BY: BRIAN SMITH, MS, MA, MDiv; MICHAEL J. KRAMAREK, PhD; THOMAS P. GAUNT, SJ, PhD; and DAVID LICHTER, DMin
The Catholic Health Association has partnered with the National Association of Catholic Chaplains (NACC) to study trends in health care chaplaincy for the last 20 years. In 1998 and 2008, the two associations conducted surveys of their chaplain members who ministered in health care settings. The analyses were performed in-house and the results were shared with their respective members. Desiring a more scientific approach to study trends in health care chaplaincy and spiritual care departments, CHA and NACC commissioned the Center for Applied Research in the Apostolate (CARA) to survey spiritual care ministry workers in Catholic health care institutions in the fall of 2018.
Here are highlights of the survey of all spiritual care ministry workers and a smaller survey of those who oversee or manage the spiritual care department of their organization. Surveys were sent to 1,600 spiritual care ministry workers with 380 of them serving as directors of spiritual care or mission leaders.1 The response rate was 32% for spiritual care workers overall and 50% for those who oversee spiritual care departments. These findings draw from respondents' answers, previous CHA/NACC surveys and an analysis performed by the three organizations involved in conducting the survey.
SURVEY 1: SPIRITUAL CARE MINISTRY WORKERS
Using averages of the demographic data and the most frequent responses to questions by all respondents, we are able to learn more about what a typical spiritual care ministry worker looks like. A typical spiritual care ministry worker is a lay Catholic, 59-year-old white woman with a master's degree and 12 years of experience in spiritual care. She had full-time work experience in parish ministry. She is a board-certified chaplain with four units of clinical pastoral education and a member of at least one professional organization. She may have entered spiritual care ministry for one of several reasons, not least of which is a desire to help others and feeling called to this ministry.
This typical spiritual care ministry worker is employed full-time for an employer that belongs to a health care system. She works on a local level in an acute care setting and/or in palliative care. A typical spiritual care ministry worker, if he is a priest, administers the Anointing of the Sick about four times a week, provides Holy Communion to individual patients about four times a week, and celebrates a Catholic Mass about three times a week.
Spiritual care ministry workers report two broad areas that present the greatest challenge facing them in providing spiritual care: organizational hurdles and other care-related matters. Organizational challenges include lack of staffing (specifically, a shortage of Catholic priests), lack of qualified candidates for spiritual care ministry, budgetary constraints, need for a more just pay scale, lack of training and continuing education, marginalization of spiritual care (this challenge can include overcoming the fact that spiritual care departments are not revenue-generating), lack of time and other obstacles. The second group of barriers to providing spiritual care includes challenges in the diversity of the served population, the ever-changing health care system, extended services care and self-care.
A CLOSER LOOK AT STAFF CHAPLAINS
Demographics: Fifty-six percent of spiritual care ministry workers are female and 44% are male. The majority (84%) are Caucasian/European American; 8% African American/Black; 3% Hispanic/Latino; 2% Asian/Pacific Islander/Native American and 3% identify as "other."
In regard to age, staff chaplains – those who provide direct patient care – were born on average in 1958 (which makes them 60 years old at the time the survey was administered). Half of them are between 32 and 61 years old and the other half between 61 and 94 years old. Significantly, religious respondents are 11 years older, on average, than lay respondents. Staff chaplains, on average, plan to retire in 11 years, with half planning to retire in the next 10 years.
Religious Affiliation: Spiritual care ministry workers in Catholic health care settings include individuals who work in organizations belonging to CHA and/or NACC. Sixty-seven percent of the staff chaplains who responded to the survey are Catholic, 20% are Protestant, and fewer than 10% are either Christian nondenominational (6%) or some other faith (6%).
This was a surprise finding for the staff of CHA and the NACC because it does not reflect a 20-year trend of a shrinking percentage of Catholic staff chaplains (87% in 1998 and 59% in 2008). Possible explanations provided by CARA were the survey methodology in 1998 and 2008 was not as scientific and may have underreported the number of Catholic staff chaplains, or that a disproportionate number of Catholic staff chaplains completed the 2018 survey, making it appear that the number of Catholic staff chaplains has increased over the last 10 years. When asked to describe the religious denominations of their staff, those who oversee spiritual care programs indicated 46% of their staff are Catholic, 43% Christian and 10% other faith traditions. These data are more consistent with the trend we have been observing and what both associations hear from members, namely that the number of Catholic staff chaplains is steadily declining and that it is increasingly more difficult to fill these positions, especially with Catholic priests.
Education: A high level of formal education is found among spiritual care ministry workers. Four in five staff chaplains have a master's degree (79%) and another one in 10 has a doctorate (10%). About one in 10 has a bachelor's degree or less (8%). A few staff chaplains have some college or associate degrees (2% or five respondents), high school or less (one respondent), or trade or technical school (one respondent).
