By JULIE MINDA
It's been about a year since CommonSpirit Health formally launched community health worker networks in six of its markets and several of those networks are gaining traction and having a measurable impact on the lives of vulnerable people who previously
had struggled to access health and social services.
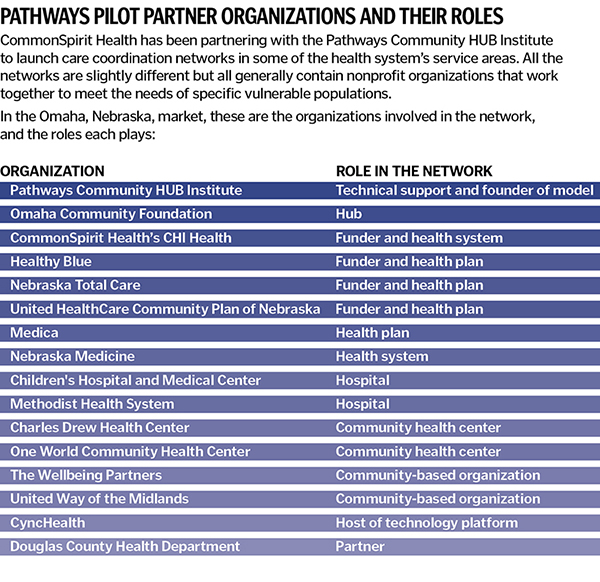
Working with the nonprofit Pathways Community HUB Institute, CommonSpirit spurred the creation of, and provided seed funding for, the networks. The networks engage community health workers in identifying vulnerable individuals and guiding them on specific
pathways to attain services so they can address the most pressing socioeconomic concerns they face. Under the approach, the community health workers' pay is partly based on their ability to meet their clients' needs.
Ji Im is senior director of community and population health at CommonSpirit, which has 140 hospitals and 1,000-plus additional care sites in 21 states. She says, "This is a community care model, not a hospital program. This Pathways program is owned
by and sits in the community. We are a community partner in this. And this is a significant shift" from approaches in which hospitals lead such efforts.
 Im
ImThe Pathways work is an offshoot of CommonSpirit's ongoing efforts around what it calls Community Connected Networks. These networks link clinical care providers and social service organizations within a referral system and technology platform to
address people's needs.
Hub and spoke
Im says CommonSpirit became aware of Pathways Community HUB Institute as it was seeking to enhance community-based care
coordination programs it had established in some of its markets.
The institute has developed a hub-and-spoke model that has a community organization at the center of a network of agencies in a particular locality. Two or more agencies in the network hire community health workers to engage and coach people in addressing
their pressing health and social service needs.
Also involved in these collaborations are organizations that have an interest in or a direct hand in meeting the needs of the program's clients. Those partnering organizations can include health systems, federally qualified health centers, managed
care organizations, government entities and social service providers. The partners fund the work with grants, philanthropy and payments from some insurers.
The institute helps train and certify the organization at the hub of the model and the community health workers.
The community health workers guide clients in the completion of pathways, or specific steps toward resolving particular health and social service concerns (see sidebar). The workers do this by connecting
the clients with organizations that can address their needs. The community health workers track and document clients' progress along the pathways in a database.
Pilots
When CommonSpirit first signed on with the Pathways Community HUB Institute around 2020, it committed $1 million to the work the institute would need to do to support communities in CommonSpirit service
areas as they implemented the model. That $1 million investment spurred an additional $3 million in investments from other funders that helped pay for startup infrastructure.
About two years ago, CommonSpirit hosted an informational session on the model with all its markets and invited those that wished to pilot the institute's model to do so. The six markets that were ready to move forward were Omaha, Nebraska; Brazos
County, Texas; King County and Pierce County, Washington; San Joaquin, California; Clark County, Nevada; and Maricopa County, Arizona.
Some have moved from the pilot phase to full commitment to the model. CommonSpirit intends to expand it to more of its markets.
Catalyst
Im says because all the CommonSpirit service areas differ in terms of their assets, resources, needs and shortcomings, each has been proceeding at its own pace and each looks a little different in its
implementation of the Pathways model. "Every community is a snowflake," Im says.
But in all six markets, CommonSpirit and its hospitals are functioning as catalyst, connector, collaborator and informal consultant in building out the hub-and-spoke network.
