BY: CLARE WILLRODT
"Geography shouldn't be a determining factor of how good [is the] care you get," said Dr. Jill Kruse, a physician at Bon Homme Family Practice Clinic Avera, located in Tyndall, S.D. Tyndall is a town of approximately 1,250 residents in a county with a population density of 13 people per square mile, and Kruse's is typical of rural practices around the United States. There are many weekdays when she is the only provider in the clinic — and many weekends when she is the only health care provider in town.
"In rural medicine, you are often the first, last and only line of defense, and sometimes it feels very lonely," Kruse explained. She called "invaluable" the backup she gets from a unique two-way telemedicine platform developed by Avera Health, based in Sioux Falls, S.D.: "At the push of a button, I can talk to someone else who has excellent resources.
"Before the system became available, I would see an ambulance rush by my house hard and fast, and I would think, 'I better get in right now!' I was never completely off call," she recalled. "This has taken some of the burden off, because it means there is a physician available immediately."
FACING SHORTAGES
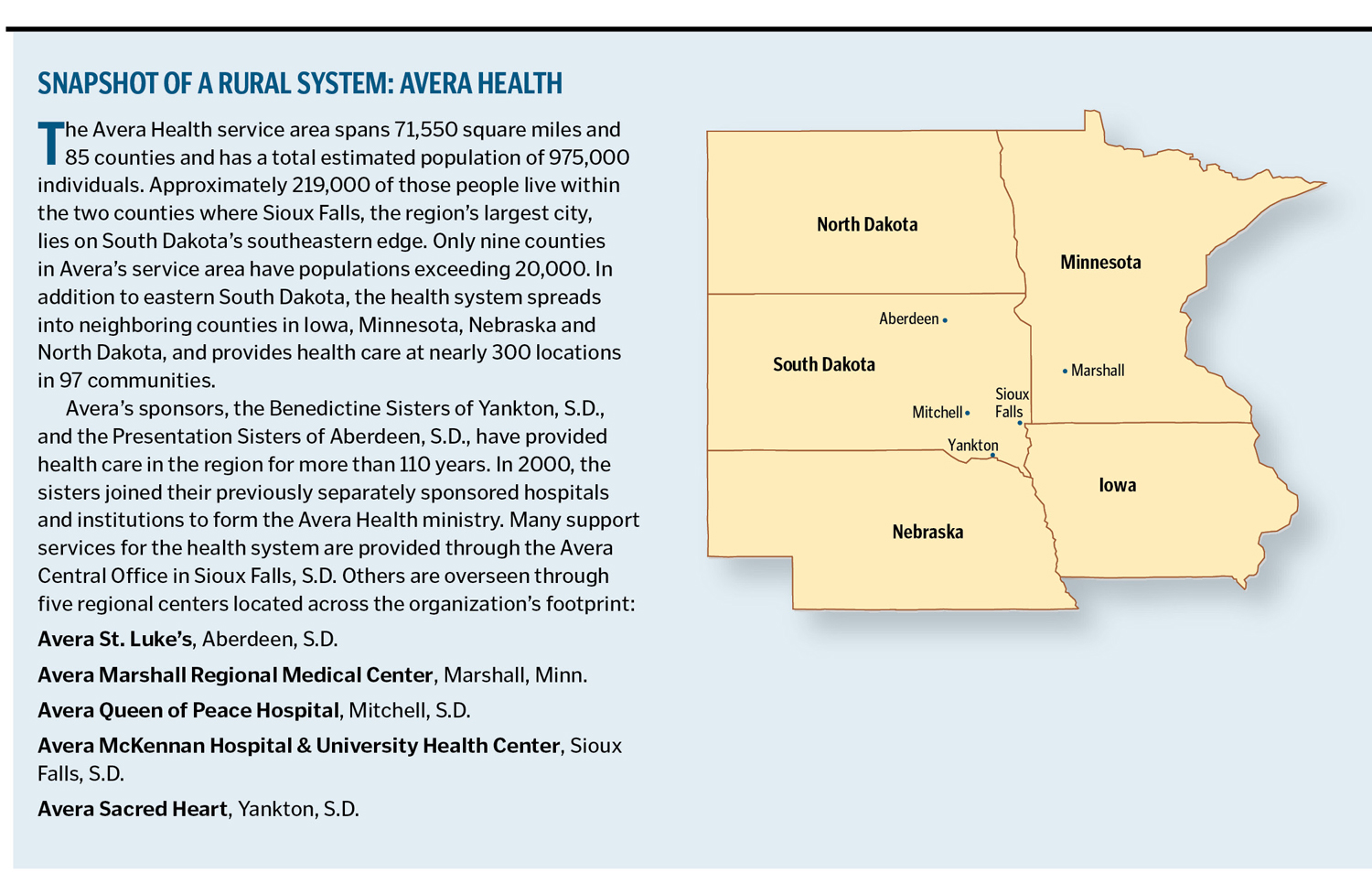
According to the U.S. Census Bureau, the region served by Avera Health has somewhere between 200 and 250 physicians per 100,000 population, one of the lowest rates in the nation. Recruitment and retention of rural physicians have never been easy. Many rural physicians are the sole providers in their communities, which means longer hours and much less time off than their urban counterparts have. Today, as the baby-boomer generation ages and requires greater care, and physicians currently practicing reach retirement age, studies by medical groups indicate that the U.S. will need as many as 200,000 more physicians by 2020. Rural areas can expect to face even greater challenges contending with shortages.
