The days immediately after hospital discharge were so much worse health-wise for Ashley Kathman three years ago when she delivered her son Brooks than this past January when she delivered her daughter Camille.
Kathman had preeclampsia in both pregnancies and related high blood pressure post-delivery. But three years ago, her high blood pressure drove her to the emergency room on multiple occasions. This year was completely different.
Kathman's obstetrician-gynecologist Dr. Leizl Sapico knew Kathman was at risk for high blood pressure and connected her with a program that educated her about her condition and what to do when her blood pressure spiked or plummeted. Also, this time, Kathman used a blood pressure cuff every morning and evening that transmitted her vitals to a nurse. That nurse would follow up with Kathman if the numbers were concerning. Kathman also had around-the-clock access to clinicians by phone, including through messaging. Kathman called several times when her blood pressure was abnormal to ask what to do.
"I would have gone to the emergency department if I hadn't been able to call and receive quick correspondence for peace of mind," says Kathman. An emergency department visit would not only have been scary, she says it would have been difficult to manage, especially if she had a toddler and newborn in tow.
With the support from St. Anne Hospital in Burien, Washington, Kathman successfully managed her blood pressure, was able to wean off her blood pressure medication within a month of starting it, avoided the emergency department and, most importantly, suffered no ill health effects from her condition.
The postpartum health program "made a huge difference, it was amazing," Kathman says. "It should be the standard of care for every mom."

Postpartum safety net
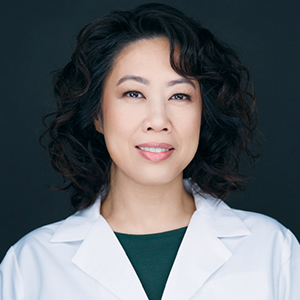
Sapico developed the postpartum wellness program and implemented it at Virginia Mason Franciscan Health, which is part of CommonSpirit Health. Virginia Mason Franciscan Health has facilities in northwest Washington. Now in place at Virginia Mason Franciscan Health 's St. Anne Hospital, the Postpartum Wellness and Recovery Program, or PWR, includes nurse navigation, health and wellness education, health monitoring, and care referrals for new moms who are vulnerable to the most dangerous postpartum diagnoses.
Currently, the program focuses on women identified to have hypertension or who screen for perinatal mood and anxiety disorders. This summer, the program also will support women at risk for gestational diabetes.
"We've now created a safety net for when new moms leave the hospital," Sapico says.
'We have to do better'
Statistics show that the United States' maternal mortality rate has more than doubled in the last two decades and is now worse than for most other high-income countries. The Centers for Disease Control and Prevention says that maternal mortality rates are significantly worse for Black women than for white, Hispanic and Asian women.
Sapico says statistics show that most cases of maternal morbidity and mortality that occur in the postpartum period are preventable.
"We have to do better in taking care of moms," she says.
Capstone project
Sapico has been an obstetrician-gynecologist at Virginia Mason Franciscan Health since 2014.

Her work to get at the top causes of harm for new moms began in earnest when she was pursuing her master's in organizational leadership at Gonzaga University in Spokane, Washington, in 2021. As her capstone project, she came up with the idea for the program to identify women in danger of postpartum clinical and mental health concerns and provide them with in-depth support. She launched the PWR program at Virginia Mason Medical Center in Seattle and recently transitioned it to St. Anne. The program is in pilot phase. In time, Sapico plans to create a toolkit so that other CommonSpirit facilities can launch their own iterations.
Women do not have to be patients of Virginia Mason Franciscan Health facilities to take advantage of the PWR program, but most who do are.
Navigation
Sapico has been rolling the PWR program out in phases, with hypertension navigation first in 2023, and the perinatal mood and anxiety disorders navigation second in 2024. In July, she'll add on navigation for gestational diabetes.
Building out the program has involved many steps, including garnering the support of leadership and clinicians, securing grant funding, hiring a full-time nurse navigator, and deepening connections and establishing referral relationships with clinicians. This includes both clinicians who can direct patients to PWR as well as those who can treat PWR clients.
As the program grows, Sapico hopes to add more staff, including perhaps a social worker or community health worker.

For hypertensive moms like Kathman, PWR's full-time perinatal nurse navigator Lacey Parsadmehr gets a referral and visits them before discharge. She talks with them about hypertension and its signs and symptoms, educates them on the basics of self-care and tells them about the benefits of PWR. Those who sign on to receive Parsadmehr's no-cost services get a device so their blood pressure can be monitored remotely. They get check-ins for six weeks, a warm handoff to their primary care clinician and ongoing navigation services from Parsadmehr.
That navigation includes continual education on their condition, help using home health equipment, assistance scheduling follow-up appointments with doctors, support with any socioeconomic concerns, and other help for a year after the baby's birth.
For women who screen at risk for perinatal mood and anxiety disorders, Parsadmehr takes a similar approach but one tailored to mental health aid.
Lifesaving intervention
Key goals of the program are to prevent maternal mortality, improve maternal health outcomes, and reduce hospital readmissions of postpartum women. Sapico says while there are systems in place to gather data to measure these and other impacts of PWR and to prove its value, the program is too new to have solid evidence of its impacts yet. However, she and Parsadmehr say they already are seeing much anecdotal evidence of the benefits.
Sapico and Parsadmehr say patients have said PWR saved their lives.
Sapico says that mental health concerns are some of the most threatening conditions for new moms. PWR seeks to reduce the stigma around new moms' mental health. This includes ensuring moms know, through PWR efforts, that it is OK to express that they are feeling anxious, depressed or overwhelmed — and to get help coping — at a time in their life when society may be saying they should only be feeling joy about their new baby.
Parsadmehr notes that in addition to addressing mental health concerns, PWR has provided much-needed assistance with financial and language barriers. She says these barriers can be extremely taxing for new moms, and PWR's help with navigating social services and accessing translation services has been invaluable to those moms.
Sapico says often when a woman gives birth, so much attention is on the baby, and so much of the woman's own time and energy is focused on the baby, that she can neglect her own health. PWR shifts attention back to the mom's health, and ensures that she is seen and heard. Parsadmehr says she loves that she and Sapico are educating patients, helping them make life choices that will have a lasting benefit, and encouraging them to advocate for themselves.
Sapico says, "Imagine how much death can be prevented, and how much healthier our patients can be if we push for better outcomes. That's what drives this work — we just want healthier outcomes."
Further reading: SSM Health's Wisconsin hospitals give new moms alert bracelets to flag them as at-risk
