
As Americans and their health care systems struggle with both escalating costs and the growing complexity of a fragmented payer-provider landscape, a sobering truth looms over this essential social function: Despite operating the most technologically advanced and expensive health care system in the developed world, the U.S. produces health outcomes that lag behind every other industrialized nation — and even some developing ones.
Life expectancy, years of healthy disability-free life or healthspan, rates of premature death, infant and maternal mortality, and the prevalence of chronic disease, obesity and mental illness in the United States all trail those of other member nations of the Organisation for Economic Co-operation and Development (OECD). This is despite the U.S. spending more per capita on health care than any other country — $12,914 per person in 2021,1 compared with the OECD average of $4,488.2
While lack of universal access, fragmentation, high delivery costs, underinvestment in primary care, and the chronic underfunding of mental health services contribute to these outcomes, the uncomfortable reality is that the medical care we provide — no matter how sophisticated — accounts for only about 20% of an individual's health outcomes.3 Genetics certainly play a role, but it is now well established that the social determinants of health — income, education, housing, access to nutritious food and physical safety — along with individual behaviors, account for the vast majority of health outcomes and longevity.
In recent years, the field has also begun to reckon with the profound effects of trauma and chronic stress on both physical and mental health. These forces heighten the risk of substance use disorder, chronic illness and early mortality, while eroding the sense of safety and belonging that promotes healing. Conversely, faith, contemplative practice, purposeful living and nurturing relationships have been associated with improved health outcomes.4 If we are serious about addressing America's declining health metrics and rising costs, we must broaden our focus beyond treatment to include the deeper, integrated work of promoting whole-person health.
This begins by acknowledging that the prevailing biomedical model — which treats the human being as a collection of discrete organ systems, and the mind as an abstract entity housed in the brain — is no longer adequate. Neuroscientist Candace Pert famously coined the term bodymind to capture the inseparability of these domains.5 By omitting the hyphen, she signaled that while "body" and "mind" are conceptually distinct, they are biologically inseparable. Modern biology now confirms this unity: Emotions influence immune function, gene expression and even the microbiome, while physiological states shape mood, cognition and motivation.
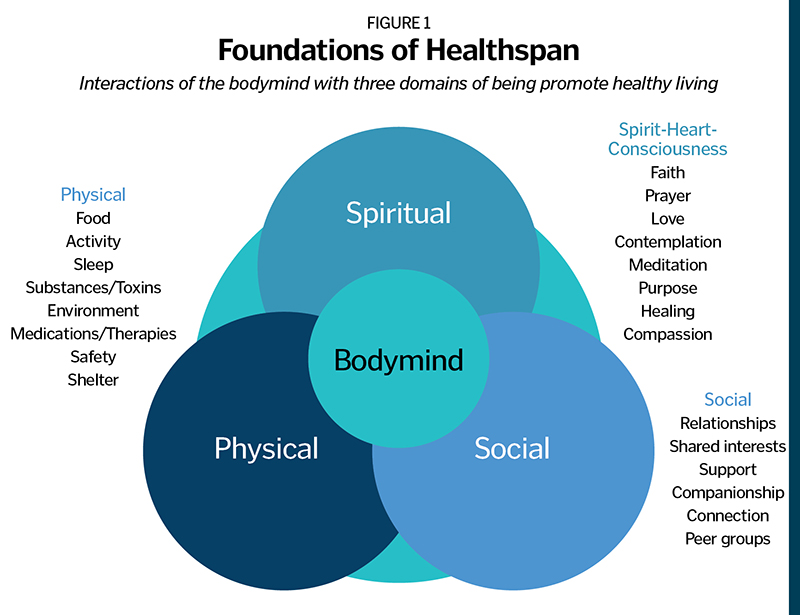
A practical way to visualize whole-person health is through three interconnected domains — physical, social and spiritual — each interacting dynamically with the bodymind, the integrated human organism that engages with all three. Together, these domains define the terrain of healthspan (see Figure 1.)
THE PHYSICAL DOMAIN: FOUNDATIONS OF DAILY LIVING
Health care leaders often refer to the physical and social domains when discussing the social determinants of health, and the evidence base is formidable.6 Hundreds of prospective and population-based studies demonstrate that healthy diet, regular physical activity, restorative sleep, and avoidance of smoking and alcohol misuse significantly increase longevity and reduce the risk of cancer, cardiovascular disease and neurodegenerative disorders. The lifestyle plus factors described by Dr. Eric Topol, director and founder of Scripps Research Translational Institute, in his book Super Agers: An Evidence-Based Approach to Longevity, represent the most concrete and accessible avenues for improving healthspan — but they are only part of the path toward true whole-person wellness.
