By LISA EISENHAUER
Colleagues cheered as Greg Newsham, a registered nurse who specializes in wound and ostomy care, became the first of the frontline workers at Mercy Hospital St. Louis to get a dose of the Pfizer-BioNTech vaccine for COVID-19. Newsham was part of the first phase or "A" group in line to get the vaccine because he has been caring for COVID patients, including during the fall surge when the hospital's daily census included about 100 patients with COVID on an average day.

Members of the news media surround Rachel Shields-Carnley, a registered nurse and manager of the intensive care unit at Ascension St. John Medical Center in Tulsa, Oklahoma, as she receives the COVID-19 vaccine on Dec. 15. The Tulsa Health Department set up a drive-thru site to administer shots to frontline health care workers.
Across the nation, thousands of frontline health care workers like him stepped up to get the first injection of the two-part vaccine on the first day it was available to them. Asked if he had any reservations about taking a vaccine that had gotten expedited approval from federal regulators for experimental use, Newsham said, "None whatsoever."
Staff at Catholic health care systems spent weeks submitting the necessary applications for allotments of the vaccine and putting in place processes for inoculating their workforces. Ministry health systems are hopeful that most employees will get the vaccine and that the inoculation assembly line will go smoothly, as it did on Dec. 14 during the first run at Mercy Hospital.
Workers eager for shots
Steve Frigo, executive director of pharmacy for Mercy Hospital, called the first day a "soft opening" for the COVID vaccination clinic with only a few of the eight stations in use. It was in operation in an auditorium for a few hours that day and the next as a run-through to see if any kinks needed to be worked out. Frigo said there were none as the 975 doses the hospital got in its first shipment began to be dispensed. By the end of the month, the clinic was open from 7 a.m. to 7 p.m. for frontline staff.

Frontline workers at SSM Health DePaul Hospital take a moment to pray before getting their first COVID-19 vaccinations at the suburban St. Louis hospital on Dec. 17.
Frigo was confident the hospital would use up the shipments it expects to get weekly as they come in. The Pfizer vaccine requires a second dose 21 days after the first. "When we started talking about looking for people who wanted to sign up on our first day in our A group, we had an overwhelming number of people who wanted to get in," he said. "It's very exciting to see that."
In the first stage of distribution with vaccine supplies limited, federal guidelines call for the vaccine to go to nurses, doctors, respiratory therapists, housekeepers and other staffers who are providing direct care to COVID patients or potentially exposed to infectious material. First priority is also being given to residents and workers at long-term care facilities, which have been ravaged by COVID and account for a disproportionately high concentration of deaths. The guidelines recommend that the second phase of vaccinations go to "frontline essential workers" such as firefighters and grocery store clerks, and anyone aged 75 or older.

Bartles
As of Jan. 5, there were 17 million doses distributed nationwide and 4.8 million vaccinations given, according to the Centers for Disease Control and Prevention.
At large systems like Providence St. Joseph Health, which operates 51 hospitals in seven Western states, tens of thousands of staffers are eligible to be at the head of the vaccine line. Rebecca Bartles, executive director of system infection prevention, said the system had given more than 50,000 first-round vaccinations by Dec. 30. Bartles said Providence St. Joseph Health was getting its expected allotments of vaccines and able to offer shots to all frontline workers considered at high risk. "Our caregivers have been eager to receive the vaccines," Bartles said. "It's given everyone hope during these trying times."

A clinician at Providence Alaska Medical Center in Anchorage gets a COVID-19 vaccine from a colleague.
As part of the prep work for the vaccine, the system bought commercial-grade ultra-cold freezers needed for long-term storage of Pfizer's vaccine. "They are a hot commodity right now and they're not inexpensive," Bartles said of the appliances.
By mid-December a second vaccine, this one from Moderna, had gotten emergency FDA approval and was being rushed to inoculation sites, including some Providence St. Joseph Health facilities. Moderna's two-dose vaccine does not require super-cold storage temperatures.
State-by-state challenges
Health systems have had to navigate the separate structures each state devised for divvying up their vaccine allocations from the federal government. Bartles said the processes vary vastly by state. "The state-level complexity has really added a lot of flavor to this recipe," Bartles said. "And the fact is that some states are incredibly active and forward-thinking and responsive, and others are on the other side of that, and so it's been just a really trying process."
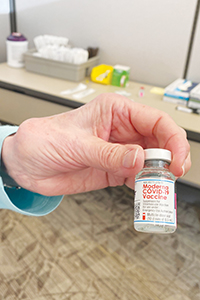
A medical worker holds a vial of the Moderna vaccine, one of two vaccines that federal regulators had approved for COVID-19 as of early January.
Providence St. Joseph Health loosely based its COVID vaccination process for staff on the one it uses for flu vaccines. Associates were being notified when they qualified in the priority roll-out and could proceed to one of the vaccination clinics to get their shot. The vaccines are being tracked in the employee record system.
At its long-term care centers, the system relied on the partnership set up by the Centers for Disease Control and Prevention with Walgreens, CVS and other pharmacies to administer the vaccines.
Planning for quick work
Dr. Sam Bagchi, executive vice president and chief clinical officer at CHRISTUS Health, said the leeway the federal government gave to the states to set up their own distribution processes, while making the process more complex, has had something of a silver lining in that states have been allowed to be innovative.

Bagchi
"It's been good to see different states try different things," he said. "What would be nice to have is a clearinghouse to say, here's the practices that work the best and that's going to become the new national standard. Right now, I don't see that clearinghouse available to share those best practices."
David Benner is vice president of clinical ancillary services for the division of clinical excellence at CHRISTUS Health, which has facilities in Texas, Louisiana and New Mexico. He said the system planned to administer as many doses as possible of the vaccine quickly because that would in part affect how many doses it gets in future weekly allotments.
In a social media post updated on Dec. 31, CHRISTUS Santa Rosa Health System in San Antonio said it was starting to vaccinate people in the "Phase 1B" group. Texas' definition of the group includes those age 65 and older and adults with existing health issues. "However, as our hospitals continue to care for patients with COVID and other medical needs, we are working to turn this process over to specific clinics and outpatient care locations, which are better prepared to provide this type of care to large groups of the public," the post said.
Back at Mercy Hospital St. Louis, part of the four-state Mercy midwestern system, Newsham had a message for colleagues and the public: "Take the vaccination. Let's get this healing process started."