BY: JADE GONG, MBA, RN, and ANNE LEWIS, MA
The Program of All-Inclusive Care for the Elderly, better known as PACE, is a program under Medicare and Medicaid that can honor an elderly individual's desire to be cared for at home and in his or her community for as long as possible rather than in a nursing home setting. PACE enrollees receive comprehensive medical care and social services in day centers, in the community and at home via an interdisciplinary team of health professionals.
Beneficiaries, caregivers, providers and policymakers long have regarded PACE as the gold standard of integrated care for the most vulnerable adults. The model fully captures the Triple Aim and improves quality, reduces costs and improves the patient experience.
Trinity Health, headquartered in Livonia, Michigan, was one of the earliest adopters of PACE and today is the largest sponsor of PACE programs in the United States. Viewed through the lens of Catholic health care, PACE is a unique, mission-driven strategy for improving the care provided to a specific population that is growing in size, uses a tremendous share of the nation's health care dollars but has unmet needs. Trinity Health, which currently operates 11 programs in eight states, regards PACE as an expression of its Catholic values and health care ministry. The system is actively expanding PACE across the nation as the foundation of a person-centered health system that, along with traditional long-term care facilities, is an essential part of the continuum of care in each community it serves.
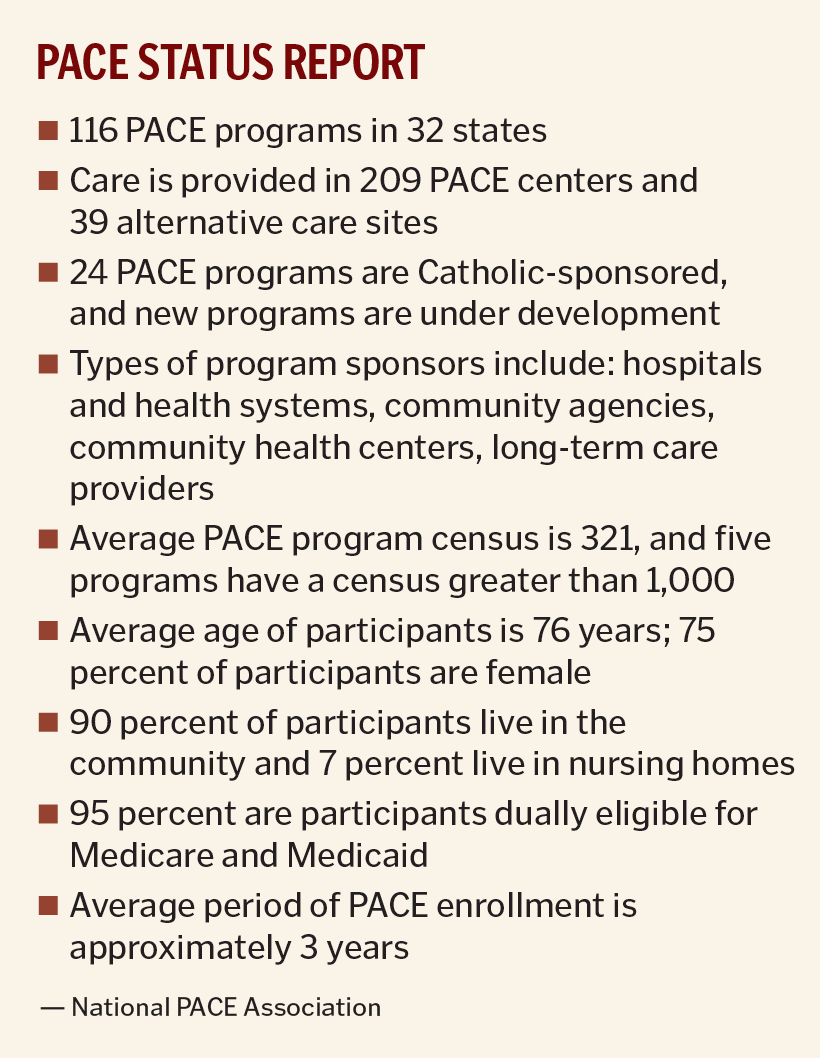
PACE began as a demonstration program in 1983 and proved successful. In 1997 the U. S. Congress authorized a permanent program. Operating under the current federal statute and federal and state regulations, the PACE community has grown to encompass 116 programs serving approximately 35,000 enrollees in 32 states.
In 2016, PACE leaders are looking forward to new opportunities to serve expanded populations with a more flexible model as a result of the 2015 PACE Innovation Act. In addition, PACE leaders also are expecting an updated federal regulation in 2016 that will offer greater flexibility in adapting to the current operational realities to reduce costs and improve outcomes.
