BY: JEAN M. LAMBERT and MICHAEL D. CONNELLY
Ms. Lambert, vice president, mission integration, Catholic Health Initiatives, Erlanger, KY, formerly filled that role at Catholic Healthcare Partners, Cincinnati. Mr. Connelly is president and chief executive, Catholic Healthcare Partners.
A Catholic System Develops a Way to Replenish and Expand Its Ranks of Chaplains
Recognizing that Catholic hospitals must treat the whole person, including mind, body, and spirit, and recognizing the national critical shortage of chaplains, Catholic Healthcare Partners (CHP), Cincinnati, has worked proactively to revitalize its approach to attracting and retaining top-quality spiritual caregivers.
In the spring of 2004, CHP decided to address this issue directly because of two major challenges in maintaining effective spiritual care:
- In the past, the majority of chaplains in Catholic health care were Catholic priests and women religious. Today, the majority of chaplains are laymen and laywomen from various faith traditions.
- Chaplain salaries were not commensurate with the job expectations, education requirements, and certification necessary for a person to effectively perform the role of chaplain.
To ensure that this redesign remained a priority at CHP, the conversation started at the highest levels of the organization. In April of that year, Michael Connelly, the system's president and CEO; Sr. Doris Gottemoeller, RSM, PhD, senior vice president, mission and values; and Jean Lambert, then vice president, mission integration, met to develop and implement a strategy.
The three decided to initially approach these challenges by developing a database that would:
- Serve as an inventory of everyone involved in spiritual care
- Help CHP find a way to meet the system's standards for certification
- Assist in identifying opportunities for continuing education and professional development of chaplains
To ensure accuracy, each CHP chaplain was asked to enter his or her data via CHP's intranet.
Inventory Outcomes
Among the key observations from CHP's spiritual care inventory were the following:
- The average age of the system's chaplains was 64 years. At any given moment in the future, a full 25 percent of them would need to be replaced due to attrition.
- Twenty-six percent were women religious or clergy.
- Forty-seven percent were certified by either the National Association of Catholic Chaplains (NACC) or the Association of Professional Chaplains (APC).
- Eighty-seven percent had a master's degree or higher.
- Self-identified educational needs focused on ethics and theological reflection.
Committees Established
Spiritual care directors from each of CHP's nine regions played a significant role in moving the agenda forward. To organize the effort, they helped form committees to develop data on credentialing, chaplain competency, productivity, and outcome measures.
Extensive research was undertaken for benchmarking purposes. The committees studied the competencies materials from the NACC and the APC; the productivity and outcome measures data from Catholic Health Initiatives, Denver; and the concept of levels of chaplaincy developed by Anne Bellan and Br. Edward Smink, OH, when they were at Catholic Healthcare West, San Francisco. The committees used data to develop specific recommendations that could be implemented over time to enhance the quality of CHP's pastoral care services.
Standards Called for Certification
One recommendation, concerning the implementation of pastoral care certification standards, was for CHP to determine that, "beginning in 2007, all chaplains were to be certified." The credentialing process was developed for those who were already in the system. Eligible chaplains were asked to participate in a credentialing program that included an application and interview process to help identify gaps. The program facilitated educational opportunities for those chaplains who needed either clinical pastoral education (CPE) or an update in theology.
As a result, three years later, more than 90 percent of CHP chaplains are either credentialed by CHP or certified by NACC or APC.
Competencies
The competencies promulgated by NACC and APC became the focal point for a CHP conversation about the future of chaplaincy and the critical question: "From where will future chaplains come?"
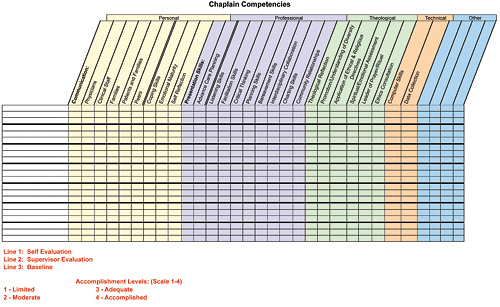
The committee agreed that the competencies, although extremely helpful, should be presented in a more user-friendly format that could be used as a management tool. As a result, a grid was developed to be used by pastoral care directors for performance appraisal; development of individual and department educational goals; and performance improvement. In the end, the competencies served as the basis for redesigning position descriptions in a way that made the recruitment of future chaplains more intentional and better defined.
