Food insecurity is an intractable and long-standing issue in the U.S., and a concern that Trinity Health is prioritizing throughout its 25-state footprint through its Food Is Medicine strategy. It recognizes that nutritious food is an essential component of overall health, but many people do not understand that connection or they face significant barriers to healthy eating.

Through Food Is Medicine programs, multiple Trinity Health regions address nutrition concerns, in the clinical environment and the broader community. While each Trinity Health facility's particular approach varies based on local circumstances, all of them use some type of patient screening for food security, partnerships with community organizations to address food access issues, education of patients and community members as well as data collection to monitor outcomes.
Dr. Daniel Roth, Trinity Health executive vice president and chief operating officer, is helping to lead Food Is Medicine. "We're educating people on food and lifestyle, and their connection to health … and we're ensuring that they have ways to connect to healthy food in their community," he says. "We're making it easy to do."
He adds, "We know we're saving lives."
A deepening crisis
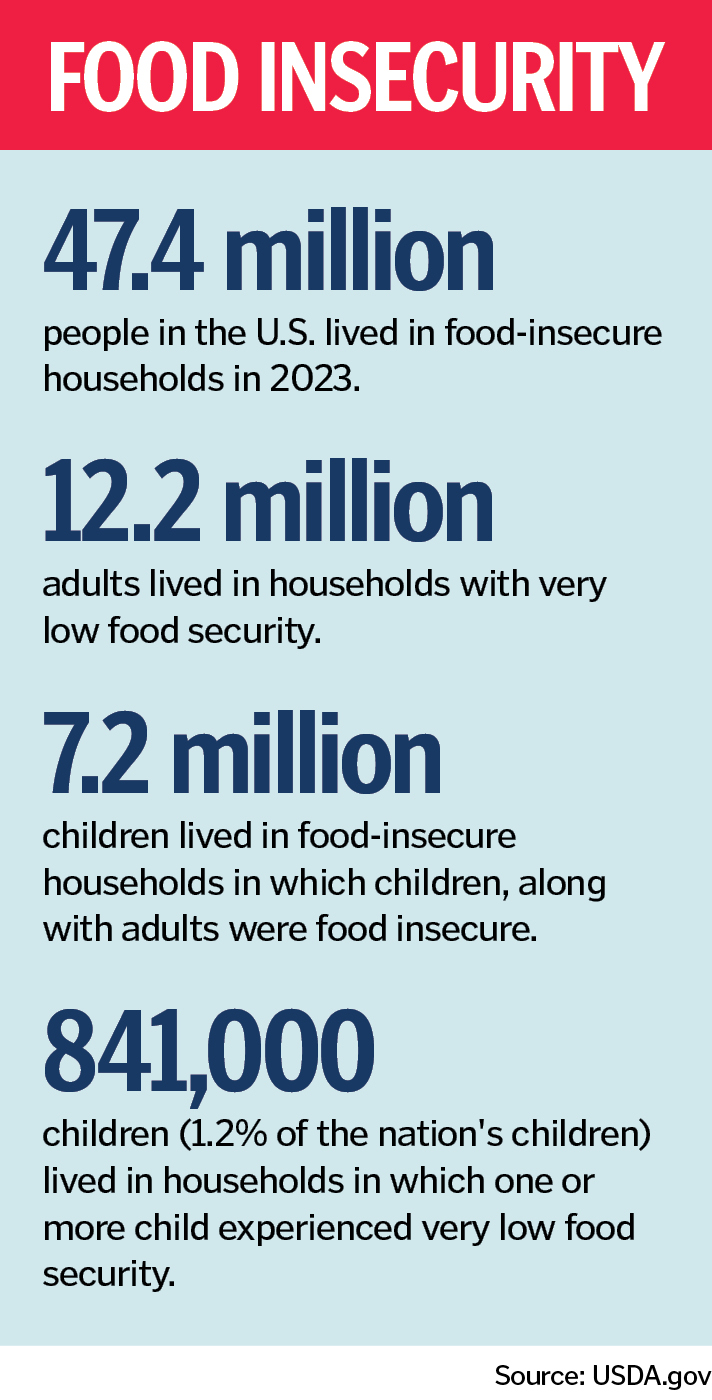
About 47.9 million Americans lived in food-insecure households in 2024, with some minority populations especially at risk, according to an analysis of the December 2025 Household Food Security report from the Department of Agriculture's Economic Research Service.
The report's findings "highlight a crisis that is set to deepen as the deepest cuts to the Supplemental Nutrition Assistance Program in history take effect," the nonprofit Food Research & Action Center said in a release. According to the USDA, an average of about 41.7 million people per month participate in the federal nutrition program, with benefits averaging $187.20 per participant per month.
Food insecurity consistently ranks as a top concern in community health needs assessments from nearly half of Trinity Health's hospitals and their community partners. Trinity Health clinical data shows that food insecurity is a persistent issue for many patients.
Barriers to healthy eating
Roth says food insecurity has two main facets: Can people afford nutrient-rich food and can they buy that food in their area? Many areas that Trinity Health facilities serve lack grocery stores, a persistent and widespread problem.


