When Alma Valencia, a mother of two in Pasadena, California, left her job in fashion to care full time for her mom living with dementia, she didn't receive formal training or much guidance. "You just learn as you go," she said. Her days quickly filled with medication management, feeding, bathing and navigating benefits paperwork, alongside parenting and household duties. "Sometimes it feels like you're on an island by yourself," she admitted. Valencia's experience, which she shared when the 2025 edition of Caregiving in the U.S. was released by AARP and the National Alliance for Caregiving, is the reality for millions of families today.1
Family caregivers shoulder complex clinical tasks and major costs. Four bipartisan bills, new Medicare caregiver training codes and the Centers for Medicare & Medicaid Services' (CMS) Guiding an Improved Dementia Experience (GUIDE) Model give hospitals and other providers practical tools that can help.
THE LAY OF THE LAND
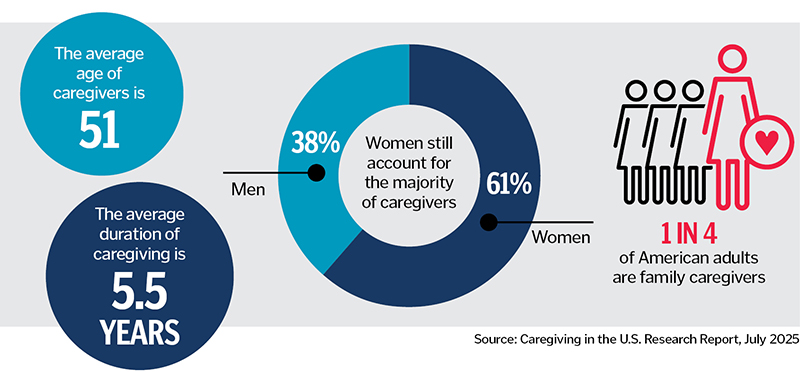
In 2025, an estimated 63 million Americans — nearly 1 in 4 adults — are providing care to adults or children with chronic conditions or disabilities — a 45% increase since 2015.2
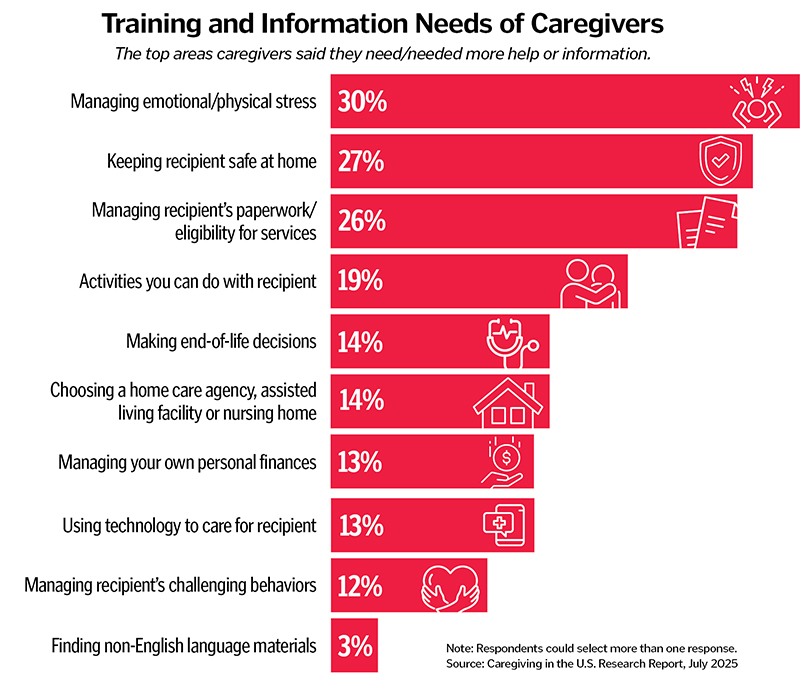
Tasks are increasingly clinical — including wound care, injections and complex medication regimens — yet only a minority receive related training. Only 11% of family caregivers receive any formal training to prepare them to assist with activities of daily living — such as bathing and dressing — and instrumental activities of daily living — such as preparing meals and managing finances — while two-thirds of caregivers help with at least one activity of daily living, and only 22% of caregivers receive training in handling medical or nursing tasks. Despite this, the majority of caregivers assist with these tasks.3
At the same time, more than half (58%) of family caregivers advocate with providers, community services or government agencies on behalf of their loved one. One in 4 wants help managing paperwork or navigating eligibility for services.
Financially, caregivers spend more than $7,200 on average annually out-of-pocket — roughly a quarter of their income — on home care, home modifications, assistive technology, respite care, transportation and more.4 For Catholic health care and the broader health environment, caring for caregivers is integral to caring for patients as they are an essential part of the care team. It's also practical: When caregivers are trained, equipped, supported and connected to resources, readmissions fall, adherence improves and burnout is less likely.