Outcome Measurement
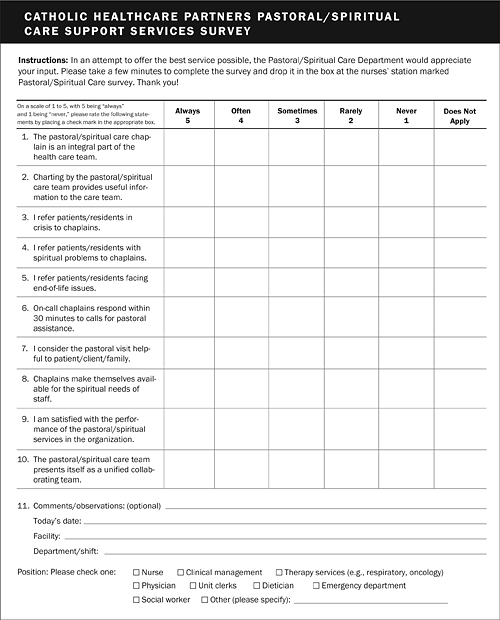
Like most other systems, CHP uses patient satisfaction scores to measure chaplains' effectiveness. The challenge involved in doing so — as identified by spiritual care directors across CHP and at other systems — is that much of chaplains' work is done with dying patients and their families, who, for obvious reasons, cannot be asked to fill out patient satisfaction surveys. In order to gather more evidence for use in outcome measurement, CHP developed a "Pastoral/Spiritual Support Services Survey" instrument and administered it to those who work with chaplains (including nurses, physicians, emergency departments, clinical management, and others) on a regular basis. Results of the surveys were overwhelmingly supportive of the chaplains' effectiveness as members of their respective health care teams.
Professional "Ladder"
One of CHP's major challenges is the recruitment of certified chaplains. Because certification requires a master's degree in theology or a related area, as well as four units of CPE, developing a pool of certified chaplains would take at least three to five years. Something had to be done to manage the lacuna.
Several years ago, Bellan and Br. Smink developed job descriptions for various levels of chaplaincy. Using their work as a basis, CHP developed a professional "ladder" for chaplains. The professional ladder could serve not only as a way for chaplains to progress professionally but also as a way to manage departmental needs.
Job descriptions were developed for "certified," "associate," and "assistant" chaplains. The distinctions between one description and another were critical from a professional standpoint and also allowed the system's Human Resources (HR) Department to develop distinct salary ranges for the three positions. In the end, although a job description was developed for the assistant chaplain role, opinions differed on how it would function; as a result, the salary was not set.
Salary Initiative
Over the past 20 years or so, as U.S. demographics changed and more laypeople assumed the role of chaplain, health care systems have been slow to evolve from the days when they offered stipends to the priests and women religious who served as chaplains. The average salary was $37,000.
To develop salary ranges for chaplains commensurate with educational and professional expectations, CHP engaged a compensation and benefits consultant. As a basis for these ranges, the consultant used the redesigned job descriptions, chaplain competencies, CHP core competencies, and the new professional ladder.
One of this article's authors, Jean Lambert, was CHP's vice president for mission integration. Working together with Michael Kushner, former vice president for compensation and benefits, she met several times with the system's HR leaders to clarify the issues involved. Because HR professionals normally base salary ranges on market data, it was important to present the rationale for the proposed changes clearly. For example, HR executives recognized that recruiting chaplains for smaller, more rural facilities might sometimes be more difficult than recruiting for larger and more complex institutions, and that fact had to be taken into account in developing appropriate ranges.
The discussion with the HR executives established the following ranges:
- Certified chaplain, $44,600-$74,400
- Associate chaplain, $40,000-$63,400
The benchmark for the midpoint was set at $50,000 for the certified chaplain and $45,000 for the associate chaplain.
Expanding the Ranks
Spiritual care is essential to CHP as it works to extend the healing ministry of Jesus, and, while much has been accomplished over the past three years, the journey is far from over. The challenge continues as the system works to find new ways to both replenish and expand the ranks of its chaplains.
Copyright © 2007 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.