SARA DAMIANO, LMSW, CCM, ACHP-SW, and RAFAEL BLOISE, MD, MA, MBA
Ascension
"Even if we know that we cannot always guarantee healing or a cure, we can and must always care for the living, without ourselves shortening their life, but also without futilely resisting their death. This approach is reflected in palliative care, which is proving most important in our culture, as it opposes what makes death most terrifying and unwelcome — pain and loneliness."
— From Pope Francis' message to participants of the European Regional Meeting of the World Medical Association at the Vatican on Nov. 7, 2017
With a commitment rooted in the loving ministry of Jesus, we are called to care for people living with serious illness, especially those who are poor and vulnerable. This is a pressing concern as nearly 30% of the adult population in the United States has multiple chronic conditions, this number predicted to rise with the aging of the population. Studies have shown that most people living with a serious illness experience inadequately treated symptoms, fragmented care, poor communication with their clinicians and strains on their family caregivers.1 People living with multiple chronic conditions account for a disproportionate share of health care utilization and costs, as almost half have functional impairments, and nearly all readmissions among Medicare beneficiaries occur among this group.2 Similarly, health care costs and spending continue to grow, which further widens the gap in access to affordable care, thus contributing to health disparities.3
Given our rapidly evolving health care environment, population demographics and the disproportionate impact of social determinants of health, there is an even more urgent need to address the barriers to health care access.4 In the same vein, palliative care has the unique advantage to positively impact health equity through holistic, evidence-based care for those living with serious illness.
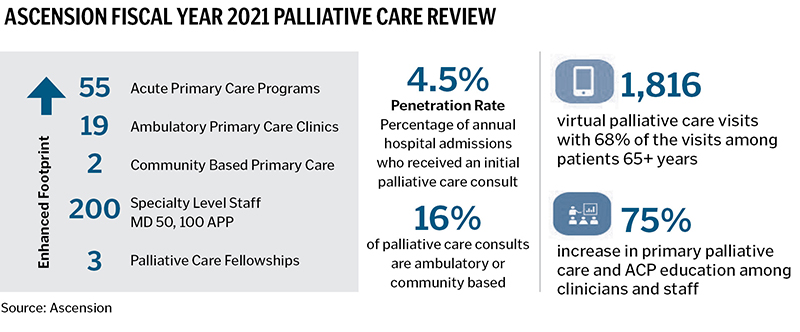
As one of the nation's leading Catholic health systems, Ascension is dedicated to transforming care across the continuum with a renewed strategic focus on palliative care. Palliative care is specialized medical care for people living with a serious illness. This type of care is focused on providing relief from the symptoms and stress of illness. The goal is to improve quality of life for both the patient and the family.5 Ascension palliative care services span 12 states, with 55 inpatient locations, 19 outpatient clinics, two community-based models of care, three pediatric programs, three fellowship programs and more than 200 interdisciplinary specialty staff with 50 physicians, 100 advanced practice providers, 30 nurses, 26 social workers and 16 chaplains. In 2021 alone, Ascension had more than 34,000 initial and subsequent visits in palliative care. In order to continue meeting and refining the level of care provided to these patients, we envision an integrated system of services that supports:
- Increased specialty palliative care access and referrals to comprehensive interdisciplinary palliative care services in the inpatient, outpatient, community and virtual settings.
- Enhanced primary palliative care skills among all clinicians and care teams in advance care planning, serious illness communication and pain and symptom management.
- Intentional integration of palliative care into the population health, care management, clinical service line, virtual care and hospice strategy.
To expand and enhance our palliative care services, Ascension has launched multiple efforts. Of these initiatives, three are specifically focused on the following: advance care planning, ambulatory care pathways and predictive analytics. These areas emerged as differentiators during the COVID-19 pandemic and have further precipitated palliative care's integration into the larger health care delivery system. Developed through strategic planning efforts with our national palliative care steering committee — with support from market level clinicians and interdisciplinary team members — these efforts included a careful review of best practices prior to launch, along with a desire to ensure person-centered care principles in every step along the way.
Dr. Baligh Yehia, senior vice president, Ascension, and president, Ascension Medical Group, said areas of focus include improving quality of life and well-being for patients and families and enhanced communication and continuity of care. "Our palliative care approach helps us address the varied and often complex needs of our patients which is a critical component of our ministry's population health focus and a tangible embodiment of our mission."