POLICY THAT MEETS FAMILIES WHERE THEY ARE
With a growing and diverse population of caregivers experiencing strain and feeling a lack of support, these findings reveal a call to action is needed by all involved to develop systems that can provide meaningful relief for family caregivers.
AARP supports a suite of bipartisan proposals designed to ease the financial and administrative challenges that make caregiving harder than it needs to be:
- The Credit for Caring Act, which is also supported by CHA, would create a targeted, nonrefundable federal tax credit to help offset a portion of out-of-pocket caregiving expenses for eligible working family caregivers.5
- The Lowering Costs for Caregivers Act would allow adults to use tax-favored health savings accounts, flexible spending accounts, health reimbursement accounts or Archer medical savings accounts to pay qualified medical expenses for their parents or parents-in-law — even if they aren't a tax dependent.6
- The Alleviating Barriers for Caregivers (ABC) Act would direct Medicare, Medicaid, the Children's Health Insurance Program and Social Security to simplify processes and communications so caregivers can more easily navigate benefits, saving time and frustration without feeling like they need a full-time case manager.7
- The Connecting Caregivers to Medicare Act would inform people about the voluntary option for people with Medicare to allow family caregivers to access their health information through 1-800-MEDICARE. For those who use this option, it can make it easier for their caregivers to communicate with Medicare to help their loved one or advocate on their behalf. As of this writing, this bill has not been introduced yet in the current Congress. However, the first three have been introduced and referred to the Senate Finance Committee and the House Ways and Means Committee or to both the House Ways and Means Committee and House Energy and Commerce Committee.8
When caregivers are recognized as part of the care team, they report greater confidence and stronger connections to community services. For providers, including caregivers in care planning can mean fewer discharge delays, reduced readmissions and better patient outcomes.
BUILDING PROFESSIONAL SUPPORT FOR CAREGIVERS
Policy matters, but practice is just as essential. Health care professionals are central to supporting family caregivers. When caregivers are recognized as part of the care team, they report greater confidence and stronger connections to community services. For providers, including caregivers in care planning can mean fewer discharge delays, reduced readmissions and better patient outcomes.
AARP has developed a new Healthcare Provider Resource Hub to help clinicians and systems build this support into routine practice.9 The hub:
- Highlights successful hospital programs that support family caregivers.
- Provides strategies for action and implementation.
- Offers stories and insights from leaders driving change in caregiver support.
- Hosts expert discussions on the benefits of involving family caregivers in care planning and delivery.
With CHA's network of more than 650 hospitals and 1,600 long-term care and other health facilities in all 50 states, AARP hopes these resources may be shared widely, equipping front-line staff with proven tools and amplifying impact across Catholic health systems.
CAREGIVER TRAINING TO LESSEN RISKS AND FEARS
Clinical leaders often ask, "How do we make time for caregiver education?" Medicare has given a practical answer. In the 2024 and 2025 Physician Fee Schedules, released by CMS, codes for caregiver training services were finalized and expanded so clinicians can bill for training family caregivers to carry out patient care plans.10 (Key codes include CPT Codes 97550–97552 and 96202–96203, which became effective in the 2024 calendar year, and HCPCS Codes G0539-G0540 and G0541–G0543, which became effective in the 2025 calendar year. More details are available in the fee schedules.)
CMS has also clarified that caregiver training services can be furnished via telehealth. This was temporary for 2025 but will be permanent under the final Calendar Year 2026 Medicare Physician Fee Schedule rule.
Paying for caregiver training aligns incentives. Providers are compensated for teaching, beneficiaries get safer care at home, and family caregivers gain confidence and competence. Valencia, the caregiver mentioned earlier, initially watched YouTube videos for help learning skills. However, these codes could have meant learning wound care directly from her mother's clinicians — with fewer risks and less fear.
GUIDING CAREGIVERS TO DEMENTIA SUPPORT
More than 6 million Americans live with dementia, with 14 million projected cases expected by 2060.11 Because many people with dementia also have multiple chronic conditions, providing support and managing their care can present mental, physical, emotional and financial strains for caregivers.
 For people living with dementia and their family caregivers, Medicare's Guiding an Improved Dementia Experience (GUIDE) Model offers care coordination, caregiver training, respite and 24/7 support.12 CMS launched GUIDE in July 2024, and, as of late 2025, said it had 327 organizational participants nationwide. Hospitals, nursing homes and other providers can refer eligible patients to providers who participate in the GUIDE model.
For people living with dementia and their family caregivers, Medicare's Guiding an Improved Dementia Experience (GUIDE) Model offers care coordination, caregiver training, respite and 24/7 support.12 CMS launched GUIDE in July 2024, and, as of late 2025, said it had 327 organizational participants nationwide. Hospitals, nursing homes and other providers can refer eligible patients to providers who participate in the GUIDE model.