Emerging research suggests that these behaviors act not only through risk reduction but also through physiologic optimization — improving mitochondrial (the cellular organelles that convert nutrients into usable energy) function, reducing systemic inflammation, and enhancing cellular repair mechanisms that slow biological aging.7 Regular aerobic activity, for example, is associated with increased brain-derived neurotrophic factor levels, promoting neuroplasticity and cognitive preservation into late life. Diets rich in whole foods, omega-3 fatty acids and polyphenols have been linked to improved metabolic flexibility and reduced incidence of frailty. Adequate sleep, long overlooked in population health, is now recognized as a pillar of immune regulation and memory consolidation.
When viewed together, these physical determinants of health embody a truth both ancient and modern: that the bodymind is not a passive recipient of disease, but an adaptive system capable of repair and renewal when its foundational needs are met.
THE SOCIAL DOMAIN: CONNECTION AS MEDICINE
The adage that human beings are social animals is both self-evident and profoundly substantiated by research. Social relationships predict not only emotional well-being but also physical survival. Meta-analyses involving hundreds of thousands of participants have shown that social isolation increases mortality risk as much as smoking 15 cigarettes a day, while loneliness predicts higher rates of cardiovascular disease, stroke, depression and dementia.8
The Harvard Study of Adult Development — which is composed of two groups of men, the Grant Study and the Glueck Study, and now spans more than eight decades — provides a deeply human window into this science. Among men followed from adolescence into late life, the single most powerful predictor of health status at age 80 was the quality of their relationships at age 50. Those with stronger relational health — trust, belonging and emotional safety — were significantly less likely to develop chronic disease or cognitive decline. In effect, love and connection serve as buffers against physiological wear and tear, moderating stress responses and supporting immune function.9
These findings remind us that health is not produced in isolation, but in community. The relationships that sustain us — families, friendships, neighborhoods and peer groups — constitute a form of public health infrastructure every bit as essential as hospitals and clinics. In the same way that clean water and sanitation transformed 19th-century health outcomes, rebuilding social cohesion may well define the next frontier of 21st-century medicine.
THE SPIRITUAL DOMAIN: THE REALM OF SPIRIT, HEART AND CONSCIOUSNESS
The spiritual domain — the realm of spirit, heart and consciousness — encompasses faith, prayer, meditation, contemplation, compassion and the lived experience of purpose and meaning. It is through this dimension that the bodymind experiences coherence, belonging and transcendence. Increasingly, evidence shows that these qualities are not merely existential comforts but potent biological and behavioral determinants of health and longevity.
People who live with a clear sense of purpose consistently demonstrate lower all-cause mortality, reduced risk of cardiovascular disease and slower cognitive decline. In the Rush Alzheimer's Disease Center's Rush Memory and Aging Project, older adults with higher purpose scores were nearly 50% less likely to develop Alzheimer's disease and experienced slower global cognitive decline.10 A meta-analysis of more than 50,000 participants confirmed that a strong sense of life purpose is associated with a substantially lower risk of dementia.11 Finally, in a meta-analysis of more than 130,000 participants, those with a higher sense of purpose in life had a 17% lower risk of all-cause mortality and a comparable reduction in cardiovascular events.12
Spiritual and contemplative practices appear to work through overlapping mechanisms. Regular meditation and prayer are associated with lower circulating inflammatory cytokines, reduced cortisol reactivity and enhanced vagal tone, all markers of physiologic resilience.13 Mindfulness-based stress reduction programs have been shown to improve glucose metabolism and blood-pressure regulation and even preserve telomeres, the protective structures at the ends of chromosomes, which seem to shorten as a function of biological aging.14 Functional MRI studies demonstrate that long-term meditators maintain greater cortical thickness and connectivity in regions governing empathy, attention and emotional balance.15
When viewed together, these physical determinants of health embody a truth both ancient and modern: that the bodymind is not a passive recipient of disease, but an adaptive system capable of repair and renewal when its foundational needs are met.
Taken together, the data illuminates what centuries of spiritual tradition have taught: that contemplative awareness and purposeful living are not ancillary to health but central to it. Spiritual engagement — whether through faith, service or mindful presence — appears to fortify both the neural circuitry and the molecular architecture of well-being. In doing so, it extends an individual's healthspan not only by preventing disease, but by deepening their experience of meaning, compassion and connection that define a life well lived.
INTEGRATING THE THREE DOMAINS: A COMMUNITY MODEL FOR HEALTHSPAN
Recognizing the opportunity to improve health outcomes and healthspan on a communitywide basis, Nevada County has begun translating this framework into action. Dignity Health Sierra Nevada Memorial Hospital and Nevada County in California have partnered to launch HealthSpan Nevada County. This new community organization is dedicated to promoting and facilitating behaviors across all three domains — physical, social and spiritual — that demonstrably enhance both health outcomes and human fulfillment.