ADVANCE CARE PLANNING
The effects of the COVID-19 pandemic have isolated family members at the very time they need to make decisions together regarding end-of-life care. If a loved one dies and family members haven't talked about one another's wishes in advance, some can be left struggling, wondering if they did the right thing or feeling regrets about what was done with risk for complicated grief.6 Advance care planning is a process for all adults that involves a reflection and conversation on one's goals, values and preferences for future health care decisions. Its purpose is to help ensure that people receive medical care that is consistent with these priorities, which has become even more imperative due to the physical, mental and spiritual distress inflicted on patients during the COVID-19 pandemic.
Advance care planning should be proactive, appropriately timed and integrated into routine care. During these conversations, the patient and health care provider discuss the meaning of such planning as well as explore any fears or concerns. This process may also involve the patient choosing a health care agent(s) to speak on their behalf if they were to become too sick or injured to communicate, and often includes the completion or review of relevant legal forms, known as advance directives.
Ascension has made significant investment in engaging in these conversations in the ambulatory setting by leveraging the Affirm Health Advance Care Planning (ACP) tool as a software application in athenaClinicals, a web-based electronic health record, to support these discussions at the point of care. This dialogue is optimized through tool features such as a simple notification process, conversation guide and integrated billing to ensure that advance care planning is part of the routine clinical workflow.
The organization has seen a rapid uptake of advance care planning documentation and billing after training on the use of the tool, said Dr. Aaron Shoemaker, chief medical officer, Clinical & Network Services, Ascension. "The ACP tool aggregates the necessary documents for ACP conversations so clinicians don't have to guess." He said most importantly, patients appreciate the conversation to document and address their care wishes moving forward.
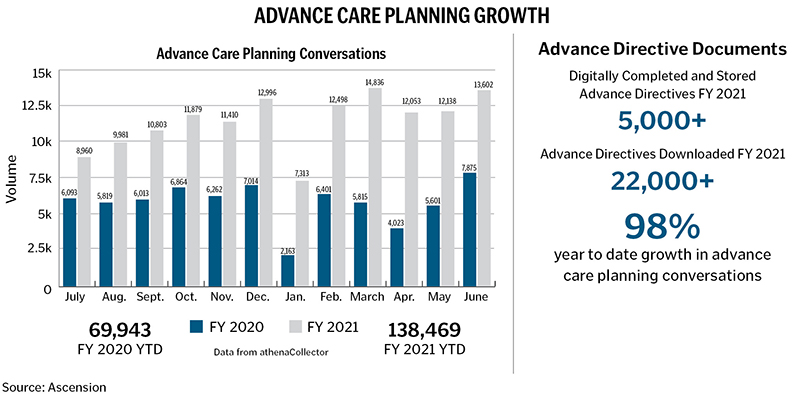
The tool allows for embedded reminders in the electronic health record to encourage clinicians and health care team members to initiate discussions with patients 65 and older. This has resulted in a 98% increase in conversations from the prior fiscal year (see bar graph on page 57). The advance care planning tool also offers a simple notification process to nudge primary care clinicians to engage in a conversation with patients during their Medicare annual wellness visit. The Medicare wellness visit is an excellent opportunity to integrate this conversation as it normalizes the process as part of a high-quality and comprehensive health care approach. The conversation guide provides a step-by-step framework for supporting this. These discussions begin by first asking patients their permission to engage in the conversations, normalizing the process, exploring their understanding and values, discussing the process of choosing a health care agent and supporting patients in sharing those wishes in the written form of an advance directive.
In 2016, the Centers for Medicare and Medicaid Services (CMS) opened up advance care planning billing and reporting codes to appropriately track and reimburse clinicians for engaging in these essential conversations. Medicare pays for advance care planning as either an optional element of a patient's Medicare wellness visit or as a separate Medicare Part B necessary medical service. It is important to note that when a patient engages in advance care planning services outside the Medicare wellness visits, CMS recommends informing patients that Part B cost-sharing applies just as it does for other physician services.7 While the introduction of these codes represents CMS's recognition of the value of these conversations, data shows underutilization of the advance care planning codes.8 To help increase awareness and appropriate utilization, the tool offers an integrated billing platform to ensure that advance care planning is part of the routine clinical workflow.
AMBULATORY CARE PATHWAYS
As part of this process, ambulatory palliative care clinical pathways were developed to guide clinicians and support patients and families living with advanced congestive heart failure and advanced cancer with a goal of improving quality of life and health outcomes.