For Valencia, GUIDE could have offered structured respite and around-the-clock advice, reducing her isolation and giving her mother's care team a clearer line of sight into caregiving challenges at home.
CAREGIVER SUPPORT
With the growing demand for family caregivers to serve as the primary source of support for older adults with chronic conditions or other disabilities, efforts to support, train and provide financial relief for caregivers can help lessen the stress and challenges. Clinicians can take steps to help support them through multiple avenues, from education to connecting them to financial and administrative support:
- Identify the caregiver. Ask, document and flag the primary family caregiver (and others if appropriate) in the electronic health record.
- Train and bill. Help map common diagnoses to enable opportunities for appropriate caregiver training services. Use CPT and HCPCS codes to report caregiver training services as appropriate, including telehealth options.
- Refer to GUIDE (for dementia). Create a referral pathway to local GUIDE organizations (participants) or dementia care programs.
- Connect families to resources. Share AARP's Family Caregiving Guide,13 resource guides14 and resource line at admission and discharge. Visit www.aarp.org/caregiving for more details.
- Leverage CHA networks. Through its network of Catholic hospitals, long-term care and other health facilities, CHA can be a powerful partner in disseminating caregiver-support strategies and tools across systems nationwide.
FAITH, MISSION AND THE WORK AHEAD
Catholic health care's tradition calls health care professionals to accompany the patient and their family. Family caregivers aren't "visitors" — they are part of the care team. As the population ages and longevity extends, our systems must treat them that way by recognizing, including and engaging, training (if they would like it) and supporting them.
If Valencia's health team had been able to bill for caregiver training, enroll her mother in GUIDE, and point her toward a modest but meaningful tax credit and clearer Medicare navigation, her sacred work of caregiving could have continued with less fear, fewer avoidable complications and a little more breathing room. That is a vision CHA and AARP share, and it's achievable — now.
NICOLE DURITZ is director of family and caregiving for AARP. RHONDA RICHARDS is government affairs director for AARP.
NOTES
- Caregiving in the U.S. 2025 is a research report that draws from a national online survey completed by approximately 6,800 family caregivers aged 18 and older. "Caregiving in the U.S. 2025," AARP and National Alliance for Caregiving, https://www.aarp.org/pri/topics/ltss/family-caregiving/caregiving-in-the-us-2025/; Beth Pinsker, "America's 63 Million Family Caregivers Are Mostly Unpaid, Stressed and Begging for Help," MarketWatch, July 24, 2025, https://www.marketwatch.com/story/americas-63-million-family-caregivers-are-mostly-unpaid-stressed-and-begging-for-help-632690ff?.
- "Caregiving in the U.S. 2025."
- "Caregiving in the U.S. 2025."
- Laura Skufca and Gerard 'Chuck' Rainville, "Caregiving Can Be Costly — Even Financially," AARP, June 29, 2021, https://www.aarp.org/pri/topics/ltss/family-caregiving/family-caregivers-cost-survey/.
- "S.925–Credit for Caring Act of 2025," Congress.gov, https://www.congress.gov/bill/119th-congress/senate-bill/925?.
- "S.1565–Lowering Costs for Caregivers Act of 2025," Congress.gov, https://www.congress.gov/bill/119th-congress/senate-bill/1565?.
- "S.1227–ABC Act," Congress.gov, https://www.congress.gov/bill/119th-congress/senate-bill/1227.
- "S.3766–Connecting Caregivers to Medicare Act of 2024," Congress.gov, https://www.congress.gov/bill/118th-congress/senate-bill/3766. Note this bill has not been reintroduced yet in the current 119th Congress.
- "Support Family Caregiver Integration: Tools for Healthcare Delivery," AARP, https://www.aarp.org/caregiving/medical/healthcare-professionals/.
- "APTA Practice Advisory: CPT Codes for Caregiver Training Without the Patient Present," American Physical Therapy Association, March 28, 2024, https://www.apta.org/contentassets/44f3909dba914ba1a3c92ab0090492b2/apta_practice_advisory_caregiver_training_codes.pdf; "Medicare and Medicaid Programs; CY 2025 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Prescription Drug Inflation Rebate Program; and Medicare Overpayments," Federal Register, December 9, 2024, https://www.federalregister.gov/documents/2024/12/09/2024-25382/medicare-and-medicaid-programs-cy-2025-payment-policies-under-the-physician-fee-schedule-and-other.
- "Guiding an Improved Dementia Experience (GUIDE) Model," Centers for Medicare & Medicaid Services, https://www.cms.gov/priorities/innovation/innovation-models/guide.
- "Guiding an Improved Dementia Experience (GUIDE) Model."
- "AARP Family Caregiving Guides," AARP, https://www.aarp.org/caregiving/prepare-to-care-planning-guide/.
- "AARP's Family Caregiver Resource Guides," AARP, https://www.aarp.org/caregiving/care-connect/resources/.
