A 60-year-old woman living with chronic conditions such as asthma, polymyositis, rheumatoid arthritis and depression sought emergency care due to worsening shortness of breath. Following her discharge from the emergency department, she continued to struggle with her symptoms while also navigating significant barriers to recovery, including food insecurity, lack of transportation and the need for home-based medical support.
However, through Maryland's Total Cost of Care (TCOC) Model,1 the woman changed the course of her condition, leading her on a road to health and recovery through whole-person care that bridged her clinical and social needs. She is not being identified by name to respect her privacy.
The TCOC Model operates under a unique Medicare waiver that began in 2019, in which Maryland assumes the full financial responsibility for the total cost of care for Medicare beneficiaries. The Total Cost of Care Model establishes global budgets for hospitals, providing predictable revenue streams while simultaneously creating accountability for managing the total cost of care for their populations.2 For Catholic hospitals, with their long-standing commitment to serving the poor and vulnerable, the model's support of integrated care allows the opportunity to align financial incentives with their core values of compassion, justice and community service.
CHARTING A COURSE TO MORE HOLISTIC CARE
The Health Services Cost Review Commission serves as the central regulatory body of the model, setting hospital budgets and monitoring performance against cost and quality targets. Each hospital receives an annual global budget that covers all inpatient and outpatient services, fundamentally changing the financial dynamics of health care delivery.
Unlike traditional reimbursement models that pay for each service provided, global budgets create incentives for efficiency and population health management. Hospitals that successfully manage their attributed populations within budget while meeting quality standards can retain savings, while those that exceed their budgets face financial penalties.3
Unlike traditional fee-for-service models that reward volume, this waiver allows Maryland to assume complete financial risk for Medicare beneficiaries' total health care costs across all settings and providers.4 In the model's first years, from 2019-2021, Maryland generated more than $689 million in excess Medicare TCOC savings.5
A unique and innovative initiative of the TCOC Model is the development of the Maryland Primary Care Program (MDPCP).6 This program serves Medicare patients and places an emphasis on the utilization of their primary care services. Through voluntary participation by primary care providers, funding is awarded to support the delivery of advanced primary care to a vulnerable population. The MDPCP provides hospitals with flexible funding that allows for the creation of resources and support that give primary care providers the ability to have a deeper role in the prevention and management of chronic diseases, and thus yields a reduction in hospitalizations.7
The TCOC Model's success suggests that the future of health care lies not in choosing between mission and margin, but in creating systems where serving the common good and achieving financial sustainability are mutually reinforcing goals.
The model includes specific requirements for care coordination services, including nutrition counseling, pharmacy services, behavioral health integration and health education. These requirements recognize that effective health care delivery requires addressing patients' comprehensive needs, not just their immediate medical conditions. Hospitals must demonstrate meaningful engagement with community partners and show measurable improvements in care transitions and patient outcomes.8
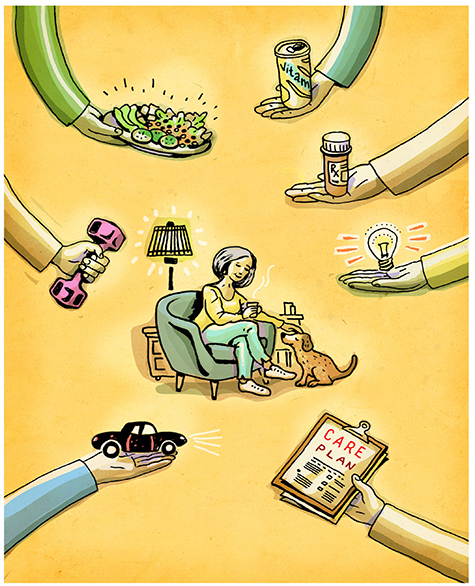
Through Maryland's comprehensive care coordination model, the patient with multiple chronic conditions was promptly connected with services, including home health care, the Moveable Feast meal program for Marylanders, and durable medical equipment like an oximeter and rollator. Care managers accelerated her primary care follow-up, provided emotional support, assisted with Maryland Transit Administration Mobility services, and ensured she had access to physical and occupational therapy.
SUPPORTING MISSION-DRIVEN CARE
For Catholic health care organizations, the TCOC Model offers a unique opportunity to align financial incentives with their fundamental mission of serving those most in need. Catholic hospitals have historically struggled with the tension between their commitment to providing charity care and the financial pressures of operating in a fee-for-service environment. The TCOC Model resolves this tension by creating financial incentives that support rather than penalize mission-driven activities.
