At one of the country's largest nonprofit health systems, it may seem like a daunting task to get clinicians on the same page. But Ascension, with facilities in 16 states and the District of Columbia, credits the Recognize and Rescue initiative it started about five years ago with preventing more than 4,000 deaths in 88 hospitals over a three-year study period, reducing risk-adjusted mortality by 20%.
The Recognize portion of the initiative is focused on optimizing the care of high-risk conditions and preventing the deterioration of the patient's condition. It includes early identification of serious conditions such as sepsis and breathing problems; preventing health care-associated infections; monitoring and minimizing the side effects of certain medications; and engaging in goals-of-care discussions with patients and families. The Rescue portion of the initiative calls for prompt management of events. It includes guidance on standardization of rapid response and on code team process and protocols; escalation and use of the chain of command for resolving concerns; promoting teamwork while assessing and managing patients; and prioritizing frontline worker education through simulations.
Ascension leaders provided tool kits on the initiative to each market, which started their work in January 2022. The initiative ultimately involved more than 2 million patients over the first three years, and the results were published in the February edition of The Joint Commission Journal on Quality and Patient Safety.

Catholic Health World spoke with Dr. Mohamad Fakih, Ascension chief quality officer, about why the system started the initiative and why it has been successful. His responses have been edited for length and clarity.
What brought this on?
With the COVID pandemic, we witnessed many changes in health care. We had sicker patients, disruptions in the operational and clinical processes, and unprecedented pressure on the workforce. The big element for us was how to support our health care workers, to ensure that we have the optimal treatment for patients, not just COVID, but anyone who's coming to a hospital. How do we treat them in the best way possible, with no gaps in care, and how can we assure that these patients don't get exposed to any harm when they are in our facilities?
During the pandemic, the workforce was extremely exhausted. A lot of very seasoned health care workers left and newer people were coming in. We needed to also make sure that they have the best competencies to do their jobs. So that was also part of our focus, to have a standardized approach.
This sounded like the ultimate playbook. Was it a matter of putting it together and then communicating it?
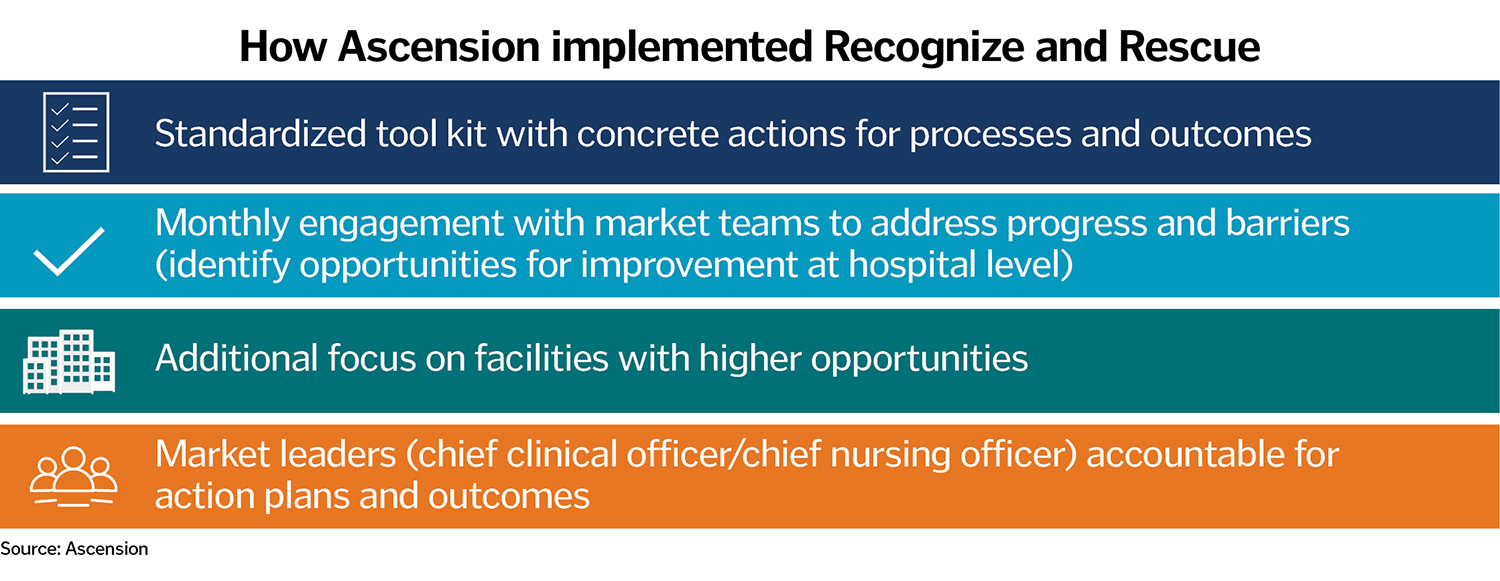
I can buy a cookbook, but it does not mean I'll become the best chef, right? It's how we follow that recipe. We created a standardized tool kit that we shared with leaders of each market. We also underscored the importance of including key disciplines, ensuring multidisciplinary collaboration. We involved the clinical arms, both physician and nursing, in addition to pharmacy and other supporting services. The tool kit had concrete actions for processes and outcomes, how to do things to get to your goal.
We engaged every market. Initially it was monthly, and then after a year, we dropped it to every two months. We were supporting them technically on how to establish processes and adopt best practices, but also pushed for accountability of the leaders. We had additional focus on facilities that had high opportunities, or those that may need more support.