PACE TODAY
A PACE program is a fully integrated provider of care for those who are among the frailest members of society and whose care is among the costliest. According to current statute, PACE programs enroll only individuals who are:
- At least 55 years of age
- Living in a PACE service area
- Certified by their state as needing nursing facility care
- Able to live — with PACE services — safely in the community at the time of enrollment
Most PACE participants are eligible for Medicare, Medicaid or both. The program is voluntary and the participant can leave at any time. Once someone is enrolled, a PACE program provides for the entire continuum of Medicare and Medicaid services by means of a team that includes a primary care physician, registered nurse, master's level social worker, dietician, PACE center manager, home care coordinator and personal care attendants, among others. The team tailors services to the individual with a focus on providing long-term support in a community-based setting — generally at a local day facility called the PACE center.
The heart of PACE — and the key to its success — is the interdisciplinary team that knows the patient and family and is responsible for the patient's care on a 24/7 basis. By design, the PACE program's person-centered care has great flexibility to meet individual needs, enabling programs to achieve Triple Aim goals including improved patient experience of care.
CONSTRAINTS AND OPPORTUNITIES
PACE was the first fully integrated and capitated provider of care for persons who are frail enough to be admitted to a nursing home. Initially, nursing homes and home- and community-based waiver programs offered alternatives to PACE in most communities. Since that time, though, new models of care — including managed care plans for persons eligible for both Medicare and Medicaid, Medicare Accountable Care Organizations (ACOs) and others — also have emerged to serve the same type of patients.
Despite recognition of the model's success, PACE programs have grown incrementally and care for only a fraction of their potential population. More substantial expansion has generally been limited by factors that include state policy as well as Centers for Medicare and Medicaid Services statutory and regulatory requirements to serve only persons who are nursing home eligible, to operate an adult day care center, to maintain a substantial interdisciplinary team, to complete a lengthy and complex application process and to apply for waivers from prescriptive regulations and protocols. The National PACE Association has estimated that if PACE programs could access half of the eligible population in the nation and achieve the level of enrollment of successful programs that are now operating, then PACE would serve approximately 182,000 enrollees.
CMS already has offered some flexibility in providing care in locations other than a PACE center to reduce facility opening and operating costs. It is hoped that a new regulation will provide even more operational flexibility to support expansion and allow PACE programs to operate more competitively in the post-health care reform marketplace.
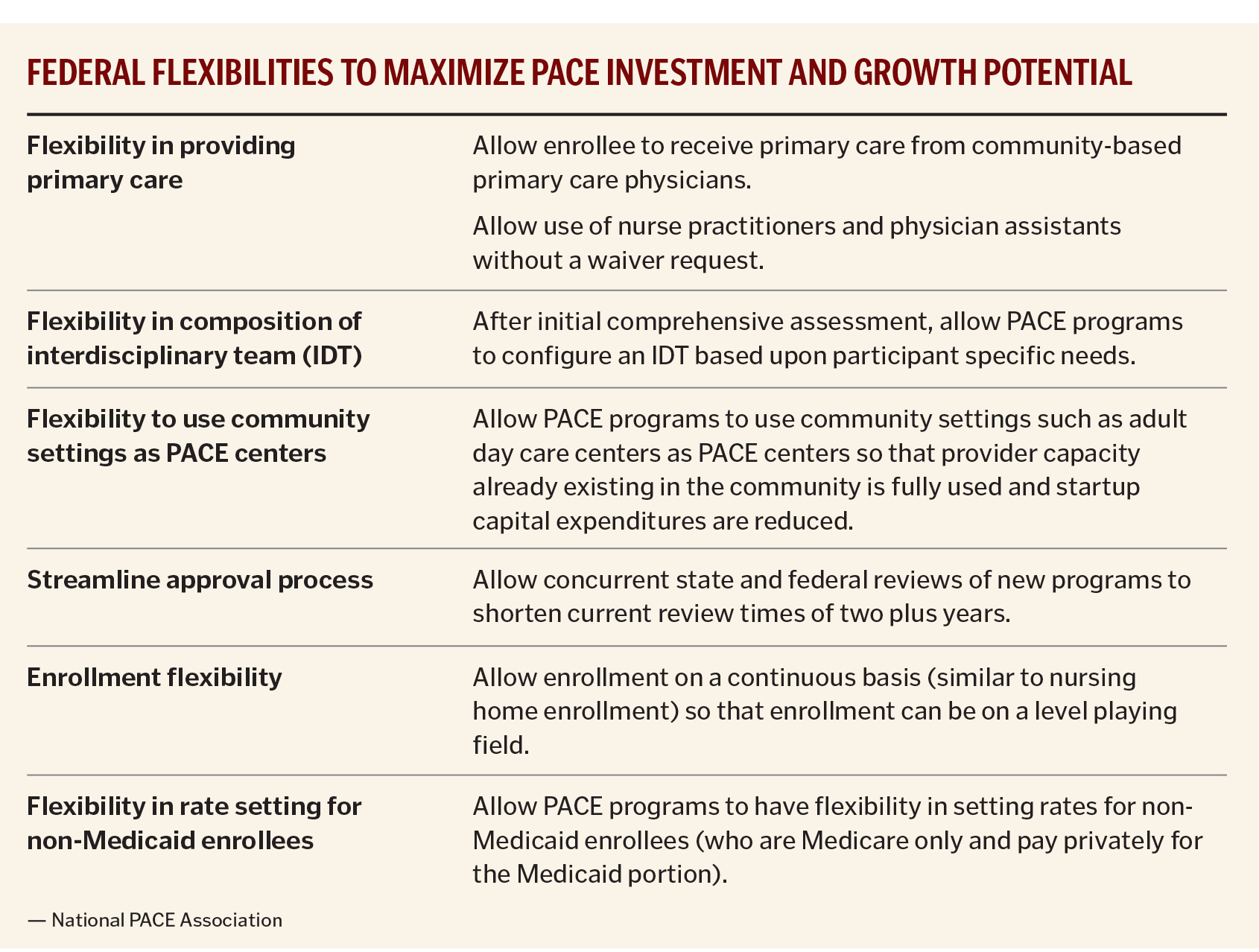
PACE providers seek a range of policies to allow programs more freedom to tailor care to individual needs, as noted in the chart on page 63.
PACE OF THE FUTURE