Taken together, the data illuminates what centuries of spiritual tradition have taught: that contemplative awareness and purposeful living are not ancillary to health but central to it.
Startup funding from both partners has enabled early operational support, and a growing coalition of local leaders is now shaping the organization's governance and strategy. The founding vision is clear: to help all residents of Nevada County live longer, healthier and more meaningful lives by aligning local systems, organizations and community assets around evidence-based health-promoting practices.
Working with policy strategist Micah Weinberg, PhD, the group engaged community stakeholders in a series of sessions from late 2024 into early 2025 to identify the core pillars of the initiative: food, social connection, activity, and youth and family (see Figure 2). These pillars form the operational backbone of HealthSpan Nevada County. A guiding white paper, developed by the working group, outlines the governance structure, metrics and early-stage priorities.16 An executive director has been appointed to advance implementation, expand partnerships and identify early demonstration projects designed to strengthen one or more domains of healthspan while reinforcing the others.
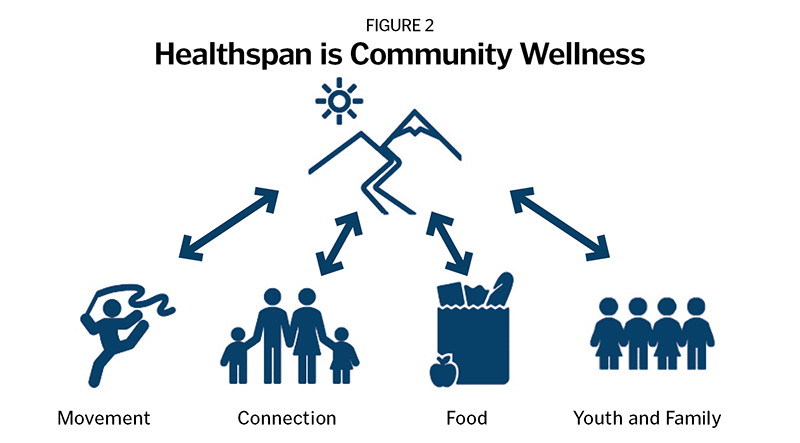
This local effort embodies what the evidence has long shown: that longevity and well-being are not the product of medical technology alone, but of daily environments that support purpose, connection, nourishment and movement. HealthSpan Nevada County seeks to make those supports not exceptional, but ordinary, woven into the fabric of community life.
A MODEL FOR COMMUNITY REALIGNMENT AROUND WELLNESS
The work unfolding in Nevada County represents more than a local innovation; it signals a shift in how communities across the country might reclaim ownership of their health. In an era of rising chronic disease and unsustainable health care costs, the HealthSpan model offers a replicable pathway — anchored in science yet grounded in local relationships.
By investing in food security, physical activity, social connection and purpose-driven living, communities can address the root causes of disease while cultivating resilience, fulfillment and equity. The potential return on investment is immense: Every additional year of healthspan — a year lived free from chronic illness and disability — translates into lower health care expenditures, improved productivity and stronger civic participation.
The Nevada County experience offers a prototype for other rural and midsized regions seeking to realign their health care and social systems around wellness rather than illness. It demonstrates how health care organizations, public agencies, community nonprofits, schools, businesses and residents can co-create solutions that transcend institutional boundaries. What begins as a local collaboration can evolve into a national movement — a reframing of health policy to prioritize whole-person vitality across the lifespan.
As health care leaders, our task is to redefine success — not by the number of procedures performed or margins achieved, but by the sustained well-being of the people and places we serve. Extending lifespan is no longer enough; the opportunity before us is to extend healthspan — and, in doing so, to restore humanity to the heart of health care.
DR. SCOTT NEELEY is president and CEO of Dignity Health Sierra Nevada Memorial Hospital.
NOTES
- "California Health Care Almanac," California Health Care Foundation, August 2023, https://www.chcf.org/wp-content/uploads/2023/02/NationalHealthSpendingAlmanac2023.pdf.
- "Health Spending Per Capita–Country Rankings," The Global Economy, https://www.theglobaleconomy.com/rankings/health_spending_per_capita/OECD/.
- Chenyu Li et al., "Realizing the Potential of Social Determinants Data in EHR Systems: A Scoping Review of Approaches for Screening, Linkage, Extraction, Analysis, and Interventions," Journal of Clinical and Translational Science 8, no. 1 (2024): https://doi.org/10.1017/cts.2024.571.
