As a cardiologist in the Philadelphia area, Dr. Peter Kowey treated countless patients over the decades for different heart ailments. So, he wasn't surprised when he received a call from one of them. What was surprising was that the patient was asking him about her hip replacement surgery. She was in extraordinary pain and had gone in to see her surgeon for a follow-up appointment.
"The surgeon came in and said, 'This device is broken. We're going to have to replace it,' and then he walked out, leaving her with a gazillion questions," said Kowey. Totally frustrated and unable to get her questions answered, she called Kowey, knowing he would take the time to explain everything to her.
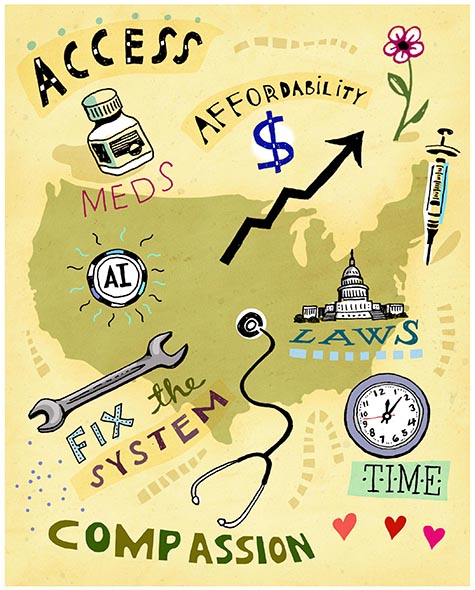
As anyone enmeshed in the world of health care will share, doctors are under increasing pressure to see more patients but for shorter amounts of time, often to bolster the bottom line. Compounding this and other pressures is the uncertainty around the future of the health care landscape with the July 4, 2025, passage of the One Big Beautiful Bill Act (OBBBA). One aspect remains certain: The health care system has a lot of work to do to make care more accessible, affordable and beneficial to everyone, especially given the constraints of the new law, with many pieces of the legislation going into effect in 2026. The Congressional Budget Office is projecting OBBBA to cause around a $1 trillion reduction in federal health care spending through 2034 and increase the number of uninsured people by 10 million.1
As health care continues along this uncertain path, there are many issues that need to be addressed.
CHAIN REACTION
For doctors to do their jobs well and for patients to get the answers they need, something has to give, according to Kowey, a professor of medicine and clinical pharmacology at Thomas Jefferson University in Philadelphia who recently authored the book Failure To Treat: How a Broken Healthcare System Puts Patients and Practitioners at Risk. Otherwise, very few doctors can give the attention and care necessary to fully address patients' concerns and symptoms.
"We're stacking the patient schedule every 15 to 20 minutes per patient, and the patients suffer, of course, because they don't think that they have enough time," said Kowey. "By the time the technician puts the patient in the room and gets a cardiogram and vital signs, we're halfway through the visit. So, part of the problem is that even when you get in, you don't necessarily have a satisfactory visit, or that you don't walk out feeling like you got what you needed."
It isn't just patients feeling unsatisfied. Due to myriad pressures, physicians are walking away or retiring earlier than planned. In a recent MedCentral survey, more than one-third (35%) of physicians said they have considered leaving the medical practice since the start of 2025. Top reasons cited include personal burnout, early retirement and clinical demands.2 If the current situation continues, the U.S. can expect a physician shortage of up to 86,000 physicians by 2036, according to the Association of American Medical Colleges.3
EVERYONE LOSES
One area that needs to be addressed is the haphazard approach to health care in the U.S., according to Dr. Jeff Salvon-Harman, CPE, CPPS, vice president of safety for the Institute for Healthcare Improvement (IHI). "In the U.S., we have not done a great job at keeping people from becoming patients," he said. "As a result, what we're seeing that is affecting hospitals is patients with four or five chronic, comorbid conditions that impact each other, such that when any one of them causes an acute complication, the multiple others that are in the background are also being impacted. We have to do a better job in communities, in ambulatory care, in primary care, not only delivering care, but creating safer environments for people, so that people don't have to become patients."
In 2023, approximately 76% of U.S. adults reported one or more chronic conditions, and about 51% reported multiple chronic conditions. That number jumped to nearly 79% for older adults, according to the Centers for Disease Control and Prevention.4
A more strategic approach needs to be taken, according to Salvon-Harman. "Part of what we have to acknowledge is that the health care system that we have today did not come to be through intentional design. Nobody convened a committee or a working group or a task force to say, 'Let's design perioperative care for the whole country. Let's design primary care for the whole country. Let's design specialty care, inpatient and outpatient for the whole country.' Every health system has pulled together, starting out with individual hospitals becoming multiple hospitals, and then becoming a large organization. They've adapted and adopted and added as they needed to for their business models or as care paradigms changed."
