BY: CHRIS ALLEN, MHSA, FACHE
Leaders in Catholic health care should point the way forward in how to best use community benefit dollars to improve the wellness and health of populations. Are we up for the challenge? I ask that because the change will be very uncomfortable to many in our health ministry. Today, hospitals and health systems often operate in siloes — though there are some exceptions — supporting community projects specific to their patient populations while fulfilling the community health needs assessment required by the Affordable Care Act. However, a hospital's community health projects often aren't large enough in scope and scale to make a meaningful change in improving a population's health. Because of this, leadership from religious congregations, health system/hospital sponsorship, governance and administrative executives need to view the use of community benefit dollars through a new lens.
The current model of care and the associated reimbursement do not encourage people to be well and healthy. Millions of dollars are spent annually in the community health benefit area with very little impact on a population's morbidity and mortality, its illnesses and deaths. Kevin Barnett, DrPH, a senior investigator at the California Public Health Institute, has led research and fieldwork in hospital community benefit suggesting that change is necessary to fulfill a hospital's or health system's community benefit responsibility. Viewing health care through a new lens of population health is a heavy lift and transformation requires a significant shift in thinking. The approach will take courage and new skills from those in governance and management.
I am reminded of one of Martin Luther King Jr.'s quotes, "Courage is an inner resolution to go forward despite obstacles; cowardice is submissive surrender to circumstances. Courage breeds creativity; cowardice represses fear and is mastered by it. Cowardice asks the question, is it safe? Expediency asks the question, is it polite? Vanity asks the question, is it popular? But conscience asks the question, is it right? And there comes a time when we must take a position that is neither safe, nor politic, nor popular, but one must take it because it is right."
Applying this quote in the context of population health conjures up a different meaning based on one's role in the current health care environment. My lens is based on 20 years in hospital management and 20 years working on issues related to community social determinants and equity. In the last 14 years, I have been president and chief executive officer of Detroit-based Authority Health, a public-private population health organization in Detroit that works to create a stronger safety net for vulnerable populations. In April, I retired from that position. In governance roles, I chair the newly formed Bon Secours Mercy Health Board of Directors in Cincinnati, following the recent merger of two Catholic health care systems, Bon Secours Health System and Mercy Health. Previously, I was the former board chair of the Bon Secours Health System. This diverse professional experience informs my opinion on where hospital and health systems are headed in the population health environment.
I subscribe to the definition of population health by David Kindig, MD, PhD, and Greg Stoddart, PhD, who published it in 2003. Their definition describes population health as "the health outcome of a group of individuals, including the distribution of such outcomes within the group."1 In an online article published in April 2015, staff from the master's in health administration program at The George Washington University suggested that health care executives and providers they asked had somewhat different opinions on the definition, with many viewing it as "an opportunity for health care systems, agencies and organizations to work together in order to improve the health outcomes of the communities they serve." The writers of the article noted, "While we may not have reached a universal consensus on what ‘population health' means, we discovered that now is the time to think differently — not only about the definition of population health — but also about the way health care is delivered. In our ever-changing health care environment, perhaps the ‘traditional way' may not be the right answer."2
What is clear is that the use of community benefit dollars is falling short of the intended purpose and health care systems and their partners aren't moving a population health metric in a positive direction fast enough. That has become evident since health care organizations started to utilize the Robert Wood Johnson Foundation/University of Wisconsin County Health Rankings data in their strategic planning initiatives earlier in this decade.3 When that happens, analysis of the data begins to open the eyes of those working on strategy and care providers about the enormity of the task and how little change has occurred. An example is the use of morbidity and mortality data by county. For the last 10 years, nearly every county in the United States has been ranked. Among the many findings, one analysis centered on a chart that highlighted the factors that impact a person's health.
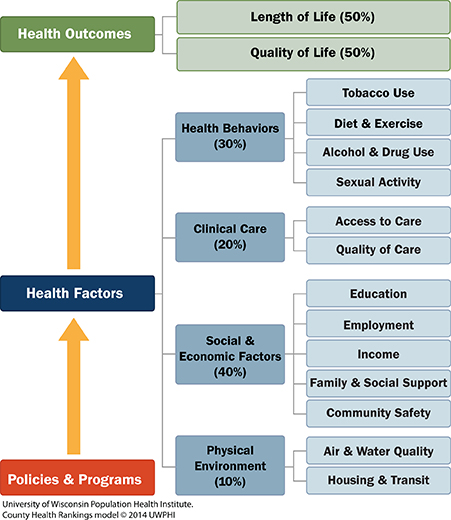
The County Health Rankings model measures health outcomes by length of life and quality of life. This graph illustrates that 80% of the relative contribution of modifiable factors influencing morbidity and mortality include: health behaviors at 30%; social and economic factors at 40%; and the physical environment at 10%. Compared to these other factors, clinical care contributes only 20% to a community's length and quality of life. However, the current health care system spends about 90% of our time in the clinical care area trying to change a health outcome of the communities we serve with very little or no success. True population health measures such as the rankings can provide a baseline for all community benefit planning. An analysis of the Bon Secours markets in 2016 utilized the rankings data and applied it to its community benefit settings.
As past chair of the Bon Secours Health System, I encouraged and witnessed Rich Statuto, the former president and chief executive officer, and Sr. Pat Eck, CBS, chair of Bon Secours Ministries, take a bold step in evaluating morbidity and mortality in each one of Bon Secours' health system markets in seven states utilizing the Robert Wood Johnson County Health Ranking data by the Bon Secours leadership team, with an "A" being the highest and "F" being the lowest score.
