By LISA EISENHAUER
When she was expecting her first child eight years ago, Rebecca Bernadel remembers feeling like she was just following orders from her care providers.
 Research shows that the CenteringPregnancy group prenatal care model in use at Mercy Medical Center in Baltimore improves birth outcomes for Black women and their babies. Here, yoga and mindfulness instructor Kahlil Kuykendall, left foreground, teaches
balancing and stretching poses to, clockwise from center, Nevaeh Weathers, 20, of West Baltimore; Jnai Player, 20, of Baltimore; Destiny Johnson, 22, of West Baltimore; and Keimyra Pumphrey, 21, of Baltimore. Participants learn to advocate for
themselves with care providers and they build supportive friendships. Jennifer McMenamin
Research shows that the CenteringPregnancy group prenatal care model in use at Mercy Medical Center in Baltimore improves birth outcomes for Black women and their babies. Here, yoga and mindfulness instructor Kahlil Kuykendall, left foreground, teaches
balancing and stretching poses to, clockwise from center, Nevaeh Weathers, 20, of West Baltimore; Jnai Player, 20, of Baltimore; Destiny Johnson, 22, of West Baltimore; and Keimyra Pumphrey, 21, of Baltimore. Participants learn to advocate for
themselves with care providers and they build supportive friendships. Jennifer McMenamin"It was like, you do this, you do this, you do this," says Bernadel, who is expecting her second child in August with her boyfriend and first-time father-to-be Jabarri Johnson. "This experience, I really wanted to be in tune with how I can advocate for
myself, and Jabarri can advocate for me and the baby, and all of our options."
That's why Bernadel and Johnson accepted the invitation of their midwife to try the CenteringPregnancy care model that Mercy Medical Center in Baltimore started last year. In the care model, women at or near the same stage of pregnancy attend prenatal
visits with their providers that extend into group learning sessions. The providers encourage the expectant mothers to develop supportive relationships with each other.
"We really wanted to be fully educated on our experience but also have that support from a midwife and from other women in the group," Bernadel explains.
Even though they are early in the program, Johnson says he is already excited about its patient-centered approach and the education it is providing on topics like nutrition during pregnancy, exhaustion, breastfeeding, mindfulness and mental health.
"When you want the example of how people of color want health care, I think this is a prime example when it comes to maternal health care," Johnson says. "I wish everybody could have that experience."
Attuned to disparities
The couple's midwife, Kia Hollis, wants all of Mercy's maternity patients to have the opportunity to feel similarly seen and empowered. Hollis is the director of Mercy's CenteringPregnancy
program.
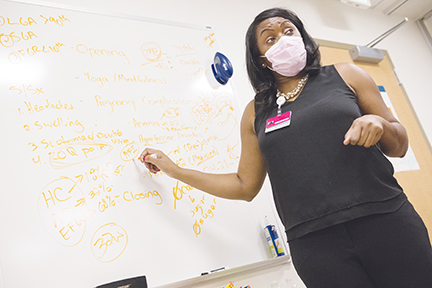 Kia Hollis, director of CenteringPregnancy at Mercy Medical Center in Baltimore, leads a discussion with a group of expectant mothers about pregnancy complications, such as anemia, allergies and gestational diabetes. The CenteringPregnancy model
is used at more than 400 sites across the country. Under the model, women at similar stages of pregnancy attend medical visits that incorporate peer group support. The medical visits include mini seminars about such topics as prenatal testing,
nutrition, lifestyle changes, domestic violence and abuse, and mental relaxation along with hands-on demonstrations on cooking, car seat installation and prenatal yoga. Jennifer McMenamin
Kia Hollis, director of CenteringPregnancy at Mercy Medical Center in Baltimore, leads a discussion with a group of expectant mothers about pregnancy complications, such as anemia, allergies and gestational diabetes. The CenteringPregnancy model
is used at more than 400 sites across the country. Under the model, women at similar stages of pregnancy attend medical visits that incorporate peer group support. The medical visits include mini seminars about such topics as prenatal testing,
nutrition, lifestyle changes, domestic violence and abuse, and mental relaxation along with hands-on demonstrations on cooking, car seat installation and prenatal yoga. Jennifer McMenaminShe says the hospital and its Metropolitan OB/GYN provider group was motivated to start CenteringPregnancy by research that shows the care model gets high marks from participants and improves outcomes for mothers and newborns, especially for Black
patients.
Mercy serves a largely African American population in the heart of Baltimore, a city whose poverty rate of 20% exceeds the national average of about 11.6%. It is one of the city's main maternity hospitals. Last year, 2,600 babies were born there.
Hollis says she and her colleagues are attuned to the dismal statistics on maternal outcomes for women of color compared to white women. She notes that those race-related disparities appear across income and education levels.
"We are trying to educate women about their bodies so that they know what warning signs and symptoms to look out for so that they can be a stronger advocate for themselves when they actually present to care," Hollis says. "Through this program,
we hope to decrease those poor health outcomes."
 Keimyra Pumphrey practices mindfulness and prenatal yoga at a CenteringPregnancy session at Mercy Medical Center. Each of the cohorts has five to eight participants. The partners of the women are welcome, too. Jennifer McMenamin
Keimyra Pumphrey practices mindfulness and prenatal yoga at a CenteringPregnancy session at Mercy Medical Center. Each of the cohorts has five to eight participants. The partners of the women are welcome, too. Jennifer McMenaminRacial maternal disparities include a pregnancy-related mortality rate for Black and Hispanic women that is up to three times higher than that of white women and higher rates of preterm births, low birth weights, and births in which women received
late or no prenatal care, the Kaiser Family Foundation says.