Sheilah McCart, Eric Stone and Carolyn Alessi are Trinity Health colleagues advancing the Food Is Medicine work in local markets. They explain that numerous barriers can exacerbate food insecurity. The rising cost of living can make it too expensive to buy nutritious food, says McCart, manager of community engagement, community health and well-being at St. Peter's Health Partners in Albany, New York. Some people do not have the transportation needed to travel to stores with healthy foods, says Stone, director, community health and well-being at St. Joseph's Health, Syracuse, New York. Maintaining food access over time can be especially challenging, notes Alessi, regional director of community health and well-being at Trinity Health Of New England.
Whatever the barriers and issues, poor nutrition can have serious — and even life-threatening — implications, says Roth. Unhealthy diet is linked to some of the top health concerns in the U.S., including heart disease, cancer, diabetes, kidney disease and chronic liver disease. An analysis from the nonprofit National Institute for Health Care Management says these types of chronic conditions are among the nation's leading causes of death and account for an overwhelming percentage of health care spending. The institute's analysis says some minority communities are particularly at risk.
Some of the top chronic conditions on Trinity Health regions' radar screens through Food Is Medicine include diabetes, stroke and cardiovascular concerns, including hypertension.
Tools for success
Roth says Trinity Health enables local markets to tailor programming, based on particular needs and resources in each community.
But the regions' work has common aspects. All include both clinical initiatives that apply to Trinity Health patients as well as population health approaches that apply to the broader community. On the clinical side, all are taking advantage of Trinity Health's electronic medical record, which has screening questions on health-related social needs, including food insecurity. All are forging partnerships with community partners, including food pantries and social service agencies. And all are incorporating nutrition education, often from registered dietitians. Multiple regions involve community health workers in their programming. These workers help with coaching, navigation and follow-up, for both Trinity Health patients and community members.
Roth adds that all the programming is grounded in whole-person care concepts, addressing people's needs — body, mind and spirit.
Local iterations
Food Is Medicine programming in some areas Trinity Health serves includes:
- Trinity Health New York: Trinity Health's Albany and Syracuse markets offer the Food Farmacy initiative, which includes 12-week group sessions for patients who have specific chronic conditions and who have screened as food insecure. The participants get food and healthy lifestyle education, help addressing socioeconomic concerns, free healthy food if they need it and help connecting with community partners that can meet identified needs. Both the Albany and Syracuse markets also offer patients and staff members access to on-site emergency food supplies. The Albany program involves community health worker support.
- Trinity Health Of New England: Saint Francis Hospital in Hartford, Connecticut, has made community health workers a central part of its Food Is Medicine work. Saint Francis Hospital engaged a committee of community partners in developing an intervention for people with food insecurity and unmanaged chronic disease. Piloted at the hospital's safety net clinics and then broadened to patients of the primary care practices within Trinity Health Of New England's Medical Group, the program provides intensive support from specially trained community health workers to patients diagnosed with certain chronic illnesses. The community health workers provide education on making healthy choices, coaching on nutrition and help with addressing socioeconomic barriers.

- Trinity Health Michigan: Three Trinity Health Michigan sites — Ann Arbor, Muskegon and Oakland — run Food Is Medicine farm programs on their hospital campuses. These farms provide community-centered food programs and seek to improve health equity while investing in the local food system, according to Trinity Health Michigan. The programming includes the Farm Share program that offers produce boxes and cooking education to community members, the Farm Share Assistance program that provides fresh fruit and vegetables to food-insecure people, and the Produce to Patients program that supplies patients with fresh produce. The farms also supply produce to farm stands and food pantries and for nutrition classes. In the Oakland market, retired emergency department physician Dr. Ross Weinstein recently announced a $4 million estate pledge to expand the farm's work and add a community food hub on the hospital campus.
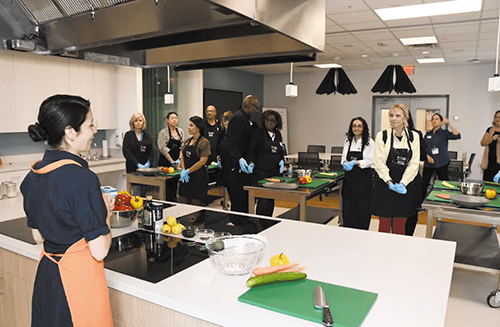
- Trinity Health Florida: As part of a larger body of work, Holy Cross Health of Fort Lauderdale, Florida, hosts an annual Food Is Medicine Symposium. The October 2025 gathering drew more than 100 people — in-person and virtually — to learn how to improve health through nutrition. Sponsored by Holy Cross's community health and well-being department and local partners, the event featured presentations by experts in food policy, nutrition science and community health. Holy Cross says a highlight of the symposium was the Culinary Medicine Masterclass, three hours of hands-on learning on how to prepare healthy, culturally relevant meals that support chronic disease prevention.

Roth says this and other Food Is Medicine work results in measurable improvements in health outcomes. This includes reductions in readmissions and emergency room visits and improvements in chronic disease management.
"We are joining with partners to change the dynamics in communities that are under-resourced," Roth says. "We are increasing their food access."