- Lucinda Rachel Grummitt et al., "Association of Childhood Adversity with Morbidity and Mortality in U.S. Adults," JAMA Pediatrics 175, no. 12 (2021): https://doi.org/10.1001/jamapediatrics.2021.2320; Harold G. Koenig, "Religion, Spirituality, and Health: The Research and Clinical Implications," ISRN Psychiatry 2012, no. 1 (2012): https://doi.org/10.5402/2012/278730.
- Candace B. Pert, Molecules of Emotion: Why You Feel the Way You Feel (Scribner, 1997).
- Yanping Li et al., "Impact of Healthy Lifestyle Factors on Life Expectancies in the U.S. Population," Circulation 138, no. 4 (2018): 345–355, https://doi.org/10.1161/CIRCULATIONAHA.117.032047; Yanping Li et al., "Healthy Lifestyle and Life Expectancy Free of Cancer, Cardiovascular Disease, and Type 2 Diabetes: Prospective Cohort Study," BMJ 368, no. l6669 (2020): https://doi.org/10.1136/bmj.l6669.
- Dr. Eric Topol, Super Agers: An Evidence-Based Approach to Longevity (Simon & Schuster, 2025).
- Julianne Holt-Lunstad, Timothy B. Smith, and J. Bradley Layton, "Social Relationships and Mortality Risk: A Meta-Analytic Review," PLOS Medicine 7, no. 7 (2010): https://doi.org/10.1371/journal.pmed.1000316.
- George E. Vaillant, Triumphs of Experience: The Men of the Harvard Grant Study (Belknap Press of Harvard University Press, 2012); Robert Waldinger, MD, and Marc Schulz, The Good Life: Lessons from the World's Longest Scientific Study of Happiness (Simon & Schuster, 2023).
- Patricia Boyle et al., "Effect of a Purpose in Life on Risk of Incident Alzheimer Disease and Mild Cognitive Impairment in Community-Dwelling Older Persons," Archives of General Psychiatry 67, no. 3 (2010): https://doi.org/10.1001/archgenpsychiatry.2009.208.
- Angelina Sutin et al., "Sense of Meaning and Purpose in Life and Risk of Incident Dementia: New Data and Meta-Analysis," Archives of Gerontology and Geriatrics 105 (2023): https://doi.org/10.1016/j.archger.2022.104847.
- Randy Cohen, Chirag Bavishi, and Alan Rozanski, "Purpose in Life and Its Relationship to All-Cause Mortality and Cardiovascular Events: A Meta-Analysis," Psychosomatic Medicine 78, no. 2 (2016): https://doi.org/10.1097/PSY.0000000000000274.
- Richard Davidson and Bruce McEwen, "Social Influences on Neuroplasticity: Stress and Interventions to Promote Well-Being," Nature Neuroscience 15, no. 5 (2012): https://doi.org/10.1038/nn.3093.
- Elissa Epel et al., "Can Meditation Slow Rate of Cellular Aging? Cognitive Stress, Mindfulness, and Telomeres," Annals of the New York Academy of Sciences 1172, no. 1 (2009): https://doi.org/10.1111/j.1749-6632.2009.04414.x.
- Madhukar Dwivedi et al., "Effects of Meditation on Structural Changes of the Brain in Patients with Mild Cognitive Impairment or Alzheimer's Disease Dementia," Frontiers in Human Neuroscience 15 (2021): https://doi.org/10.3389/fnhum.2021.728993; Sara Lazar et al., "Meditation Experience Is Associated with Increased Cortical Thickness," NeuroReport 16, no. 17 (2005): https://doi.org/10.1097/01.wnr.0000186598.66243.19.
- "HealthSpan Nevada County Collaborative Community Wellness Proposal," HealthSpan Nevada County, May 2025.
QUESTIONS FOR DISCUSSION
Dr. Scott Neeley, the CEO and president of Dignity Health Sierra Nevada Memorial Hospital, points out that medical care accounts for only about 20% of a person's health outcomes. But he describes the HealthSpan project in Nevada County, California, as a way for the health system to partner with others to gauge what's already working, to encourage healthy behaviors, and to promote the need for healthy mind, spirit and community connections for overall wellness.
- What does this realignment around wellness rather than illness make you consider about how your health care setting responds to social determinants of health?
- Have you worked on collaborations outside of your health care setting? What were some of the stumbling blocks? How were they resolved?
- What did you learn from this article about reducing loneliness and addressing trauma and stress that you didn't know previously? Have you thought about ways to support this for patients, your work colleagues and for yourself? What's one way you look after your own health that others might find helpful to try?
- Looking beyond the physical domain of healthy living, how do your lived mission and values contribute to the spiritual and social domains of health for your patients, families, staff and communities?
