By LIZ GARONE
Caylee Spencer's now 3-year-old daughter suffered a stroke in utero, which left her severely disabled. For Spencer, 26, who lives on the outskirts of Billings, Mont., it has been a long and lonely road navigating the medical landscape and learning just how much mettle it takes to parent a child with special needs.

With support from St. Vincent Healthcare in Billings, Mont., the community's Healthy by Design Coalition produced a video to encourage viewers to take a simple screening that scores exposure to adverse childhood experiences. Unresolved emotional harm from early childhood trauma has been linked to mental health and medical issues later in life. The video is at
https://vimeo.com/204389471.
But she is finding her footing in part through the work she does at weekly therapy sessions at the student-run Walla Walla University Billings Mental Health Clinic. The clinic, which is funded through St. Vincent Healthcare, does not charge for any of its services.
"There's not a lot of support for parents with disabled children in my community," said Spencer. "I can talk to people with neurotypical children until the cows come home, and they just don't get it." She credits therapy with helping her regain some sense of normalcy and control in her life. "I can just talk about what I need to talk about, and it's a relaxing place to do it. There isn't any judgment."
Student counselors
The clinic provides counseling to individuals who do not have health insurance as well as to those who are living below the poverty line. Spencer said she could not afford to pay for the therapy, which is helping her build resilience and coping skills.
Graduate students in Walla Walla University's Master of Social Work program provide the therapy, logging the clinical hours required to complete their degrees, said April Keippel, St. Vincent Healthcare's mission and community benefit program manager. In 2017, the clinic provided mental health services to 158 people who didn't have insurance coverage, 76 percent of whom were living below the poverty line.

Keippel
The clinic "not only addresses the immediate needs of vulnerable individuals for therapy, but also builds capacity in our community by training mental health providers," Keippel said. "The students gain valuable hands-on experience while serving community members in need of mental health care and removing any financial barriers" that prevent patients from accessing care.
Trauma focus
When the clinic opened in March 2015, it was funded through a three-year federal grant supporting development of systems for trauma response education. The grant was received and administered by the St. Vincent Healthcare Foundation on behalf of several area health care and social services providers. The grant money also supported St. Vincent Healthcare in the development of a community collaborative approach to address the National Center for Trauma-Informed Care's three Rs of care: realize, recognize, and respond, according to Keippel. Woven throughout the collaborative's work is the fourth R of resist re-traumatization, she said.
Trauma-informed care has been gaining traction in the U.S. for about 10 years. That is because the seminal Adverse Childhood Experiences Study, known as ACE, established that exposure to trauma and violence in childhood are strongly related to risk factors for disease and mental illness in adolescents and adults.
The ongoing longitudinal ACE study, which began in the mid-1990s, is a collaboration between the Centers for Disease Control and Prevention and Kaiser Permanente, a health maintenance organization whose patients are the study subjects. Many researchers have used the data set to study the impact of adverse childhood experiences on aspects of social, physical and emotional well-being. Their findings are behind efforts to identify people whose childhoods put them at increased risk of disease as well as efforts to proactively build resilience in children and adults.
Among other adverse impacts, researchers have linked exposure to multiple early traumas to an increased risk for substance abuse and diseases as varied as obesity, diabetes, cancer, heart failure and asthma.
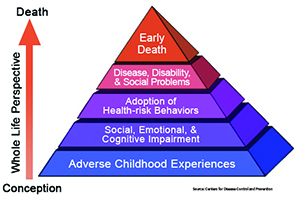
The ACE Pyramid illustrates the conceptual framework for the ongoing Adverse Childhood Experiences Study, known as ACE. A collaboration between the Centers for Disease Control and Prevention and Kaiser Permanente, the longitudinal study established that childhood trauma raises the risk factors for disease and can harm well-being throughout life.
Awareness-building
"Knowing the connection between adverse childhood experiences and a number of health issues, it's important that we address these issues across the community," said Keippel. As part of the grant, 14 local organizations, including the Friendship House of Christian Service, the YWCA Billings, and Big Brothers Big Sisters of Yellowstone County, received training and organizational assessments around trauma-informed care.
"I think having organizations aware of the impact of trauma and having skills to avoid re-traumatization of community members with trauma is important. Also important is being able to provide mental health resources to address trauma and build resiliency for those community members, such as the Walla Walla mental health clinic," Keippel said.
The partnership with the university's social work school has allowed St. Vincent Healthcare to address mental health needs in Billings and meet its mission to serve the most vulnerable in the community, said Keippel. When the federal grant funding ended in September of 2017, some of the collaborative's services, including those provided by the clinic, were put in limbo. St. Vincent Healthcare stepped up with most of the funding to keep the free clinic open. The operating budget is augmented by a state grant and donations. St. Vincent also is paying for the ongoing trauma-informed care training, according to Keippel.
In addition to the training, the collaborative has used social marketing to increase public awareness and motivate individuals to learn their ACE score so that they might actively mitigate potential health risks, said Keippel.
ACE score
Every person seeking care at the mental health clinic is asked to fill out an assessment survey with 10 yes-or-no questions about childhood exposure to trauma. The instrument includes questions about whether a household member was incarcerated or had mental illness, and whether there was domestic violence including child abuse, and alcohol or substance abuse in the household.
The higher the ACE score, the higher the risk for health and social problems. For example, when a respondent ticks the yes box on four or more survey questions, the risk of chronic pulmonary lung disease increases 390 percent; hepatitis, 240 percent; depression, 460 percent; and attempted suicide, 1,220 percent, according to the original ACE study, which was published in 1998.

Perry
Extended reach
Pamela Bing Perry, an assistant professor of social work at Walla Walla University came up with the idea for the free mental health clinic. Without the clinic, many people in the area would not have access to mental health services, she said. The clinic extends its geographic reach by providing tele-mental health services for clients living in more rural parts of the state.
She said the clinic trains clinicians "to come from a trauma-informed perspective, which helps to further broaden the infrastructure of care for our community."
Client Spencer has been impressed with the quality of the care she has received from the students over the two years she has been attending weekly sessions at the clinic. "They are very compassionate," she said. "They are not trying to fix you. They are trying to understand what you are going through and to find a way to help you."
Copyright © 2018 by the Catholic Health Association
of the United States
For reprint permission, contact Betty Crosby or call (314) 253-3490.