Im says the hub organizations have been starting small, with client populations identified as among the most vulnerable. The hub organizations have been growing the client base and network as they prove to their existing and prospective partners
the validity of the approach. The networks have shown that they have been very effective in connecting clients to services, improving their health outcomes, stabilizing their socioeconomic circumstances and improving how they access care.
 Li
LiBrian Li, CommonSpirit system director of community health strategic initiatives, notes that Pathways network partners get access to the data the community health workers put into the database. He says that data is extremely valuable to CommonSpirit
— it reveals which social service and medical needs are most difficult to meet in its communities. This intelligence can illuminate gaps in community services that CommonSpirit can address through programming and investment.
Community bank
In some cases managed care organizations are involved in and support the networks and pay for the services their members receive from the community health workers. However, in many cases, there
is no reimbursement source. So, the care navigation networks rely on a "community bank" approach, says Im.
 CommonSpirit Health's Dignity Health St. Rose Dominican in the Las Vegas area is part of a group of community organizations that is collaborating to provide community health worker support to people in vulnerable populations. Here,
community health worker Maria Ambriz, left, meets with client Roxana Henriquez to complete a risk assessment.
CommonSpirit Health's Dignity Health St. Rose Dominican in the Las Vegas area is part of a group of community organizations that is collaborating to provide community health worker support to people in vulnerable populations. Here,
community health worker Maria Ambriz, left, meets with client Roxana Henriquez to complete a risk assessment.Organizations in the networks put money into a community bank. The money can cover the Pathways hub organization's operating costs, including infrastructure and community health worker services.
For instance, the care navigation network in Omaha is addressing the needs of pregnant women at risk of poor birth outcomes. CommonSpirit and three managed care organizations — United HealthCare Community Plan of Nebraska, Healthy
Blue Nebraska and Nebraska Total Care — each have contributed funds to the network's community bank. Those funds are going toward the hub's operations and toward reimbursing for the community health workers' services to navigate
clients to any additional services from other organizations, such as prenatal services from a health care provider.
In markets that have advanced beyond the pilot stage, some of the capital pays bonuses that the community health workers earn when their client completes a pathway. The amount of the bonus varies by market.
Im says CommonSpirit is early in the Pathways work. The partners are finding that when it comes to addressing the social determinants of health and health inequities, efforts are "most effective when they are owned by and centered in the
community."
Whole-person approach
Julie Tousa is a social worker and the Pathways Agency program manager at CommonSpirit's Dignity Health St. Rose Dominican in the Las Vegas area. In Clark County that CommonSpirit
hospital is the Pathways Agency and St. Rose Dominican employs the network's four community health workers. A Pathways Agency is a single organization that has adopted the model.
 Tousa
TousaThe Nevada Ryan White Program that serves people with HIV and the hospital's R.E.D. Rose Program that promotes breast cancer screening and provides diagnostic services at no cost to uninsured women are primary funders of the network. The community health workers follow
up on referrals from partner organizations and invite people with HIV or cancer and low-income pregnant women to join the Pathways program.
The community health workers are bilingual in English and Spanish and have deep roots in the community. They build trust and offer support to clients working toward goals set out in pathways.
According to data from Tousa, the community health workers in Nevada aided 73 clients in 2022. That included closing 260 pathways. As a sampling, 10 of those were housing pathways, 24 were medical pathways, and 24 were food security pathways.
Tousa says the reason Pathways succeeds where other programs may fail in addressing social determinants is in large part that Pathways "takes a whole-person care approach.
"This allows us to look at the person and their family and all their risks. And we follow up (on solutions). And because of the trust that the community health workers build with the clients, the clients are more willing to engage."
The institute's 21 pathways
The Pathways Community HUB Institute model involves community health workers assessing and addressing social determinants of health and other needs. At the outset of a relationship with a client the community health worker
fills out an intake form that identifies the client's unmet needs.
The assessments will help the community health worker determine which of 21 different pathways to take in guiding the client to resolving the concerns.
The 21 standard pathways are:
- Adult education
- Developmental referral, for when a client's child may have developmental delays
- Employment
- Family planning
- Food security
- Health coverage
- Housing
- Immunization referral
- Learning
- Medical home
- Medical referral
- Medical adherence
- Medical reconciliation, for when there is a need for medical providers and/or pharmacists to evaluate a client's prescribed medications
- Medical screening
- Mental health
- Oral health
- Postpartum
- Pregnancy
- Social service referral
- Substance use
- Transportation