SHIFTING FROM INPATIENT TO OUTPATIENT
At New Jersey's Saint Peter's Healthcare System, President and CEO Leslie Hirsch is seeing the shift from inpatient to outpatient visits that many hospitals across the country are experiencing. Medical procedures that, in the past, would have required multiple days in the hospital, such as hip surgery, can now be done as a one-day appointment for otherwise healthy patients.
While the advancements in technology that make this possible are, as Hirsch describes, "incredible," it has also meant that insurers want to pay less wherever they can. "The role that insurers play in pre-authorization and denials for consumers and then for providers has resulted in an extremely complex and frustrating system for both consumers and providers," said Hirsch. Even if a patient stays in the hospital for multiple nights, but insurance classifies them as "observation status," they are still considered an outpatient. That means insurance pays a fraction of what it would have paid had it been an inpatient visit, yet the patient is receiving the same level of care and services, and the hospital is using just as many resources and staff. "What's going to happen is the payer, the insurance company, is going to deny us payment on that, and then we're going to have to appeal," he said. Hospitals end up having to leave millions of dollars on the table because of this. "It's just this is the game that insurers play," said Hirsch.
PROCEED WITH CAUTION
Technological advances have saved many lives and a lot of time, but they must be carefully implemented, according to Salvon-Harman. Many manual surgeries and open surgeries have become laparoscopic and are now becoming robotic. "Those kinds of changes happen over time. None of that was intentional. Nobody said, 'We need to have a robot to do surgeries, because it'll be better than laparoscopes and open surgeries.' The technology evolved and emerged, and we said, 'Yes, we could use that because that looks like it's better, that might be more effective, that might be more consistent [for some surgeries].'"
As a result of the way our health system has evolved, there are a lot of inconsistencies. "When you move across one organization to another, sometimes even within the same parent organization, different sites of care may be doing things differently. And so, we're always trying to balance the structures, the processes and the culture of the large parent organization, but also each and every one of the individual sites of care, whether a hospital or an outpatient practice," said Salvon-Harman. "So, there's still a lot to do around achieving those higher levels of consistency and, in some cases, being in sync with other parts of the system. Technology holds some promise in closing some of those gaps, moving us in that direction, but it hasn't yet done it completely successfully."
Many of the new technologies are intended to help us "work smarter, rather than harder, and are supposed to increase the efficiency or the effectiveness of what we do," said Salvon-Harman. But we need to be cognizant of the ways they introduce additional complexity. "They have a learning curve for how to use them optimally. They have various influences, like what we call human factors: how the human interfaces with that piece of equipment or that technology that may introduce risk at the same time that it is eliminating other risks."
EMBRACING, INVESTING IN INNOVATION TO COMPETE
At the same time, we are at a point when new technologies must be embraced, as they can keep health care moving forward and are what many patients have come to expect, according to Yunan Ji, an assistant professor of strategy with a focus on the design and regulation of health care markets at the Georgetown University McDonough School of Business. With more transparent pricing than in the past, health care organizations also need to find effective ways to communicate "nonprice attributes," such as clinical outcomes and patient experience, in ways that resonate with consumers who are making choices about where to receive care.
"This shift also reflects a broader transformation toward a more digital, consumer-oriented health care ecosystem — accelerated by the rise of telemedicine, on-demand care and virtual-first models. Just as consumers have come to expect seamless, intuitive digital experiences in sectors like retail and banking, they now bring those same expectations to health care, particularly for elective services, outpatient care and administrative interactions," Ji said. "Hospitals and health systems that invest in modern, user-friendly digital platforms — ranging from online scheduling and virtual visits to personalized cost estimators and mobile engagement tools — will be better positioned to attract and retain patients. In a competitive environment where convenience, transparency and digital experience matter more than ever, digital maturity is becoming a key differentiator for providers."
INTEGRATING AI
At Bon Secours Mercy Health, one of the goals is to make health care easier for patients and for consumers. In 2024, Bon Secours Mercy Health launched a conversational, artificial intelligence (AI)-powered digital guide called "Catherine," (named in honor of Catherine McAuley, the founder of the Sisters of Mercy) aimed at transforming how patients access information and resources when they have knee, hip and shoulder pain.5
"In a competitive environment where convenience, transparency and digital experience matter more than ever, digital maturity is becoming a key differentiator for providers."
