BY: SANDRA E. REZNIK, MD, PH.D.
Emergency contraception, that is, any of a number of methods to prevent pregnancy after coitus, has become more effective and certainly easier to obtain in recent years. Levonorgestrel, also known as "Plan B," is, by wide agreement within the scientific community, the most effective emergency contraceptive agent available and, for women 18 or older, can now be obtained without a prescription. Confusion about this agent's mechanism of action has fueled debate among some non-medical people, however: Does Plan B act only as a contraceptive or also as an abortifacient?
Unfortunately, there has not been adequate emphasis on how Plan B differs from the emergency contraceptive agents that preceded it, and scientifically unsupported wording on its package insert has increased misconceptions about how Plan B works. Unlike its predecessors such as mifepristone (also known as RU486), levonorgestrel acts to prevent pregnancy before, and only before, fertilization occurs.
The purpose of this article is to review the evidence for how levonorgestrel prevents pregnancy.
We know that several events must occur for a pregnancy to begin and then to be maintained. Sperm must enter the cervix and travel up the uterine canal to the fallopian tube, which is the site of fertilization. An egg cell, or oocyte, must be released from the ovary by a process known as ovulation, and a sperm cell must unite with the oocyte by the process known as fertilization. Finally, the fertilized oocyte must develop into an early embryo, known as a blastocyst, and become implanted in the uterus. So entrance of sperm into the cervix and ovulation precede fertilization, whereas development of the blastocyst and implantation follow it.
The debate surrounding Plan B, therefore, is focused on whether this agent affects only ovulation and the entrance of sperm into the cervix, i.e. pre-fertilization events, or if it also affects the development of the embryo and implantation, i.e. post-fertilization events.
To begin with, levonorgestrel is an artificial progestin — a synthetic compound with a structure and function similar to the female hormone progesterone. Progestin helps to make the uterus more receptive to implantation and helps maintain pregnancies.1 Biologically, the concept of a synthetic progestin rendering the endometrium less receptive to implantation, and thereby acting as an abortifacient, is completely illogical.
Nevertheless, changes in the endometrium after exposure to levonorgestrel were examined in animal studies. Neither the rat2 nor the new-world monkey3 demonstrated any endometrial changes consistent with decreased receptiveness to implantation. Similar results were found in an in vitro study that tested the effects of this agent on endometrial cells growing in culture medium.4 Finally, a human tissue study showed only minimal changes of the endometrium resulting from exposure to levonorgestrel.5
There is abundant evidence, on the other hand, that levonorgestrel affects pre-implantation events. There are two mechanisms whereby contraceptives prevent fertilization. One is by preventing the union of sperm and oocyte through the introduction of an obstacle impeding that union. The other is by inhibiting ovulation. Several investigators have shown that Plan B in fact causes thickening of cervical mucus, thereby decreasing the number of sperm able to enter the cervico-uterine canal and ultimately able to reach the oocyte.6
It is virtually undisputed that levonorgestrel prevents ovulation. Ovulation is always preceded by a characteristic spike in production and release of luteinizing hormone, an anterior pituitary hormone that stimulates the ovary. Studies7 have shown that Plan B suppresses the hypothalamus and pituitary glands and thereby wipes out the so-called luteinizing hormone surge. Without that hormonal surge, ovulation does not occur.
Before I address the issue at the center of questions some non-medical people have about Plan B, namely, whether this over-the-counter pill prevents implantation of the early embryo in addition to inhibiting ovulation, I need to mention a few biological facts about human reproduction:
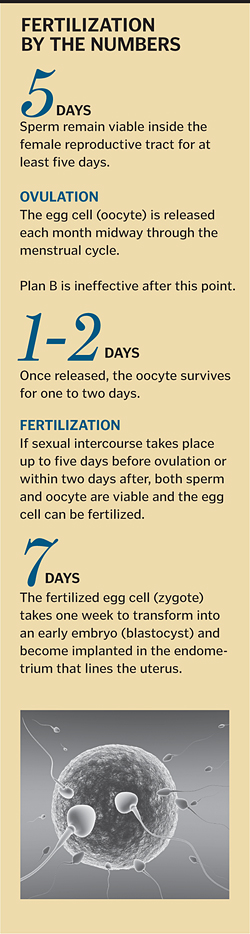
- The oocyte, released each month midway through the menstrual cycle, survives for one to two days.
- Sperm, in contrast, remain viable inside the female reproductive tract for at least five days.
- So if coitus occurs more than two days after ovulation, fertilization will not occur, because the oocyte will no longer be viable.
- If sexual intercourse takes place up to five days before ovulation, fertilization can occur, because the sperm maintain their viability for that long.
- Once fertilization occurs, the fertilized egg cell, or zygote, takes one week to transform into the blastocyst and become implanted in the endometrium.
Where dispute exists, it is focused on whether, in addition to preventing ovulation and thickening cervical mucus, Plan B acts after fertilization has occurred by preventing implantation of the early embryo. There is an abundance of clinical and epidemiological data that answers the question: No.
The timing of the administration of Plan B, meaning how many days elapse between coitus and when the patient takes the pill, is absolutely critical and closely tied with the success rate of the contraceptive.
Piaggio et al.,8 have shown that the risk of pregnancy increases as the interval between coitus and ingestion of the agent lengthens. If Plan B worked by preventing implantation, then the most effective time to administer the contraceptive would be right around the time implantation would occur. Because fertilization occurs within five days of coitus and implantation takes place seven days after fertilization, the most effective time to administer Plan B would be seven to 12 days after intercourse.
In fact, levonorgestrel is completely ineffective when it is given that late.