Over the last few years, Ascension also has invested in ambulatory palliative care sites to support frail, complex and seriously ill patients. Ambulatory palliative care settings include stand-alone clinics, embedded specialty clinics and virtual palliative care. To support this expansion, Ascension has seen the growth of the traditional palliative care interdisciplinary team structures as well as the development of new staffing models with certified advanced practice providers and nursing-led models of care.
In some ministries across Ascension, this effort required the recruitment of clinical staff. In markets with limited capacity, Ascension collaborated with community-based palliative care organizations that had availability to take on additional referrals. In ministries where the palliative care team's efforts were more targeted on caring for patients with the most complex needs, all clinicians were given a primary palliative care skill set in advance care planning, pain and symptom management and appropriate communication to help the larger population.
The palliative care team supports primary care and specialty clinicians by addressing complex symptom burden, initiating conversations about goals of care, integrating advance care planning and ensuring coordination of care, carried out through the following steps:
- Identify: Provide early identification of patients who could benefit from palliative care.
- Screen: Conduct standardized evidence-based screenings of patients for symptom distress in physical, psychological, emotional, spiritual and social domains.
- Assess: Explore symptom severity and needs across all domains.
- Manage: Offer management of symptoms by the care team to improve patients' quality of life and prevent avoidable crisis.
- Refer: Consider a specialty palliative care referral for complex problems and symptoms.
An ambulatory palliative clinical pathway was created; this protocol-based, standardized set of clinical and administrative workflow steps guides care team members. While developing these care paths, careful attention was also paid to the clinician's well-being, experience and efficiency with utilizing the screening tools. Efforts included consideration of the time needed to complete the screen and exploration of ways to simplify unnecessary or duplicative documentation. For fiscal year 2022, four Ascension markets will pilot the use of ambulatory care pathways to engage and refer patients living with serious illness to specialty palliative care.
PREDICTIVE ANALYTICS
According to the Center to Advance Palliative Care, patients who receive palliative care services report a 66% reduction in symptom burden, while operationally palliative care programs lead to a 48% reduction in hospital readmissions. Moreover, recent studies have estimated lower direct hospital costs for adults with serious illness irrespective of diagnosis, with an overall $3,232 reduction in cost; a $4,664 cost reduction for cancer patients; and savings of more than $6,000 per patient from reduced need for future hospitalization.9, 10
Overall, palliative care is underutilized. Research suggests that more emphasis should be aimed at early access to palliative care to improve the experience for those who are seriously ill, not just at the end of life. Palliative care offers a large scope of practice by providing both curative treatment as well as pain and symptom relief for patients at every age and stage of life.
In order to incorporate palliative care earlier into the care delivery model of seriously ill people — particularly the top 5-15% of the most critically ill patients who account for approximately 50% of health care spending — Ascension is prioritizing the use of predictive analytics or machine-learning algorithms to help with early identification of patients who may need more support managing their serious illness.11 Focusing on inpatient and outpatient electronic health records, Ascension will be using Cerner Palliative Care tools within the electronic health records to offer timely identification and stratification of the population, and the system nudges clinicians based on algorithms for age, disease burden, utilization, functional limitations, uncontrolled symptoms and poor prognosis. Research supports that early consultation to palliative care is associated with a reduction in direct hospital costs of almost $1,700 per admission ($174 per day) for patients discharged to another level of care or home and almost $5,000 per admission ($374 per day) for patients who die in the hospital.12, 13
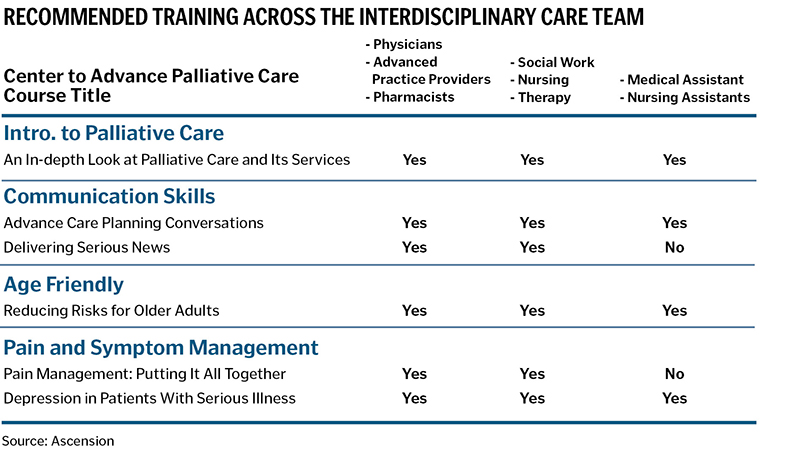
Ascension is working toward a balanced approach by improving the effectiveness and competency of all clinicians and associates in primary palliative care, through 1) a quarterly national grand rounds series that will feature expert speakers in palliative care, 2) launching the first Ascension-wide palliative care conference and 3) utilizing our Center to Advance Palliative Care system-wide membership to allow care team members access to continuing education online materials for more effective communication, pain and symptom management and age-friendly care (see table on page 59 for recommended courses). Through this approach, we will provide education on how to communicate to those with serious illness, including delivering bad news, discussing prognosis, pain and other symptom management. In addition to the process of early identification, we will also improve the assessment of identified patients and provide ongoing readjustments to their plan of care as their condition warrants to support work streams focused on transitions of care and care management.
