
When she picked up a nursing student earlier this year at the end of an educational rotation at the St. Anne Home eldercare facility in Greensburg, Pennsylvania, Helen K. Burns says the young woman walked out beaming.
"What the student told me is that she really believed it was positive for her learning, and her presence was positive for the patients' health and well-being as well," says Burns, a professor and the inaugural chair of the Department of Nursing at Saint Vincent College. "They understood she was a student, but they were so gracious to talk with her, to help her learn, answer her questions, and to accept her presence there with them as a caregiver."
The student's experience was part of a partnership between Saint Vincent, a Catholic liberal arts and sciences college in Latrobe, Pennsylvania, and St. Anne Home. Their pairing is under the umbrella of the Pennsylvania Teaching Nursing Home Collaborative, a growing initiative focused on improving nursing home resident care, nursing student education, and nursing faculty support.
The initiative provides:
- Webinars and a library of resources including sample meeting agendas to help nursing homes and schools of nursing start or strengthen partnerships
- Guidance on improving eldercare and gerontological nursing education through a network of peers and educators
- Exposure for nursing students to careers in eldercare
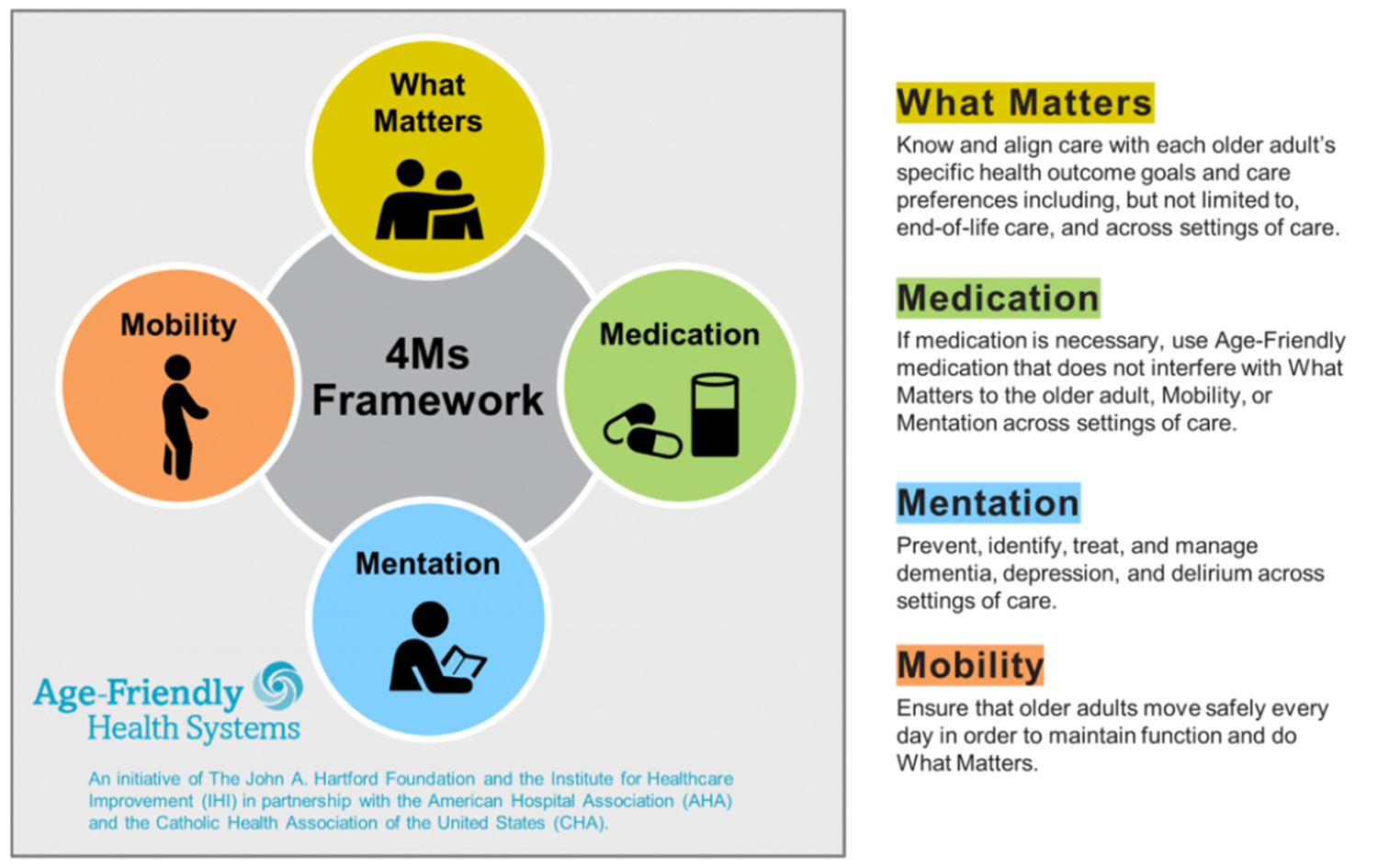
- Support to implement the Age-Friendly Health Systems framework, a set of practices designed to align care for older patients with what matters to them
The collaborative was piloted from 2021 to 2023 with four nursing homes and three schools of nursing. Those partnerships led to 677 nursing staff trained in Age-Friendly care, 591 nursing home residents receiving Age-Friendly care, 510 students completing clinical rotations in nursing homes, 40 nursing educators engaged in the initiative, and the curation of 89 guides, a textbook and other resources to support nursing practice and leadership in nursing homes. The pilot proved so successful that the collaborative launched a second phase in 2023 and now encompasses more than 70 nursing homes and more than 20 schools of nursing across Pennsylvania.