Care Setting and Allocation of Time: The majority (77%) of staff chaplains work at a local level of a health system, 13% at a regional and 10% at a state or national level. Respondents indicated they work in multiple care settings with 70% in acute care, 41% in palliative care, 30% in behavioral health, 29% in long-term care, 29% in outpatient, 27% in cancer centers, 26% in hospice, 20% in assisted/independent living, 11% in physician/clinical offices and 7% in home health.
A typical spiritual care minister spends 43% of his or her time on patient and family services, 38% on administrative work and 19% on staff support. Patient and family services include sacramental and liturgical duties, spiritual care assessment and intervention, bereavement support and other life cycle events and ethics consultations and family care conferences. Administrative work includes documentation, staff education, participation in the organization's committees and meetings and working with local clergy and community. Staff chaplains spend 60% of their time with patients and families, 21% performing administrative work and 17% providing staff support.
SURVEY 2: SPIRITUAL CARE DEPARTMENTS
A typical spiritual care department is managed by a spiritual care director who reports to a vice president or director of mission services. There does not seem to be a dominant staffing model, but rather a combination of board-certified chaplains, spiritual care providers with some clinical pastoral education, clinical pastoral education students and spiritual care volunteers.
Based on all respondents, the average spiritual care department is comprised of nine full-time equivalents: one director, three board-certified chaplains, four non-board-certified chaplains, one clinical pastoral education student or resident, one administrative support person and 20 volunteers. (A full-time equivalent is a measure of work hours equal to the hours of one full-time employee.)
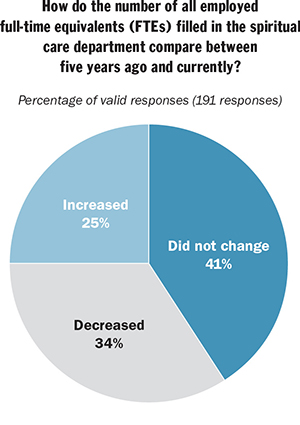
During the period between 2013-2018, most spiritual care departments (41%) reported no change in FTEs. Twenty-five percent experienced an increase in FTEs and 34% saw a decrease of FTEs that averaged 0.5 full-time equivalents.
Daily Census: We asked, "What is the average daily census in each care setting served by your spiritual care department?" Respondents reported a daily average of 213 patients served in acute care, 138 in outpatient settings, 120 in long-term care, 64 in hospice and home health, 44 in cancer centers, 33 in palliative care and 27 in behavioral health.
Coverage: When asked about the typical spiritual care coverage in their departments, 76% indicated some type of 24/7 coverage was provided. Eighty-one percent indicated on-site coverage, 61% on-call coverage.
In regard to on-call coverage, 55% reported their on-call coverage is provided by their staff chaplains, 23% by per diem chaplains, 19% by local clergy, 13% by spiritual care volunteers, 8% by students and 4% by clinical pastoral education residents. Furthermore, 29% of respondents indicated that the on-call personnel are compensated hourly, 21% per call rate and 6% daily stipend. Finally, 55% of respondents indicated on-call coverage is provided in-person, 23% by telephone, 3% by some other means and 2% via e-chaplaincy or video-conferencing.
Standards and Accreditation: Most spiritual care departments (85%) have a set of standards for spiritual care. When asked if they have an accredited clinical pastoral education program, 85% of respondents said no and 15% yes, with the vast majority accredited by the Association for Clinical Pastoral Education. In the 2008 CHA/NACC survey, 27% of respondents indicated they had a clinical pastoral education program and 73% stated they did not.
Administrative Tasks: A typical department collaborates with the medical/clinical team, which includes sharing of documentation. Ninety percent report a somewhat to very effective relationship between the spiritual care department and the clinical staff. Eighty-six percent of respondents use electronic medical records for documentation and communication. Spiritual care referrals are communicated primarily by phones/pagers 85%; electronic requests 74%; rounding 71%; and voicemail 70%. The average spiritual care referral is answered in 17 hours.
When asked whether their spiritual care department uses patient satisfaction tools to assess the quality of spiritual care provided, 60% responded yes and 40% no. The largest group of respondents indicated the use of Press Ganey surveys.
Challenges: Those who oversee spiritual care departments report their main challenge is finding qualified chaplains. When asked how long it takes to fill a position in their department, respondents indicated that, on an average, it takes six months to fill a director of spiritual care position and three months to fill a staff chaplain position.
Eighty percent of respondents indicated certification requirements to be at least one of the barriers, 71% education and experience requirements, 56% salary offered, 51% geographical challenges, 37% competition from other employers, 31% benefits offered, 31% limited support from diocesan and religious institutions in the area and 18% finding the needed religious affiliation.