The information was presented at a strategic planning retreat for the Bon Secours Health System board, the local market boards and their leadership teams. Following the presentation, a sobering discussion occurred among the health care system's leaders including sponsors, governance executives and others, which resulted in a new way of understanding why, and the importance of collaborating with other organizations to achieve improvements in health and wellness. The following year, Bon Secours Health System took another bold step by inviting community partners, one from each market, to attend the all-system board strategic planning retreat. The hope from that meeting was that, over time, collaboration will make a difference and a move toward a holistic way of measuring results. Participants said another take-away was to leave each organizational ego at the door and to leverage organizations' specific resources to make positive, market-specific improvement. Collaboration continues to improve at the local market level between Bon Secours facilities and other community-based organizations working on issues related to social determinants of health. An excellent example of such collaboration is in West Baltimore.
As the new chair of Bon Secours Mercy Health, I was delighted with the oversight committee discussion on how the new health care system would utilize $640 million a year in community benefit funds across 45 markets to continue to create, support and expand a population health model of wellness. In each one of our markets, we're asking: how can Bon Secours Mercy Health be a catalyst among many organizations around a few key social determinants to drive change? This initiative can be accomplished while honoring our mission "to extend the compassionate ministry of Jesus by improving the health and well-being of our communities and bring good help to those in need, especially people who are poor, dying and underserved."
In a joint meeting in December 2018 of Bon Secours Mercy Ministries and the Bon Secours Mercy Health Board, Sr. Doris Gottemoeller, RSM, PhD, Sr. Pat Eck and Sr. Carol Anne Smith, HM, gave stirring presentations about the courage of religious women in the 1800s. From humble beginnings and a calling to religious life, those women created their congregations on whose shoulders we stand today. It is that same courage that we need to call upon — demonstrating our history, our mission and our values in our world today — as we move Catholic health care to the forefront of those working to improve health with new approaches.
As an example, one regional population health initiative in Detroit gives some evidence of possibilities and setbacks on these types of collaborations. In 2015, Authority Health convened an initiative called the Detroit Regional Health Collaborative to utilize a population health approach, including hospital and health system data on use of health care services and local sociodemographic data for regional health improvement.
The collaborative had two broad objectives:
- To develop consensus around the process (framework, models, best practices) best suited toward collaborative population health; and
- To support an initial approach to assessing the region's health collectively, with an emphasis on supporting members' efforts regarding community and/or population health improvement initiatives.
As a neutral organization, Authority Health asked for all hospitals, health systems, health departments, federally qualified health centers and free clinics in the region to share data around their individual community health needs assessments. A requirement of the Affordable Care Act is a three-year community health needs assessment in each of the hospital markets. I asked the directors of the Wayne County Health Department and the Macomb County Health Department to co-chair the group. Each hospital organization shared its initial assessments and the results were collated.
The data suggest, because of the competitive nature of the hospitals in Detroit, their service areas often overlapped. Consequently, the same information was gathered and reported separately five times to the IRS. (For more information, see the Regional Community Health Assessment study at authorityhealth.org.) What happened next in the collaboration process surprised me. For almost a year, there were positive meetings with full engagement among hospital departments that were assigned community outreach or responsible for the community health needs analysis. At the time of the final vote to accept a single, regional community health needs assessment analysis and agree on a few social determinants that would be targeted by the group, three hospital participants and health systems moved away from the table. It was later revealed that there was concern about the future of their hospital community outreach departments and employee job security if they fully engaged in a regional approach. It is my opinion that their role and responsibilities would have been enhanced and truly valued with more regional collaboration, rather than threatened.
Using the County Health Ranking data, there are 83 counties in Michigan with Wayne County, where Detroit is located, being the largest. With all the health care resources available to area residents, including top hospitals, physicians and one of the largest medical schools in the United States, Wayne County hovers near the bottom of all 83 counties in Michigan when measured against morbidity and mortality in the 2019 rankings. Specifically, its health factors rank lowest in the state at 83, its health outcomes rank 82, and length of life ranks 80 in the most recent data online. Likewise, when community benefit dollars were collated by Authority Health staff, we learned that close to $500 million was used in Detroit in 2015. The information suggests that change and greater work together is necessary in the way we address the health of our communities.
Yet, one of the Catholic health systems involved in the regional community needs assessment called other hospital colleagues to encourage active participation with no avail. One CEO said with embarrassment that "his organization over 20 years allocated $150 million in community benefit dollars a mile long and only an inch thick, with no tangible evidence of population health improvement."
The data also suggest that the projects supported by hospitals and health systems aren't large enough to move a population health metric. No single hospital or health system is going to move a population health metric. The population health improvement must be in collaboration with many and different organizations to positively impact a social determinant.
In our Catholic health ministries, we can be the change, but it starts with each one of us. In reflection on the opening quote by Martin Luther King Jr., the courage to go forward despite the obstacles is necessary. We must not let our fear master us, but must let our courage guide us toward solutions.
CHRIS ALLEN is chair of Cincinnati-based Bon Secours Mercy Health, a board member of the Catholic Foundation of Michigan and a past chair of the Catholic Medical Mission Board.
NOTES
- David Kindig and Greg Stoddart, "What Is Population Health?," American Journal of Public Health 93, no. 3 (March 1, 2003): 380-83, https://doi.org/10.2105/AJPH.93.3.380.
- "What Is Population Health?" by the staff of MHA@GW, The George Washington University, Milken Institute School of Public Health, April 27, 2015, https://mha.gwu.edu/what-is-population-health/.
- 3. More information about the County Health Rankings & Roadmaps program: https://www.countyhealthrankings.org/.