The nonprofit Centering Healthcare Institute created and oversees CenteringPregnancy practices at more than 400 sites in 44 states. The institute
cites
data that suggests its model counters racial disparities.
For example, a study published in May 2012 in the American Journal of Obstetrics and Gynecology compared the birth
outcomes of women in group prenatal care to those who got traditional prenatal care. One of its findings was "the racial/ethnic disparity in rates of preterm birth seemed to diminish for the women who participated in group care."
Group sessions, group support
CenteringPregnancy follows the schedule of 10 prenatal visits recommended by the American College of Obstetricians and Gynecologists — monthly appointments in the early
weeks of pregnancy and twice a month from week 28 through delivery. Its sessions are 90 minutes to two hours long. During the first part, the mothers-to-be meet with their providers for health assessments. For the rest of the session,
they take part in educational group discussions.
Mercy started its CenteringPregnancy program in October. Through February, seven cohorts were underway with five to eight participants in each; most participants are expectant mothers but a few of them are partners like Johnson. Each cohort
started at different times with women in their 12th to 16th week of pregnancy. The women are referred to the program by Metropolitan OB/GYN providers. Participation is optional.
 Jnai Player struggles to drink the beverage that must be consumed in between blood draws to test for gestational diabetes. The glucose test was part of her prenatal care in Mercy Medical Center's CenteringPregnancy program. Jennifer McMenamin
Jnai Player struggles to drink the beverage that must be consumed in between blood draws to test for gestational diabetes. The glucose test was part of her prenatal care in Mercy Medical Center's CenteringPregnancy program. Jennifer McMenaminHollis is leading three of the cohorts. She conducts the 10 interactive group discussions that focus on different topics each session. The first one covers the typical discomforts of pregnancy, prenatal testing, what drugs are safe to
use while pregnant and what drugs aren't. The second delves into nutrition and includes a healthy cooking demonstration. Participants are offered free produce delivery from a Mercy partner called Hungry Harvest, a benefit that's available through their 36th week.
That's just one of the wraparound services participants are offered. Another is free Uber service to and from the sessions. They also can get referrals to agencies that address other needs such as child care and mental health.
Empowerment, connection
Christina Albo is the adviser from the Centering Healthcare Institute who is working with Mercy to develop its CenteringPregnancy model. She says the model's success requires a
systemic shift within organizations away from a one-on-one model to the group care model.
Albo helps organizations set up the steering committees for Centering-Pregnancy, figure out billing and medical coding and plan how to recruit and retain patients.
"For the sites that engage in the Centering implementation plan, we meet on a regular basis and I provide that advisory kind of perspective, answering any questions that they might have," she says. "I'll also work with anybody within their
system that needs a little extra orientation or practice around what the model of care is."
The benefits of CenteringPregnancy's evidence-based model are vast, Albo says. In addition to having regular access to their care providers, the participants discuss issues like what it means to be safe and healthy during pregnancy and
how to a speak up for themselves with care providers. They also get a chance to develop a network of support with other expectant mothers from their community.
"People come out of it feeling empowered, connected, and with improved health outcomes," Albo says.
 Rebecca Bernadel and her partner, Jabarri Johnson, are taking part in CenteringPregnancy at Mercy Medical Center. Their child is due in August. Bernadel says they both want to be educated on how to advocate for the best maternal care
and on their care options.
Rebecca Bernadel and her partner, Jabarri Johnson, are taking part in CenteringPregnancy at Mercy Medical Center. Their child is due in August. Bernadel says they both want to be educated on how to advocate for the best maternal care
and on their care options.She sees the social aspect of Centering-Pregnancy as particularly important as Americans emerge from the long period of isolation brought on by the pandemic. "I think we're in a unique moment where building connection and community just
feels kind of supremely important," Albo says. "I think that the Centering model really offers that in spades."
'I found somebody'
Quira Carver participated in Mercy's CenteringPregnancy program before she gave birth in January. She says she valued the group interaction, especially as a first-time mom.
"It was very important because a lot of people are going through the same emotions or the same problems," she says. "It helped you understand that you're not the only person going through things or feeling a certain type of way during
your pregnancy."
 Quira Carver was in a CenteringPregnancy cohort at Mercy Medical Center before the birth of her daughter, Cailey, in January. She says the program helps women understand that they aren’t alone in what they are experiencing.
Quira Carver was in a CenteringPregnancy cohort at Mercy Medical Center before the birth of her daughter, Cailey, in January. She says the program helps women understand that they aren’t alone in what they are experiencing.Carver's daughter, Cailey, arrived a little underweight but otherwise healthy.
Hollis says getting expectant mothers to join the CenteringPregnancy program isn't easy, perhaps because the sessions are about two hours long or because the groups meet during traditional working hours. However, the retention rate for
women who have attended a session is about 90%.
She recalls one patient who didn't have much in the way of a personal support system and seemed to be growing increasingly depressed about going it alone. Hollis persuaded her to join the CenteringPregnancy program even though she was
well into her pregnancy.
At the last CenteringPregnancy group meeting the patient attended, she and another expectant mother clicked. Hollis remembers the joy it brought the young woman. "She was like, 'Miss Kia, I found somebody that I can go to and we're planning
on doing walks together when we both have our babies and we're just, you know, trying to be there for each other,'" Hollis says.