The PACE Innovation Act became law on Nov. 6, 2015, and PACE leaders are waiting to learn if CMS will use this new statutory authority to expand the reach of PACE to serve new populations in innovative ways. Using the CMS Innovation Center's approach in implementing and adapting other new models of care, PACE could be made scalable and reach the high-cost and high-need populations that require the most coordination and assistance. The new law gives CMS the ability to expand a proven model of care to serve new populations that are not now eligible for PACE — but the agency is not required to do so.
To date, the PACE community has been most interested in ways to adapt the model to serve (1) persons under age 55 who have disabilities and (2) persons who are over age 55 but who are not yet nursing-home eligible (the so called pre-nursing-home eligibles). Another population of interest is persons who are currently Medicare-eligible but not yet Medicaid eligible and who could benefit from the care coordination provided by the PACE model. This care could help slow the rate of an enrollee's health decline and reduce future Medicaid spending.
While there are some successes arising from the managed care pilots that are underway, early results from CMS demonstrations have shown the health care community that turning over the care of the most vulnerable elders to large managed care plans will not provide an easy solution for all patients and all communities. PACE programs know that building a person-centered health care system for frail elders occurs one patient and one family at a time and balances the need to deliver patient-centered care with the desire for scale. Experience has shown that managed care plans must intentionally create caring relationships with each individual and family in order to achieve the desired levels of quality and success that PACE has achieved.
 CATHOLIC MISSION AND VALUES
CATHOLIC MISSION AND VALUES
Trinity Health's commitment to PACE program growth in 2016 and 2017 is helping to fulfill its mission, vision and strategic plan. The system plans to open two more programs, bringing the total number of its PACE programs to 13 in 9 states, and it is evaluating the opportunities that may arise from the PACE Innovation Act.
As a population health model that honors the wishes of each individual and family, PACE actualizes Trinity Health's vision of becoming a people-centered health system offering outstanding care in each community. Trinity Health's strategic plan calls for expanding PACE in as many communities and states as can support PACE expansion, through aggressive enrollment growth, new startups and acquisitions. In existing programs, growth will occur through development of alternative care sites and new PACE centers.
Just as Trinity Health has concluded that PACE programs are a fruitful, people-centered strategy, other Catholic health systems also may see PACE as a natural fit with mission-driven goals to extend their ministries to serve vulnerable populations and community health needs. With the sponsorship of Catholic health systems, PACE may finally be able to reach its potential enrollment to the benefit of the elderly beneficiaries the program is designed to serve.
JADE GONG is principal of Jade Gong and Associates, Arlington, Virginia, and a strategic adviser to PACE programs nationwide.
ANNE LEWIS is vice president of strategy and development with Trinity Health PACE in Livonia, Michigan.