Furthermore, several investigators have shown that the effectiveness of Plan B drops dramatically if given more than two days after coitus.9 This result is the exact opposite of what would be expected to happen if the agent interfered with implantation of the embryo — if that were the case, Plan B would become more effective as time passes after coitus and the moment of implantation approaches. In fact, the effectiveness of Plan B decreases with time after coitus, because every hour that passes before the patient takes the pill increases the probability that ovulation will have occurred. Once the oocyte is released into the fallopian tube, and once sperm have entered the tube, levonorgestrel has no effect.
When given within two days of coitus, Plan B is effective only approximately 50 percent to 80 percent of the time, meaning it prevents only 50 percent to 80 percent of pregnancies that would have occurred in the absence of any contraceptive. This finding is perfectly compatible with levonorgestrel's mechanism of action being the prevention of ovulation. If ovulation has already occurred when the agent is given, in fact if ovulation is even imminent, as is true in the 20 percent to 50 percent of cases of failed contraception, the drug will have no effect. If Plan B's mechanism of action involved a change in the endometrium, then one would expect a higher rate of success, as there would be no such critical time period.
Taken together then, there are biological, clinical and epidemiological data clearly indicating that Plan B's mechanism of action involves only pre-fertilization events.
To summarize, biological experiments involving both animal and human tissue show Plan B has no effect on the endometrium that would be compatible with decreased receptivity for implantation. Thickening of the cervical mucus — as this agent does — thereby impeding the entrance of sperm into the cervico-uterine canal and thus decreasing the number of sperm available for fertilization, would certainly represent a pre-fertilization mechanism of contraception.
Levonorgestrel is not always effective, which is compatible with the fact that it changes nothing if ovulation has already occurred.
The effectiveness of levonorgestrel drops rapidly during the passage of time after coitus, for the probability of missing ovulation increases by the hour. Plan B is not very effective once two days have passed since coitus, and it is not effective at all if there have been seven to 12 days since intercourse — the time frame when implantation actually occurs.
Some of the concerns about how Plan B works have been driven by the unfortunate and inaccurate description on the package insert, which includes a statement that levonorgestrel acts by preventing implantation. There are absolutely no data to support this statement, while there are plenty of data, summarized above, to support the conclusion that levonorgestrel acts only before fertilization has occurred.
There is an urgent need to correct the misconception that levonorgestrel is a post-fertilization contraceptive. Contraceptives that act after fertilization are considered abortifacients, whereas agents that affect any of the events that precede fertilization are simply contraceptives. As such, the use of levonorgestrel is unnecessarily limited due to the misconception about how it works. For an individual patient, the effectiveness of Plan B decreases with every passing hour, because the chance of missing ovulation increases as time passes — and science has demonstrated Plan B doesn't work after ovulation occurs. For thousands and thousands of victims of sexual assault, the opportunity to act before fertilization will continue to be missed until the data summarized here are carefully considered.
NOTES
- Jonathan S. Berek, Novak's Gynecology, 13th ed., (Philadelphia: Lippincott Williams & Wilkins; 2002), 249.
- Müller et al., "Postcoital Treatment with Levonorgestrel Does Not Disrupt Postfertilization Events in the Rat," Contraception 67, no. 5 (2003): 415-419.
- Ortiz et al., "Post-Coital Administration of Levonorgestrel Does Not Interfere with Post-Fertilization Events in the New-World Monkey Cebus Apella," Human Reproduction 19, no. 6 (2004): 1352-56.
- Lalitkumar et al., "Mifepristone, but Not Levonorgestrel, Inhibits Human Blastocyst Attachment to an in vitro Endometrial Three-Dimensional Cell Culture Model," Human Reproduction 22, no. 11 (2007): 3031-37.
- Landgren et al., "The Effects of Levonorgestrel Administered in Large Doses at Different Stages of the Cycle on Ovarian Function, and Endometrial Morphology," Contraception 30, no. 3 (1989): 275-89.
- Croxatto, "Emergency Contraception Pills: How Do They Work?" IPPF Medical Bulletin 36 (2002): Appendix 1-1, 2; K. Gemzell-Danielsson and L. Marions, "Mechanisms of Action of Mifepristone and Levonorgestrel when Used for Emergency Contraception," Human Reproduction Update 10, no. 4 (2004): 341-48.
- Croxatto et al., "Pituitary-Ovarian Function Following the Standard Levonorgestrel Emergency Contraceptive Dose or a Single 0.75 mg Dose Given on the Days Preceding Ovulation," Contraception 70, no. 6 (2004): 442-50.
- Piaggio et al., "Timing of Emergency Contraception with Levonorgestrel or the Yuzpe Regimen," Lancet 353, no. 9154 (1999): 721.
- Natalia Novikova et al., "Effectiveness of Levonorgestrel Emergency Contraception Given Before or After Ovulation — A Pilot Study," Contraception 75, no. 2 (2007): 112-18; James Trussell et al., "Effectiveness of the Yuzpe Regimen of Emergency Contraception by Cycle Day of Intercourse: Implications for Mechanism of Action," Contraception 67, no. 3 (2003): 167-71.
DR. SANDRA E. REZNIK is an associate professor at St. John's University, Queens, N.Y., where she teaches a graduate-level course in reproductive pharmacology and a reproductive endocrinology course to pharmacy students. She is a licensed physician in the state of New York who serves as a consultant on complex perinatal cases in her role as chief of Perinatal Pathology at Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, N.Y. She is often called upon to serve as an expert witness in obstetrical legal cases. She has been funded by the National Institute of Child Health and Human Development for her research in reproductive pharmacology and recently served as an ad hoc member of the Fall 2009 Pregnancy and Neonatology study section of the National Institutes of Health.
Copyright © 2010 by the Catholic Health Association of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3477.