best possible care for our mothers."
Dr. David Lagrew, executive medical director and executive leader of the Women and Children's Services Institute for the Southern California region of Providence St. Joseph Health, credits the use of the collaborative's resources and training guidance throughout the system for contributing to the fact that the system had no deaths from birth-related complications in 2017 among the 75,000 women who delivered at its hospitals.
The collaborative and Providence St. Joseph follow the Centers for Disease Control and Prevention definition of maternal mortality, which covers deaths of mothers up to 12 months after giving birth "from any cause related to or aggravated by the pregnancy."
The care collaborative's administrative director, Cathie Markow, says that in addition to creating resources to help train maternity specialists in how to handle emergencies, the organization is urging hospitals to educate emergency room staffers to watch for warning signs of potential complications, such as moderately high blood pressure as an indicator of stroke risk, when treating pregnant patients and patients who are postpartum.
Markow says a national initiative called Alliance for Innovation on Maternal Health is developing more resources specifically for emergency department staff to heighten their awareness of subtle warning signs and patients' self-reporting of confounding symptoms like a sense that something is not right.
Masson says Holy Cross obstetric team members drill on the California collaborative's recommendations during trainings using high-fidelity manikins to simulate delivery room emergencies, such as hemorrhages, preeclampsia and cardiac arrests.
"We like to practice 'in-situ,' which means that we conduct our simulations in the patient care environment, such as in a patient room," Masson says. "This is a really great way to train and practice because staff use the equipment and supplies that they are used to, and it allows us to uncover latent safety gaps."
Speak up
Those gaps can include having supplies stowed in places where they are too hard to get to in an emergency or weaknesses in the lines of communications, such as staffers being reluctant to speak up when they are unclear on an order.
"We are always talking with our teams about closing the loop," Masson says. "If you're not sure what you heard or you don't agree with something, then you want to speak up and clarify what you heard. This is called closing the loop in communication."
Masson says the main benefit of the resources provided by the collaborative and the training that puts them into practice at Holy Cross is quicker and more effective responses to maternal emergencies, resulting in more lives saved.
"It boils down to the decrease in the delay of care: identifying patients at risk, recognizing signs and symptoms of complications and responding without hesitation," Masson says.
— LISA EISENHAUER
Linking racism, health outcomes is not novel; report urges better maternal care
The idea that race plays a role in health outcomes is not a new one. In August 2000, Dr. Camara Phyllis Jones laid out a theory about racism affecting health care in an article called "Levels of Racism: A Theoretic Framework and a Gardener's Tale" in the American Journal of Public Health.
A link to her article is posted on the website of the California Birth Equity Collaborative, which is looking at what's causing black women to die from childbirth complications at a much higher rate than others and how to prevent it.
Jones' article identifies three forms of racism:
- Institutionalized: defined as differential access to the goods, services and opportunities of society by race. This form is "often evident as inaction in the face of need," says the article.
- Personally mediated: prejudice in which differential assumptions about the abilities, motives and intentions of others are made according to their race and discrimination in which differential actions are taken toward others because of their race.
- Internalized: an acceptance by members of the stigmatized races of negative messages about their own abilities and intrinsic worth.

A Twitter post by Serena Williams shows her and her baby daughter, Alexis Olympia Ohanian Jr., and urges support for a UNICEF initiative aimed at improving health care for mothers and newborns. The photo was posted about a month after Williams went public with the story of her own difficult pregnancy and complications.
Race itself is a societal classification that serves as "a rough proxy for socioeconomic status, culture and genes" but not a biological one that "reflects innate differences," wrote Jones, who has worked at the Harvard School of Public Health and the Centers for Disease Control and Prevention and is now a senior fellow at the Morehouse School of Medicine in Atlanta.
"For this reason, some investigators now hypothesize that race-associated differences in health outcomes are in fact due to the effects of racism," Jones wrote.
Racism's potential impacts on health outcomes is also a part of more recent reports, including "Eliminating Racial Disparities in Maternal and Infant Mortality," released in May by a progressive think tank, the Center for American Progress, based in Washington. In linking racism and the much poorer pregnancy outcomes of black women, the report cites statistics that show black women face more barriers, such as lower income and lack of transportation, than others to quality care.

Taylor
Jamila Taylor is the lead author of the report. She is now director of health care reform and senior fellow at The Century Foundation, a progressive think tank based in New York. Despite her report's grim findings, she sees hope that more black mothers like herself will thrive in the future.
For one thing, the topic has gotten national attention in recent years. Taylor points to tennis superstar Serena Williams revealing her ordeal after the birth of her daughter in 2017. In an interview with Vogue magazine, Williams said her own knowledge about her health history of blood clots was at first dismissed by clinicians when she complained of shortness of breath the day after she underwent a cesarean section. Williams said that it was only because she insisted on a CT scan that her suspicion of a pulmonary embolism was confirmed and the proper treatment given.
Taylor says the "Lost Mothers" investigation on maternal care and preventable deaths produced in 2017 and 2018 by the nonprofit ProPublica news service and National Public Radio also put a spotlight on the poor care provided in some hospitals that serve mostly minority women.
"I think that series as well as Serena Williams telling her story really launched the issue into the public consciousness in a way I had never seen before," Taylor says.
Taylor wants her report to be a plan of action. It suggests policy strategies including addressing maternal and infant mental health; ensuring supports for families before and after birth; and improving data collection and oversight.
"I'm hopeful the blueprint will be used by both the federal and state policy makers to inform solutions that they will put forward to address this issue and not only put forward or propose, I want to see things passed," she says.
— LISA EISENHAUER