INVOLVING THE GREATER COMMUNITY
Avera has been nationally recognized as a model for rural health care delivery and sustainability of the rural health care workforce. The system has developed a program of effective recruitment-and-retention measures, but overall, community involvement is key, said David Flicek, senior vice president of Avera Medical Group.
"Our rural communities have groups representing multiple points of interest who gather regularly, and everyone knows the plan," he said. "These are representatives from schools, businesses, service organizations and virtually every aspect of community life. The vitality of the community hospital is directly related to the viability of the community, so people in a rural community are quite invested."
The community group makes phone calls and is present to "meet and greet" when candidates and their families come to town. This community base can be powerful at the rural level, especially if a medical student has family ties to the area.
It is also crucial to involve other physicians in community-organized recruitment. "It is much easier to recruit if you have agreement about what is needed from the other providers in the community and if you present a cohesive approach," said Doug Ekeren, vice president of planning and development at Avera Sacred Heart in Yankton, S.D.
"Candidates do call physicians to learn about medical practice in the community, and you want that conversation to support your effort," he said.
In addition, local physicians send brief personal letters to medical students and residents Avera is interested in recruiting. Hearing about a practice and community firsthand from a physician who works and lives there has tremendous credibility.
In fact, when it is done well, a community's role in attracting candidates to a rural practice is hard to beat, according to Risë Waldera, director of physician recruitment at Avera Queen of Peace Hospital, Mitchell, S.D. "The whole community is like a family and steps up to welcome them," she said. "Physicians can practice wherever they want, but they don't always get the kind of atmosphere and people a smaller, rural hometown offers."
IDENTIFYING EMERGING TALENT
In 2009, when Avera McKennan in Sioux Falls learned that graduates of a local Catholic high school made up a significant number of first-year medical students at The University of South Dakota, the hospital developed a structured relationship to encourage high-school-age youth to pursue careers in health-care-related fields.
Now in its second year, the program includes job shadowing, internships, career days and more. In March, Avera McKennan hosted 101 students for a two-week career exploration activity in 45 different areas of the hospital with 94 staff mentors. Afterwards, 75 percent of the student participants said the experience influenced their decisions to pursue a health care career, and an equal number indicated they would seek employment at Avera McKennan.
An additional 83 students participated in an evening career-exploration presentation, and some 130 additional students attended a presentation on infection control, HIPAA and confidentiality.
Besides common approaches to support emerging talent, such as tracking students through medical school and residency and providing traditional clinical settings and scholarships, Avera has developed some novel programs that are showing benefits.
Clinical First Steps — an eight-week summer program for students who have completed their first year of medical school.
Students come to Avera McKennan to observe delivery of care, discuss the physician's role in hospital operations and leadership and to explore the clinical practice, economic impact and lifestyle of various specialties. Avera physician recruiters stay in touch with participants over the course of their schooling. Avera McKennan recently hired a physician who participated in the inaugural Clinical First Steps program in 2002.
Yankton Ambulatory Program — part of the Sanford School of Medicine at The University of South Dakota in Vermillion, S.D.