— Yunan Ji
"Conversational AI represents the modern era of patient engagement," said David Cannady, Bon Secours Mercy Health's chief strategy officer. "It's time to offer a solution that goes beyond what patients can currently access in Google searches or on social media platforms." In addition, the health system is working toward same-day access for patients, which Cannady believes will be driven by AI and automation. "We utilize AI to help patients access the right care at the right time by simplifying the process, from appointments and scheduling to finding the appropriate provider for their health needs, whether preventive or acute."
WAITING AND WATCHING
Leaders at Bon Secours Mercy Health are watching several legislative and regulatory discussions that could have a potential impact on patient care and the providers of that care, said Cannady. "Key topics include Medicaid and Affordable Care Act Exchange enrollment eligibility and other proposed reductions," he said. "Should enrollment and public program reimbursement decline, health systems might face decisions such as the rationing of services to sustain a viable community-based model of care. In some cases, unfortunately, there may be closures of service lines or even hospitals in rural and other communities."
For IHI's Salvon-Harman, it means thinking about new delivery paradigms, new ways to identify what is meaningful. "Is it better for a patient to have a 15-minute appointment monthly, three months in a row? Or is it better for that patient to have 45 minutes with their health care provider one time in three months but get a much more substantive dose of health care in that 45-minute appointment?" he asked. "Do we need to think about how we acquire information in the health care setting, and how we process information? Do the standard tools for a history and physical examination that have been taught for over 100 years and used for over 100 years still serve the purpose?"
He suggests we look at adapting those models and collecting information differently so we can analyze that information, and we can apply the thinking from that analysis to each patient. "I feel like that's really where we're at now in ambulatory care: needing to really question the models we've been using and their effectiveness, and identifying and testing new models to see if they enhance our ability to diagnose more accurately, more timely," said Salvon-Harman. "And to better coordinate across different specialties more efficiently and effectively, creating venues for more cross talk in real time, across specialties and across providers, leveraging AI and leveraging virtual technology to support better information sharing closer to real time. I think those are a lot of the opportunities that are emerging but haven't yet been successfully harnessed."
There are also error and human factors, according to Thomas Jefferson's Kowey. While AI and technology can help, they can't replace human judgment. "We're not dealing with widgets here. We're dealing with biological organisms with feelings, with emotions, with expectations, with fear and anxiety," he said.
Everything comes down to making systemic changes, according to Kowey, who was motivated to write his book by the "tremendous number of problems" in the U.S. health care system. "As the title says, it's broken. It's impacting both the quality of patient care and the well-being of providers. Burnout is real. But I truly believe it doesn't have to be this way," he said. "It's a call to action for patients, legislators, administrators and providers. We still have options, but not a whole lot of time. If things keep going the way they are, we may lose the quality of care we've come to expect, possibly for good."
ELIZABETH GARONE is a freelance writer who has covered health, business and human-interest topics. Her writing has appeared in The Wall Street Journal, The Washington Post, BusinessWeek and The Mercury News, among other publications.
NOTES
- "Health Provisions in the 2025 Federal Budget Reconciliation Law," KFF, August 22, 2025, https://www.kff.org/medicaid/health-provisions-in-the-2025-federal-budget-reconciliation-law.
- Marcia Frellick, "Survey Shows One-Third of Physicians Considering Leaving Medicine," MedCentral, June 17, 2025, https://www.medcentral.com/biz-policy/survey-shows-one-third-of-physicians-considering-leaving-medicine.
- "The Complexities of Physician Supply and Demand: Projections From 2021 to 2036," Association of American Medical Colleges, March 2024, https://www.aans.org/wp-content/uploads/2024/05/aamc-2023-workforce-projections-report.pdf.
- Kathleen B. Watson et al., "Trends in Multiple Chronic Conditions Among U.S. Adults, by Life Stage, Behavioral Risk Factor Surveillance System, 2013–2023," Preventing Chronic Disease 22 (2025): http://dx.doi.org/10.5888/pcd22.240539.
- "Mercy Health Cincinnati First to Launch AI Powered Digital Assistant," Mercy, December 20, 2024, https://www.mercy.com/news-events/news/cincinnati/2024/mercy-health-cincinnati-first-to-launch-ai-powered-digital-assistant.
