A prediction that providers would begin to see more uninsured patients with the end of the pandemic-era continuous coverage requirement for Medicaid appears to be proving correct.
Researchers who are tracking the Medicaid unwinding report that millions of people have been dropped from the rolls, which they projected before the process began last year. Meanwhile, the leader of a Catholic health system says more uninsured patients are coming in for care.
Unwinding is the term used by the Centers for Medicare & Medicaid Services to describe the process the agency gave states 14 months to complete to redetermine the eligibility of all Medicaid and Children's Health Insurance Program enrollees. Both federal programs are administered by states.
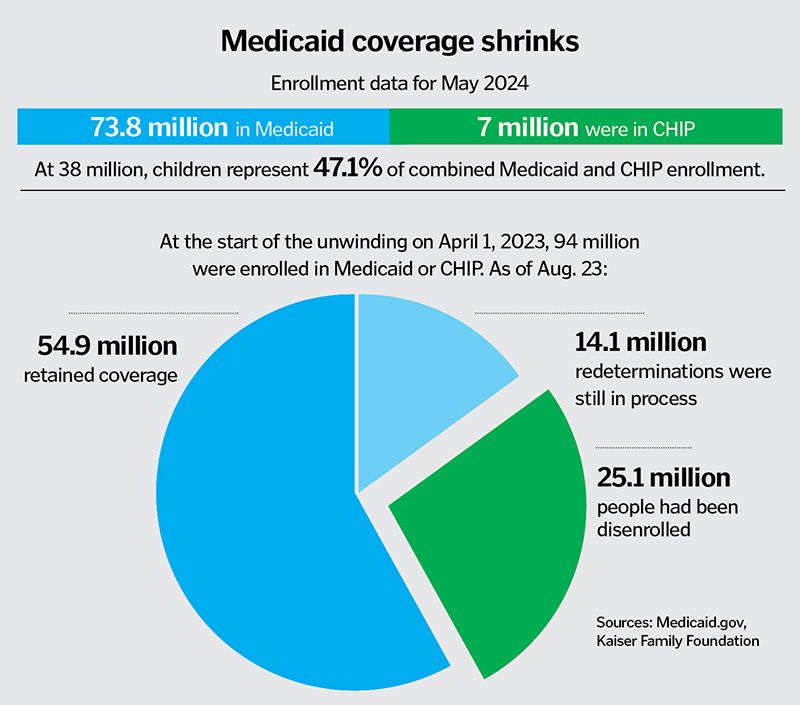
During the COVID-19 pandemic, when enrollment for the two programs hit a record of 94 million, a federal provision gave states a boost in funding in return for locking in coverage. That provision lapsed on April 1, 2023, and states could immediately begin determining who was still eligible based on income and family size.

Tricia Brooks, a research professor at the Georgetown University McCourt School of Public Policy's Center for Children and Families, is among those closely watching as states report their unwinding statistics. With the process nearly complete, tallies indicate that as of Aug. 1, the rolls had shrunk by about 25 million, or about 26%.
Brooks expects it to take another year before clear data is available so she and other researchers can tell how many of those who left the Medicaid and CHIP rolls moved to private insurance or to low-cost options in the health insurance marketplace set up under the Affordable Care Act. She's certain, however, that some of those who were disenrolled fell through the cracks in the redetermination process and lost coverage despite remaining eligible.
"Some of these people are not going to be gaining other insurance," Brooks says. "There's no question that some are going to be uninsured."
Trinity Health impact
The Congressional Budget Office estimated in June that the share of Americans without insurance reached an all-time low last year, at 7.2%. The nonpartisan office projects that by 2034 that rate will hit 8.9%,
as policies put in place during the pandemic expire.