Throughout a yearlong rotation, third-year medical students engage in six disciplines: surgery, obstetrics and gynecology, pediatrics, internal medicine, family medicine and psychiatry. About 60 percent of the rotation takes place in a clinic setting and 40 percent at Avera Sacred Heart Hospital in Yankton, S.D. Unlike traditional eight-week clerkships, medical students are able to follow a patient throughout the entire year.
The program, with its emphasis on rural practice, started in 1991 and draws interest from health care systems around the globe. A former med student in the Yankton rotation, Dr. Michael Pietela now is a program faculty member.
"The longitudinal structure and self-directed course of learning allowed me to focus in areas I was most interested in," Pietela said. "My exposure to mentors with whom I spent the entire 12 months helped me develop similar mentoring and teaching skills that I share with students today."
A measure of success: Of 47 physicians currently practicing in four Yankton-area clinics, 12 went through the Yankton Ambulatory Program. "The Yankton Ambulatory Program is innovative and has become a national model for the primary clinical year of medical education," said Lori Hansen, dean of the program. "It is exciting to see students gain knowledge and skills over the entire year. The relationships that develop with faculty, patients and the community have helped recruit students back to Yankton to practice."
RECRUITING THE PHYSICIAN AND FAMILY
Physician recruiters throughout the system emphasize the importance of building and maintaining relationships with physicians and their families. Karrie Schipper, physician recruiter for Avera McKennan, advised, "Do your homework about a candidate's needs and interests."
"As recruiters we are looking for the right fit, both for the physician as well as the facility," said Schipper, who also has experience as a medical clinic manager. "We start the recruitment process early, connecting with our local medical school graduates and residents who are from the area or have family ties in the area."
Schipper said her department maintains a database of University of South Dakota medical school graduates and where they get their residency/fellowship training. Online physician job banks also help make connections to Avera job opportunities.
Resumes and phone interviews help reveal what a prospect is looking for in a practice opportunity and community, she said, not to mention information about family members.
"Before the physician's on-site visit, we will ask additional questions on personal interests and if they need us to make arrangements for family members during the interview," she said. "We want to accommodate the whole family.
"We are also with the physician when the decision has been made to extend an offer of employment and the contract has been signed," she said. "Our department assists with credentialing and licensing paperwork, coordinating the move and orientating them to the facility and community. The physician recruiters take great pride and care in assisting the physician and their family transition into the perfect opportunity in the perfect community."
Waldera said changing times have brought changing expectations for medical practice. "Call is an issue," said Waldera. "There is a real desire for life balance between career and family, and there is an urban bias because in larger cities there usually are more career, educational and recreational choices for other family members."
"A great deal of our retention focuses on the spouse and community life, on personal and professional life balance as key to happiness here," agreed Ron Jacobson, chief executive officer of Avera St. Luke's in Aberdeen, S.D.
PROVIDING TECHNOLOGY
A suite of technological services may be Avera's most valuable asset when it comes to rural physician recruitment and retention. Today's recruitment candidate wants updated facilities and equipment, the ability to consult with other physicians, reliable emergency room and call coverage and a small practice that includes an experienced physician. On the other hand, candidates dislike practice limitations (such as no obstetrics or pediatric coverage) and handwritten charts.
Avera's technology in emergency departments and intensive care units helps monitor patients, activate emergency transport teams, deliver stroke evaluation and treatment with the help of a neurologist and gives rural practitioners 24-hour access to specialty-care physicians, pharmacists and mental health professionals. The services also include neonatal consultation, electronic records and home care monitors, among other innovations. Physicians and patients who use the services say that when the button is activated to bring the remote physician to the bedside via two-way video, it is just like having another physician in the room, or as one provider stated, "on my shoulder."
SEEKING THE COMMON GOOD
J. Michael Stebbins, Avera's senior vice president of mission services, said this technology model uses centralized expertise to support decentralized care in a way that improves outcomes, supports the workforce and saves the health care system money.
"This strategic innovation to provide care at the local and rural level is really an illustration of Catholic social teaching in action," he noted. "This is what is meant by subsidiarity. Avera has made a conscious decision to support the ongoing health and viability of communities. Catholic social teaching emphasizes the importance of working for the common good and keeping local communities viable."
CLARE WILLRODT is marketing and public relations associate, Avera Health, Sioux Falls, S.D.