SUMMARY
Spiritual care ministry workers serving in Catholic health care institutions are aging without an adequate pipeline of younger chaplains in place. The average staff chaplain is 60 years old and half of them plan to retire in the next 10 years. Significantly, those directly responsible for overseeing spiritual care departments plan to retire two years earlier than others. Further, the Catholic spiritual care department/mission leaders plan to retire on average three years earlier than non-Catholics.
The allocation of resources by Catholic institutions for spiritual care ministry workers shows variations across the country. In 40% of the organizations surveyed, staffing has remained the same, has declined in one-third of the organizations surveyed and increased slightly in 25% of the organizations. Where there has been a decrease, the average department saw a reduction of 0.5 FTE. In 2013, there were five spiritual care ministry FTEs employed in an average spiritual care department, as compared to four FTEs in 2018. When asked, "What is the biggest challenge facing spiritual care?" lack of staffing was mentioned by practically all spiritual care ministry workers (98%).
The shortage of Catholic priests available to minister to their patients also was noted. Challenges to recruiting more spiritual care ministry workers include the extensive education and experience required for the positions and the inadequate salary and benefits paid to masters-level-prepared professionals.
Although the average number of full-time equivalent spiritual care ministers in health care institutions has decreased over the past five years, the patient and staff demand for spiritual care ministry continues. Three-quarters of the spiritual care departments report that they provide 24/7 coverage. These demands are incongruent with the declining number of qualified chaplains and the decrease of resources for chaplains in many Catholic systems.
WHAT SHOULD THE MINISTRY DO?
- Hire staff chaplains with less experience and help them advance in their profession.
Since the greatest challenges to finding qualified chaplains are the educational and experience requirements, organizations must be willing to hire spiritual care providers who are working on certification. That is, they have one or two units of clinical pastoral education. In addition, organizations should offer time and resources that allow spiritual care providers to complete additional units and move toward board certification. - Ensure the salary and benefits for chaplains are fair and equitable.
The vast majority of chaplains have completed master's or PhD-level educational programs with hundreds of supervised clinical hours. Their salary and benefits, when compared to peers in other roles with the same level of education and clinical training, are significantly lower.2 It is time for Catholic health care to pay a just wage to this group of employees who are essential to the Catholic identity of our institutions. - Help senior leaders understand spiritual care as an essential and distinctive feature of Catholic health care.
The marginalization or diminishment of spiritual care was noted by spiritual care ministry workers as a particular challenge for the provision of spiritual care in their organization. Catholic health care's view of the human person as a composite of body, mind and spirit comes from the Gospel stories of how Jesus healed. How we approach care and healing in our facilities must involve all three if we are to be called a ministry of the church that continues the healing mission of Jesus. - Recruiting volunteers is a short-term fix, but not a solution to the problem.
Volunteer spiritual care ministers are a major resource for the spiritual care departments in Catholic health care institutions. In many locations they provide an initial visit, offer prayer, distribute Holy Communion to Catholic patients and generate referrals for the experienced chaplains. This triaging of patients and those who reside in long-term care, senior or rehabilitation settings helps ensure that chaplains are working at the top of their professional certification. This is similar to how licensed nurses are assisted by certified nurse assistants and trained patient experience volunteers. This allows nurses to perform the more complex clinical procedures and be involved with physicians in the care planning. We would not think of replacing nurses with volunteers; nor should we think that volunteers or local clergy can replace professionally trained chaplains without adversely impacting the quality of care.
CONCLUSION
Spiritual care ministry is a key element of Catholic health care. The current population of spiritual care ministry workers is nearing retirement age, which will place additional stress on spiritual care departments to recruit and train their replacements in coming years.
The increasing complexity and regulatory environment of health care intensifies the administrative tasks and limits direct patient and staff care. This changing health care environment may limit the number of spiritual care ministers employed, while also expanding the need for spiritual care services to be provided. This highlights the necessity for health care leadership to be knowledgeable of and responsive to the critical role of spiritual care ministry in Catholic health care.
BRIAN SMITH is vice president, sponsorship and missions services, the Catholic Health Association, St. Louis. MICHAEL J. KRAMAREK and THOMAS P. GAUNT, SJ, are with the Center for Applied Research in the Apostolate, which is affiliated with Georgetown University in Washington, D.C. Kramerek is a research associate and Gaunt is CARA's executive director. DAVID LICHTER is executive director of the Milwaukee, Wis.-based National Association of Catholic Chaplains.
NOTES
- Spiritual care ministry workers met the criteria for this study if they work in the United States, are employed to oversee or deliver spiritual care in a health care setting and are members of CHA or are members of NACC working in Catholic health facilities that are not members of CHA.
- The most recent salary survey, sponsored by the Association of Professional Chaplains (APC) and the National Association of Catholic Chaplains (NACC), with financial support from CHA, was conducted in 2018 by Sullivan Cotter. Organizations that did not participate can purchase the report directly from NACC by contacting Phil Paradowski ([email protected]) or from APC by contacting Carol Pape ([email protected]).