Mike Slubowski, president and CEO of Trinity Health, says his system already is seeing the effects of the unwinding and evidence that more people are ending up without any health insurance. Of the 30 million patients across Trinity Health's 26-state footprint, the percentage who have no coverage has grown by about a third, to 2.2%, since the nationwide review of Medicaid eligibility started last year. That translates to about 220,000 more uninsured patients and an estimated revenue loss to Trinity Health of about $27 million for the fiscal year that ended June 30 from treating so many more patients who are uninsured rather than covered by Medicaid.
In preparation for the unwinding, Trinity Health took proactive steps to educate its providers and patients about the potential loss of Medicaid and CHIP eligibility. That effort included sending more than 200,000 letters to inform patients of redetermination rules, which varied from state to state, and training the system's financial counselors to help patients who lost coverage explore other health insurance options.
"We think that if we had not developed some of the educational partnerships we did and our active financial counseling, it would have likely been much higher in terms of the percent of uninsured," Slubowski says.
Renewal process varied
Brooks notes that some states made the redetermination process fairly simple, including by using ex parte renewals. In ex parte renewals, states look at financial data already on the record for families, such
as from applications for federal food assistance programs, to determine Medicaid eligibility. Other states made the process much more challenging, such as by requiring enrollees to submit tax documents and other paperwork to confirm they meet eligibility
requirements.
Federal data show that for May there were 6.2 million Medicaid or CHIP enrollees whose coverage was up for review. Of them, 67.7% were renewed and three-fourths of the renewals were through an ex parte process. Of those who lost coverage, in 63.5% of cases the loss was "for a procedural or administrative reason."
The Kaiser Family Foundation notes on its website that's tracking the unwinding: "High procedural disenrollment rates are concerning because many people who are disenrolled for these paperwork reasons may still be eligible for Medicaid coverage."
CHA toolkit
In advance of the unwinding, CHA created a toolkit called Protect What's Precious as part of its Medicaid Makes It Possible campaign. The resources in the toolkit can help guide patients through eligibility redeterminations. The free resources can be downloaded and rebranded or co-branded by CHA members.

Paulo Pontemayor, senior director of governmental relations at CHA, says that, even as the Medicaid unwinding nears its end, those resources remain relevant to help patients understand how they can regain eligibility or apply for other assistance.
Pontemayor says CHA continues to advocate for policies that support and boost Medicaid, including by encouraging policymakers to approve continuous coverage rules. Such rules are already in place in most states for children enrolled in Medicaid or CHIP, ensuring that they have coverage for at least a year upon meeting eligibility requirements.
"We were grateful for Congress and the administration's work to make continuous eligibility for children a reality, and now let's work to make it so that adults can also have continuous eligibility," Pontemayor says.
Coalition formed
Earlier this year, CHA joined 25 other organizations in the Connecting to Coverage Coalition. The coalition
is focused on minimizing the disruptions from the unwinding and smoothing the transition to other forms of insurance for those moved off Medicaid rolls.
Executive Director Catherine Finley says the coalition is using its website as a clearinghouse of information for and from members about the impacts of the unwinding and potential responses. The organization also advocates for policies that make health insurance accessible. In addition, it is working to develop ties between coalition members and federal and state officials whose decisions affect insurance access.
"We really, as a coalition, want to see people get the insurance that they're eligible for and that works for their families," Finley says.
'The right thing to do'
If the goal of the unwinding was to see that those who remained eligible for Medicaid kept their coverage and those who weren't got connected to other forms of health insurance, Finley doesn't think
the process could be called successful. That's because it's apparent that many people who should have stayed on the rolls got removed, she says.
Nevertheless, Finley says there were some successes within the process, such as a greatly expanded use of ex parte renewals. A recommendation that CMS streamline the use of ex parte renewals is among many the coalition makes for improving the efficiency and accuracy of Medicaid and CHIP eligibility redeterminations in a policy paper it published in June.
Slubowski says getting patients coverage through Medicaid, private insurance or one of the federal marketplace plans is critical for health care providers, especially Catholic providers such as Trinity Health that turn no one away. "If we can get some form of coverage, we can still live out our mission of care for those living in poverty, which is the right thing to do," he says.