Perhaps most significantly for mission-driven organizations, the TCOC Model includes explicit incentives for reducing health care disparities and improving access for vulnerable populations. The model measures and rewards reductions in disparities between different racial and ethnic groups and improvements in outcomes for patients living in high-poverty areas. Early results have shown promising reductions in disparities. Gaps in unplanned readmissions, preventable admissions and timely follow-up care narrowed by a range of 26% to 40% between Black and white beneficiaries.9
Maryland's experience with the TCOC Model has important implications for health care transformation efforts nationwide. Last year, the Centers for Medicare & Medicaid Services announced plans to expand similar models to other states through the AHEAD (States Advancing All-Payer Health Equity Approaches and Development) Model,10 suggesting that Maryland's innovations would become more widely adopted.
A PROACTIVE APPROACH TO HEAL AND SERVE
The TCOC Model's success suggests that the future of health care lies not in choosing between mission and margin, but in creating systems where serving the common good and achieving financial sustainability are mutually reinforcing goals. For Catholic health care organizations and other mission-driven providers, this represents not just an opportunity for financial success but a pathway to more fully realize their fundamental calling to heal and serve.
For the 60-year-old Ascension St. Agnes patient, this approach meant she received medication reconciliation and proper inhalers, and she adhered to her care plan, remaining safely at home without any hospital readmissions. Her successful recovery illustrates how Maryland's all-payer, value-based health care model supports patients far beyond episodic treatment. Unlike fee-for-service systems that often end care at discharge, Maryland's model integrates medical, social and behavioral support services to address root causes and reduce readmissions.
The proactive, wraparound care received — ranging from timely follow-up to transportation and nutritional support — demonstrates how coordinated care under the Maryland model leads to better outcomes, enhanced independence and more efficient use of health care resources.
For Ascension Saint Agnes Hospital in Baltimore, MITCH LOMAX is chief financial officer. TREVOR BONAT is chief mission integration officer. OLIVIA D. FARROW is vice president of external affairs. LAURETTA OSOMIHA, a nurse and case manager, contributed information for this article.
NOTES
- "Maryland Total Cost of Care Model," Centers for Medicare & Medicaid Services, https://www.cms.gov/priorities/innovation/innovation-models/md-tccm.
- "Maryland Total Cost of Care Model."
- "Hospital Rate Setting: Successful in Maryland but Challenging to Replicate," Healthcare Value Hub, June 1, 2020, https://www.healthcarevaluehub.org/advocate-resources/publications/hospital-rate-setting-promising-challenging-replicate.
- "The Maryland Model," Maryland Hospital Association, https://mhaonline.org/wp-content/uploads/2024/06/mha-maryland-model-value-graphicdb8ede355f24402c9499fb957022b01c.pdf.
- "Maryland Total Cost of Care Model: Evaluation of the First Four Years (2019–2022)," Centers for Medicare & Medicaid Services, https://www.cms.gov/priorities/innovation/data-and-reports/2024/md-tcoc-1st-progress-rpt-aag.
- "Maryland Primary Care Program," Maryland Department of Health, June 2021, https://health.maryland.gov/mdpcp/pages/home.aspx.
- "Maryland Primary Care Program."
- "Maryland Total Cost of Care Model: Evaluation of the First Four Years (2019–2022)."
- "Maryland Total Cost of Care Model: Evaluation of the First Four Years (2019–2022)."
- "States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model," Centers for Medicare & Medicaid Services, https://www.cms.gov/priorities/innovation/innovation-models/ahead.
Questions for Discussion
Ascension Saint Agnes Hospital authors Mitch Lomax, Trevor Bonat and Olivia D. Farrow describe ways in which the Total Cost of Care Model offers a unique opportunity to align financial incentives with the fundamental mission of serving those most in need. They describe ways it allows for care coordination.

- This program operates through a unique Medicare waiver. What lessons can be learned from this approach, including for those who live in other states?
- Do you work with anyone or glean helpful information from an author or thinker who advocates for health care transformation in a way that makes considerable sense to you? Who?
- What significant changes might be needed to create "systems where serving the common good and achieving financial sustainability are mutually reinforcing goals," as the authors write of the Maryland model?
- Reflecting on the mission, vision and values of your organization, how do you see the Maryland program as a creative way to reimagine health care and services to the most vulnerable in your community?
