
The neonatal intensive care unit can be a very challenging place for babies, their families and even the unit's staff.
Most of the babies are fragile, with a precarious health status, and struggling to meet developmental milestones. Oftentimes parents are frightened about their babies' status and prognosis. The staff can be physically, mentally and emotionally taxed as they tend to the vulnerable neonates.
A new music therapy program in the NICU of Providence Cedars-Sinai Tarzana Medical Center in California is helping to address such concerns in a low-intervention, evidence-based way.
Music therapist Jenna Marcovitz helped establish the program this summer and now runs it. She says music brings a human component to what can feel like a very medicalized and foreign environment. "Music normalizes the environment," she says. "We're celebrating the family, and promoting the family's bonding. Families can feel nervous, but we provide a safe space for them. They can sing, hold their baby and celebrate their connection."
She adds, "Music can have an immediate positive effect on the nervous system" of the babies, their families and staff.
"It's feel-good hormones for everyone!" she says.

Benefactor of pediatric patients
The music therapy program at Cedars-Sinai Tarzana's NICU began with the support of two longtime donors. Robin and Susan Richards created the Chase Foundation in 1992 in remembrance of their son Chase, who died of cancer as a toddler. To help pediatric patients manage the effects of stress and trauma while hospitalized, the foundation funds child life programs at Cedars-Sinai Tarzana and other hospitals. Child life specialists are trained to help young patients gain a sense of familiarity and control of their environment through play and exploration.
Marcovitz is a music therapist at multiple health care facilities in Southern California. Using a two-year, $100,000 gift from the foundation, she designed the program in which music therapist Audrey Creevey visits Cedars-Sinai Tarzana's 21-bed, level 3 NICU most Fridays. The hospital is part of Providence St. Joseph Health.
'Feeders, growers'
Creevey can provide music therapy to support babies at almost any age and level of acuity and at almost any point in their time in the NICU. For babies whose health is so tenuous that most music can be overstimulating and do more harm than good, Creevey can tailor the interventions to meet the need. For instance, simply humming quietly outside the closed incubator may be a good starting point, and interventions can be increased over time, if warranted.
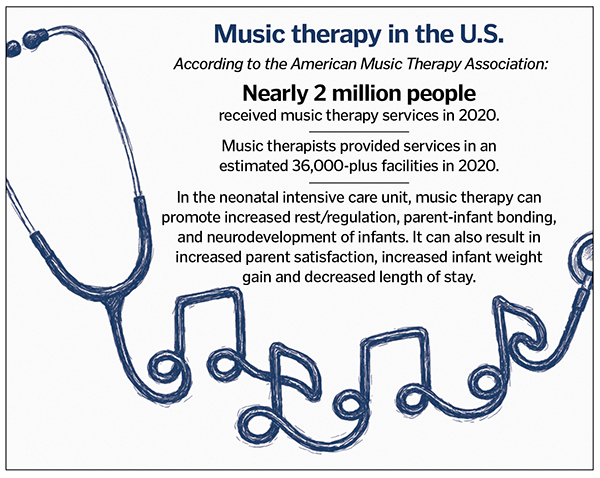 Music therapy can be very effective too for babies who are stable and preparing to transition to home. Creevey explains that these "feeders, growers," as they are affectionately called in the unit, need to sleep, eat and grow so they can hit the developmental milestones to be discharged safely.
Music therapy can be very effective too for babies who are stable and preparing to transition to home. Creevey explains that these "feeders, growers," as they are affectionately called in the unit, need to sleep, eat and grow so they can hit the developmental milestones to be discharged safely.
Marcovitz explains, "We provide a holistic approach. It is nonpharmacological relief of symptoms as well as developmental support."
During her Friday visits, Creevey brings a guitar with nylon strings — research has shown this to be a superior instrument for achieving therapeutic benefit. Upon arrival she speaks with the charge nurse or other clinicians on the unit about who to prioritize.
She then meets with each family — or sometimes visits the baby alone, if permission has been granted — incorporating different music therapy techniques based on the need. She plays lullabies or rhythmic patterns, or leads parent-involved musical activities. Sometimes she'll ask parents what songs have special meaning to them — so-called songs of kin. These can include songs that have a personal significance to the parents, songs they listened to while the baby was in utero, or songs that speak to their experiences. Sometimes Creevey will personalize songs for the family. She also provides psychosocial support, helping the families process their feelings about their experiences with their babies in the NICU.
Creevey also can play music in a way that promotes sleep or that promotes "entrainment," which is the process babies use to breathe, swallow and suck. She notes that this process is not always natural for newborns and must be learned. Certain musical rhythms can guide the babies along the process.
Monitoring impact
Creevey, who just recently earned her music therapy certification and completed an internship, has learned to watch the babies' vital signs and their bodily responses to know how to modulate the music. Sometimes a baby will "shoot up a limb," which tells her the music is too stimulating.
Marcovitz is building evidence-based measures into the program. In time, Creevey and the clinical team are checking the babies' heart rate, oxygen saturation rate and respiration rate before and after the musical intervention. The team also are noting observable physical responses, such as muscle relaxation, as well as feeding and sleeping success.
Marcovitz anticipates the evidence will show the benefits. She hopes that will inspire more financial support so this pilot program will be made permanent. She would like to expand music therapy to other patient populations at Cedars-Sinai Tarzana, including women and children. She notes that financial sustainability is a concern for music therapy in general since there is no reimbursement stream for it.

Win win
Dr. Roxanne Arcinue is the Cedars-Sinai Tarzana NICU medical director, vice chief of its department of pediatrics and an attending neonatologist. She says the music therapy program aligns well with the philosophy of the hospital's NICU, which seeks to provide family-centered care and to use the least amount of intervention possible to achieve care goals. She notes that music therapy has become another tool that can help prepare NICU patients for a successful transition home.
She mentions that music therapy also can be helpful for babies who are born to mothers addicted to illicit substances. These babies often must go through withdrawal therapy. They can be highly agitated during this process. The music has helped to calm them.
Marcovitz, Creevey and Arcinue say they already are seeing a beneficial impact from the program. Arcinue says the music therapy is reinforcing the parent-baby bond and empowering parents. Marcovitz says nurses and other staff are reporting a feeling of peace as they hear the music in the unit. "It's a win-win, the music has an immediate positive effect on the nervous system, it provides relaxation and a positive emotional response" for babies, their families and staff, Marcovitz says.
Creevey says: "My favorite part of being a music therapist at Cedars-Sinai is meeting and connecting with the families and building the relationships. I learn about them and their lives, and I feel like I am a part of their lives."
Read about a similar music therapy program at PeaceHealth Southwest Medical Center in Vancouver, Washington, here.