Reviving an old model
Jane Carmody is a senior program officer at The John A. Hartford Foundation, a nonprofit dedicated to improving the care of older adults that is one of the founders and funders of the collaborative. She says the collaborative's roots are in a teaching nursing home model that was funded in the 1980s by the Robert Wood Johnson Foundation, a philanthropy focused on improving health. That model created partnerships between nursing homes, schools of nursing, medical schools and social work schools. Patients at homes that adopted the model were among its beneficiaries because rates of heavy sedation, catheterization and restraint decreased, according to a study published in 1995.
In 2021, as the COVID-19 pandemic was ravaging nursing homes and a workforce shortage was setting in, The John A. Hartford Foundation and the Jewish Healthcare Foundation decided to revisit the teaching nursing home model, this time incorporating the Age-Friendly framework developed a few years earlier. In the Age-Friendly framework, caregivers are trained and encouraged to provide holistic patient-centered care around "the 4M's": what medication patients are on, how mobile they are, their mentation or mental acuity, and their view of what matters to them.
Carmody says the 4M's are the "common language" of the partners in the Pennsylvania Teaching Nursing Home Collaborative. "It gives them a solid support to help develop the geriatric curriculum," she says.

Looking forward
The Pittsburgh-based Jewish Healthcare Foundation is another funder of the collaborative. It is also in charge of establishing and coordinating the collaborative's partnerships, with Nancy Zionts, chief program and strategy officer, as the project's principal investigator.
Anneliese Perry, program manager for aging initiatives, and Maureen Saxon-Gioia, nurse project manager, both at the Jewish Healthcare Foundation, also have lead roles in the work. They start new pairings by meeting with leaders from the nursing homes and colleges, explaining how academic partnerships work, and going over the Age-Friendly concepts. Then the two sides craft plans for developing and advancing their partnership.
Perry says leaders of nursing homes that participated in the collaborative's pilot said it gave them hope, especially after the misery and workforce challenges brought on by the pandemic.
"After everything that they went through during COVID, it helped them look forward," she says. "It helped them know that there are people that want to bring new life into long-term care, that want to reach out to schools of nursing to get people to realize that this is an opportunity for nurses to really use that autonomy to be hands-on in the decision-making in the care process."
Saxon-Gioia says the collaborative gives each participating institution flexibility in how they work with their partner and in the goals they set for their teamwork.

As part of their work with the collaborative, she and Perry convene learning sessions for leaders of the institutions and share best practices. "We are so excited about what we're doing now," Saxon-Gioia says. "We are growing, evolving, learning and adapting as we go along."
While the collaborative only pairs nursing homes and nursing schools in Pennsylvania, institutions and groups based elsewhere can join as friends and access its online resources. The collaborative had about 70 such friends by April.
Carmody says the success of the collaborative in Pennsylvania and the interest in it from outside the state are building support for a third phase that expands the collaborative nationwide, but she acknowledges "there's work to get to that point." She notes that the collaborative got its start in Pennsylvania in part because established organizations, such as the Jewish Healthcare Foundation, the Independence Foundation, the Henry L. Hillman Foundation, the Pennsylvania Association of Directors of Nursing Administration and the Pennsylvania Higher Education Nursing Schools Association, championed the program. Similar support would be needed to set up the groundwork for the collaborative in other states.

A growing need
Meanwhile, in Greensburg, Pennsylvania, Director of Nursing Ann Donovan has high hopes for St. Anne Home's pairing with Saint Vincent College. That partnership started last year with discussions between her and Burns. Visits to St. Anne Home by nursing students started this year.
"Anytime you can attract new students to this care setting is really desired because a lot of times individuals entering the nursing profession or doing it as a second career are not necessarily interested in long-term care," Donovan says. "It doesn't seem as flashy or romantic. So, with this, we're encouraged they get to see it in a different light."
Donovan says on-site rotations often change students' views of eldercare. "My favorite thing to hear is 'Wow, it's not what I expected. It's busier,' or 'It's more complex,'" she says.
Not only is participation in the collaborative relatively new for Saint Vincent, so is the college's whole nursing program. It launched last August with a bachelor's track. A master's program starts this summer.
Burns says the college was intentional from the start about covering geriatric care in the nursing curriculum. One goal is to dispel the notion that people in nursing homes aren't vibrant or active and that caring for them might be less exciting than other nursing work.
"We're hoping that by introducing care for the geriatric population early in the curriculum and throughout the curriculum and creating really meaningful clinical placements, the students are going to see the benefit of this as a specialty when they graduate," Burns says.
In Southwestern Pennsylvania, where the college and St. Anne Home are located, Burns says eldercare is increasingly in demand as people over the age of 85 are one of the fastest-growing segments of the population.
"Our geography makes us very aware of this population, and the need to assure that our students understand how to keep elders healthy," Burns says.