Were people on board and happy to get clear direction? Were there questions or resistance?
People become much less skeptical when they see improvement happen. When they see their numbers improve, then they believe more because they're seeing it. We had a mix, initially. We had people doubting that it's going to be effective, but we had others that embraced it.
I remember one of our market teams was very excited to embrace it. They had big opportunities, and they started working on it. What was really nice is that they shared their experience and findings with other markets.
So it wasn't just the system pushing stuff at you, but also the learnings from each of the markets was shared, either we shared it from the system perspective or directly engaging each other. When you're in these calls, it's very collaborative. It has some accountability, but the main focus is pushing learning and how you improve your processes.
You've tied this work to Catholic social teaching. How so?
Almost 25 years ago, the Institute of Medicine (now the National Academy of Medicine) recommended addressing quality based on six domains, or STEEEP: Safe, Timely, Effective, Efficient, and Equitable, centered around the Patient. We've worked on how to marry the STEEEP framework with some of the principles of Catholic social teaching.
For example, promoting and defending human dignity and attending to the whole person requires us to be person centered. Acting on behalf of justice steers us to provide effective, timely and equitable care. Stewardship of resources translates into efficient care. Finally, advocating and caring for the poor and vulnerable speaks to equitable care. This brings the value of Catholic social teaching in optimizing care for our patients.
I think connecting it with these values is very, very important. I think it resonates with those that are doing the care, too.
Are other systems reaching out to you about this?
We've had calls from a few different leaders from other organizations about this. I believe it is a generalizable initiative or product. It has been one of the most successful efforts I have been a part of, and I'm so proud of the work that has been done within our ministry.
What kinds of new problems are you tackling?
I don't want to call it Recognize and Rescue 2.0, but we are evolving to address other important quality elements post-pandemic. We were able to bring in other disciplines. We've been doing a lot of work on diagnostic stewardship, which is the right test for the right patient.
Looking back, what is the general feeling about the work you and others at Ascension have achieved?
I'm so, so proud of all the teams at Ascension from the front line to the managers to directors, leaders at the market level, at the system level, and the passion we have as a system to keep quality and safety in the forefront. That means so much to me. I truly believe if you have the collaboration and the focus and the drive, you can be number one in whatever you want to do.
A lot of the folks did it because they had the drive and the passion to do the work right. This is probably one of the best things I've ever been involved in and I'm so proud to be part of that team. I give a lot of credit to those that did the work on the front line.