CONCLUSION
The COVID-19 pandemic has affected both individuals living with serious illness and the overall health care environment. To serve with even greater compassion, we are embracing and supporting palliative care delivery models throughout our ministry. Continuing to transform care for people living with serious illness and addressing their physical and psychological needs is a fundamental expression of our Catholic identity and shared ministry, a reflection of God's loving presence and purpose in our lives.
SARA DAMIANO is national director of palliative care for Ascension in St. Louis. RAFAEL BLOISE is chief medical officer for Ascension Living in St. Louis.
NOTES
- Allison Silvers and Sara Hufstader-Collins, "Driving Consistent Access to High-Quality Care For People Living with Serious Illness," April 30, 2019, Center to Advance Palliative Care, https://www.capc.org/blog/driving-consistent-access-high-quality-care-people-living-serious-illness/.
- Peter Boersma, Lindsey I. Black, and Brian W. Ward, "Prevalence of Multiple Chronic Conditions Among US Adults, 2018," Preventing Chronic Disease 17, no. E106 (September 2020): https://doi.org/10.5888/pcd17.200130.
- Arlene S. Bierman et al., "Transforming Care For People with Multiple Chronic Conditions: Agency for Healthcare Research and Quality's Research Agenda," Health Services Research 56, no. S1 (August 2021): 973-79, https://doi.org/10.1111/1475-6773.13863.
- Kimberly S. Johnson, "Racial and Ethnic Disparities in Palliative Care," Journal of Palliative Medicine 16, no. 11 (November 2013): 1329-34, https://doi.org/10.1089/jpm.2013.9468.
- "What Is Palliative Care?" GetPalliativeCare.org, https://getpalliativecare.org/whatis/.
- Maarten C. Eisma, Paul A. Boelen, and Lonneke I.M. Lenferinka, "Prolonged Grief Disorder Following the Coronavirus (COVID-19) Pandemic," Psychiatry Research 288 (June 2020): https://doi.org/10.1016/j.psychres.2020.113031.
- "Advance Care Planning," Centers for Medicare & Medicaid Services, https://www.cms.gov/outreach -and-education/medicare-learning-network-mln/mlnproducts/downloads/advancecareplanning.pdf.
- Emmanuelle Belanger et al., "Early Utilization Patterns of the New Medicare Procedure Codes for Advance Care Planning," JAMA Internal Medicine 179, no. 6 (March 2019): 829-30, https://doi.org/10.1001/jamainternmed.2018.8615.
- John E. Barkley et al., "Timing of Palliative Care Consultation and the Impact on Thirty-Day Readmissions and Inpatient Mortality," Journal of Palliative Medicine 22, no. 4 (March 2019): 393-99, http://doi.org/10.1089/jpm.2018.0399.
- Nina R. O'Connor et al., "Palliative Care Consultation for Goals of Care and Future Acute Care Costs: A Propensity-Matched Study," American Journal of Hospice and Palliative Medicine 35, no. 7 (November 2017): 966-71, https://doi.org/10.1177/1049909117743475.
- Peter May et al., "Economics of Palliative Care For Hospitalized Adults with Serious Illness: A Meta-Analysis," JAMA Internal Medicine 178, no. 6 (June 2018): 820-29, https://doi.org/10.1001/jamainternmed.2018.0750.
- R. Sean Morrison et al., "Cost Savings Associated With U.S. Hospital Palliative Care Consultation Programs," Archives of Internal Medicine 168, no. 16 (September 2008): 1783-90, https://doi.org/10.1001/archinte.168.16.1783.
- Heidi Gruhler et al., "Determining Palliative Care Penetration Rates in the Acute Care Setting," Journal of Pain and Symptom Management 55, no. 2 (September 2017): 226-35, https://doi.org/10.1016/j.jpainsymman.2017.09.013.